Abstract
Purpose: Men have a lower uptake of genetic services than women; however, the specific needs and preferences of men at risk of genetic conditions other than hereditary breast ovarian cancer are not known. We ascertain the information preferences of men with a family history of prostate cancer.
Methods: Unaffected men and their partners were administered a written questionnaire.
Results: Responses were received from 280 men (response rate: 59.2%) and 174 partners (response rate: 74%). Most men (59.6%) reported having insufficient information about their risk and wanted further information about personal risk (93.2%) and risk management (93.6%). Strikingly, 56.3% preferred to receive information related only to positive outcomes. Urologists were the preferred source of information, but there was considerable interest in a multidisciplinary service approach significantly associated with the number of affected relatives (odds ratio = 1.94, P < .002). Partners' level of concern was not associated with interest in multidisciplinary services, satisfaction with information, or support received.
Conclusions: Delivering services to men at risk will require a multifaceted approach by primary care providers and specialists. Challenges include meeting men's expectations in the face of uncertain medical knowledge, engaging those at high risk in multidisciplinary services, and delivering tailored information to those at lower risk.
Similar content being viewed by others
Main
Men have a lower uptake of genetic services1,2 and genetic testing3 than women and may have different responses to coping with and disclosing genetic information.3,4 Despite these differences, men's preferences for genetic service delivery have not been sought or identified. In cancer genetics particularly, the delivery of genetic services has been largely influenced by the experiences of women with, or at risk of developing, hereditary breast-ovarian cancer.5–7 One retrospective study examined the needs of men with BRCA1 and BRCA2 mutations and found them generally satisfied with genetic counseling, but this did not ascertain preferences. It cannot be assumed that men at risk of other hereditary cancer predispositions have the same needs as men with mutations predisposing predominantly to breast cancer.
Understanding men's preferences for the delivery of cancer genetic information becomes important when considering services for men with a family history of prostate cancer. These men have a risk of developing prostate cancer that increases with the number of affected relatives and a decreasing age of diagnosis.8–11 An autosomal dominant form (hereditary prostate cancer) has been defined,8 and 2% to 3% of all prostate cancer cases meet these criteria, with up to one third of cases diagnosed before 60 years possibly caused by dominantly inherited mutations in susceptibility genes.12 Nonetheless, the molecular basis of susceptibility remains unclear.13 Currently, it is uncommon for men with a family history suggestive of hereditary prostate cancer to be seen in cancer genetics clinics. In Australia and possibly other countries, this may be due in part to the minimal guidelines for screening or referral of men with a family history of prostate cancer to cancer genetic services.14,15 As the contribution of BRCA2 and other genes to hereditary prostate cancer is clarified,16,17 and the effectiveness of screening in men at increased risk becomes better understood, this situation may change. Meanwhile, it is likely that men with a family history of prostate cancer have unmet needs as they live with increased worry,18 feelings of vulnerability about developing this condition,19,20 and concern for their sons.21
As a first step to developing genetic services for hereditary prostate cancer, this study aimed to identify the information and support needs of men with a family history of prostate cancer and to explore their preferences for how these needs could be met. Those who seek cancer genetic services are usually either at high risk or concerned but not at high risk. To obtain a sample that includes both these groups, a population-based sample identified as having an increased risk family history through their participation in research and a self-selected group who sought participation in prevention trials were recruited. Because women play an important role in health service use by the men in their lives,22,23 the influence of spouses was also investigated.
METHODS
Sample
Respondents were recruited from two existing cohorts. The first was a register of 179 men held at the Urology Department at the Royal Melbourne Hospital. These men were originally ascertained through advertisements in the print media, inviting men who self-reported a family history of prostate cancer to register with a view to participating in research on familial prostate cancer. The family histories of these men have not been verified. No previous research had been performed on these men at the time of this survey. This cohort is referred to as the “self-selected sample” in the text.
The second source of ascertainment was through a sample of 325 men from a register of men with a verified family history of prostate cancer held by The Cancer Council of Victoria. The men were identified by affected relatives and are part of a population-based study, The Australian Prostate Cancer Family Study. Eligibility and recruitment procedures to that study have been described.24 For the current study, a subgroup of these respondents was selected on the basis of family history, comprising two or more relatives with prostate cancer or one relative with prostate cancer diagnosed before 55 years of age. In the text, this sample is referred to as the “family study sample.”
Additional eligibility criteria for both samples were no prior diagnosis of prostate cancer, ability to give informed consent, and literacy in English, because data were collected using self-reported questionnaires.
Procedure
This study was undertaken as part of a larger study that also assessed the accuracy and completeness of reporting family history of prostate cancer,25 surveillance practices (Meiser, manuscript submitted), interest in genetic testing, and perceived risk for prostate cancer (Ruth Cowan, BSc, unpublished data). The study was approved by the ethics committees of Melbourne Health and the Cancer Council Victoria. Questionnaires and reply-paid envelopes were mailed through each of the primary study centers. The package included an approach letter outlining the purpose of the study, a questionnaire, and a reply-paid envelope. A brief questionnaire and a separate reply-paid envelope were included in this mail-out for completion by partners of respondents. A reminder letter was sent to respondents 1 month after the initial mailing by the participating centers. The return of a completed questionnaire was accepted as consent for participation.
Data collection and measures
The questionnaire included both previously validated and new purposively designed items. The questionnaires were pilot-tested with 25 men; however, this did not lead to changes in the wording of the newly designed items described here. Thus, the 25 questionnaires administered as part of the pilot phase were included in the final sample.
Sociodemographic variables
Sociodemographic variables included age, marital status, level of education, number, age at diagnosis, relationship of relatives with prostate cancer, and whether the respondent had sons.
Risk perception
A visual analogue scale anchored by 0% to 100% assessed perceived lifetime risk by age 75 years.
Concern about prostate cancer
Concern about prostate cancer was assessed with one item using a 5-point Likert-type scale.
Previous information and support
Two items used a 5-point Likert-type scale to assess the amount of information about the risk of developing prostate cancer and the amount of support relating to the family history of prostate cancer the respondent had received.
Information preference style
Information preference style was determined using measures applied in previous studies.26,27 Two items used 5-point Likert-type scales to indicate how much information about prostate cancer and the available risk management options the respondent desires and how actively he has sought this information. The third item asked the respondent to indicate if he wants a minimal amount of information, only good information, or as much information as possible, both good and bad.27
Information, support, and health service preferences
Interest in seven types of information, support, and services was determined by a 3-point Likert-type scale. Interest in attending a “combined” service (defined as providing genetic information, medical advice, and support to men with a family history of prostate cancer) was ascertained with a 3-point Likert-type scale (“no,” “maybe,” and “definitely”). Preferred sources of information were assessed by asking respondents to assume that accurate information could be obtained from each of eight different sources and asking them to rank their preference from one (most preferred) to eight (least preferred). Preference for health care professionals was assessed in a similar way, with respondents asked to rank genetic specialist (medical geneticist or genetic counselor), cancer specialist (oncologist), prostate specialist (urologist), family doctor (general practitioner), and no health professional from one (most preferred) to five (least preferred).
Impact of Events Scale
The Impact of Events Scale, a 15-item scale, is a validated measure of intrusion and avoidance in relation to a specific stressor.28 In this study, the particular stressor was concern about being at risk of prostate cancer. The Impact of Events Scale has been used in related studies.18,29
Miller-Behavioral Style Scale
The Miller-Behavioral Style Scale is a four-item, validated scale that measures individual differences in coping styles in threatening situations.30 Respondents were asked to imagine four stress-provoking scenarios of a largely uncontrollable nature. Each scenario was followed by eight statements representing different attention strategies for dealing with the event, that is, “monitoring” (attending to) versus “blunting” (avoiding) potentially threatening information.
Partners' questionnaire
Several items were administered to partners; however, in this analysis we will only be reporting on one variable.
Partner concern about family history
Partner concern about family history was assessed with one item using a 5-point Likert-type scale, with response options ranging from “not at all concerned” (1) to “extremely concerned” (5). Partners were categorized, using a median split, into those with low and high concern about family history.
Statistical analyses
All data analyses were carried out using the Statistical Package for the Social Sciences Version 11.0 (SPSS Inc., Chicago, IL). Descriptive statistics were used to describe the sample in terms of sociodemographic and family history data and information and support needs. The variable relating to interest in a combined service was recoded as a binary variable for further analysis. Because only 8% of respondents responded that they would not attend a combined service, respondents who responded “maybe” were collapsed with those responding that they were not interested. To assess the association between interest in a combined service on the one hand and educational levels, recruitment source, having sons, and relationship status (unpartnered vs. low-concern partner vs. high-concern partner) on the other hand, chi-square analyses were performed. Mann-Whitney U tests were carried out for the non-normal interval variables of age, number of first- and second-degree relatives, perceived risk, and prostate cancer anxiety, and an independent t test was used for the monitoring score. Bivariate predictors significant at P less than .1 were entered into a logistic regression.
RESULTS
Response rates
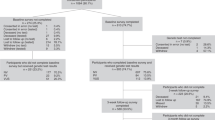
A total of 504 questionnaire packages were mailed. Of these, 325 were to men in the “family study” sample frame and 179 were to men in the “self-selected” sample frame. Twenty-three packages were returned to sender, and eight men were found to be deceased. Of the remaining 473 questionnaires that were mailed, 280 questionnaires were returned completed, resulting in an overall participation rate of 59.2%. The participation rate was 51.2% (n = 155) within the family study sample and 73.5% (n = 125) within the self-selected sample. If we assume that all of the 234 men with partners passed the partner's questionnaire on to their partners, then the response rate was 74% (n = 174). The sociodemographic and family history characteristics of the sample are shown in Table 1.
Need for prostate cancer information and support
When asked to comment on their concern regarding prostate cancer in the family, the mean concern rating was 3.48 (standard deviation [SD] = 1.16, range “not at all” [1] to “extremely” [5]). Twenty-two percent (21.8%) of the men were “extremely” concerned about their family history of cancer, and only 6.4% indicated they were “not at all” concerned. Respondents thought the amount of information they had received about their prostate cancer risk was less than enough with a mean rating for the amount of information of 2.15 (SD = 0.92, range: “not enough” [1], “enough” [3], “too much” [5]). A total of 59.6% of respondents indicated they had received less than enough information about this risk. Similarly, the mean satisfaction rating for the amount of support they had received about prostate cancer in the family was 2.40 (SD = 0.92, range “not enough” [1], “some but not enough” [3], “enough” [5]), with 43.9% responding they had received no support and a further 43.6% responding they had not received enough support.
Kruskal-Wallis tests showed no significant differences between the men's ratings for the amount of information they had received (χ2 = 0.2.18, P = .89) depending on whether men were unpartnered or had a partner with low or high concern about family history. The same was true for the men's satisfaction with the amount of support (χ2 = 4.49, P = .11) they had received about their prostate cancer risk.
Information and support preferences
Respondents preferred to obtain more information rather than less with a mean rating of 4.2 (SD = 1.2, range “no information” [1] to “as much information as possible” [5]), but had only been somewhat active in obtaining information (mean of 3.0, SD = 1.6, range “have not been active” [1] to “have been very active” [5]). Most respondents preferred only good information (56.3%), 34.4% of respondents reported that they preferred as much information as possible, both good and bad, and 6.1% of respondents reported that they preferred a minimal amount of information.
When asked to indicate their level of interest in peer support and six specific information and counseling services provided by cancer genetic services,31 the highest percentage (94%) of men were “very interested” and/or “interested” in information pertaining to risk management (Fig. 1). Obtaining information about personal risk was the second most frequently endorsed preference, with 93.2% of men responding as being either “interested” or “very interested,” closely followed by interest in the genetics of prostate cancer (88.9%). Although fewer men expressed interest in help dealing with the loss of family members who died of prostate cancer and interest in talking to other men who had a family history of prostate cancer, it is worth noting that 50% or more indicated some level of interest in each of these items.
Information and health services
Men expressed a clear preference for obtaining information about their situation directly from a health professional (Table 2a), with urologists being the most preferred type (Table 2b). Almost half the respondents indicated they would “definitely” attend (49.6%) a service for men with a family history of prostate cancer that provided genetic information, medical advice, and support; 41.8% indicated “maybe;” and 7.5% reported they would not attend. Among those reporting definite interest, 62.1% had just one or less first- or second-degree relative with prostate cancer. Several variables were significantly associated with interest in attending a combined service in bivariate analysis (Table 3). The recruitment source was significantly associated with interest, with 58.1% of the self-selected sample respondents “definitely interested” in attending, compared with 44.2% of men who were from the family study arm of the study (χ2 = 5.32; P = .021). Men who were “definitely interested” in attending a service had significantly higher prostate cancer risk perceptions (z = −2.66; P = .008) and a higher number of first and second-degree relatives with prostate cancer) (z = −3.17; P = .002). Even so, 36.6% of men with two or more affected relatives had little interest in attending a service. None of the other variables were significantly associated with interest in a combined service, including relationship status.
All variables significantly associated with interest in a specialist service in univariate analysis were entered into a logistic regression model (Table 4). Both recruitment source (odds ratio [OR] = 1.9; 95% confidence interval [CI], 1.15–3.24; P = .012) and number of first- and second-degree relatives with prostate cancer (OR = 1.56; 95% CI, 1.18–2.08; P = .002) remained significantly associated with interest in a combined service. By contrast, perceived risk was no longer significantly associated with interest in multivariable analysis (OR = 1.006; 95% CI, 0.99–1.02; P = .21).
DISCUSSION
In the absence of specialized cancer genetic services for men with a significant familial risk of prostate cancer, this study identified high levels of unmet information needs, concern about risk, and, to a lesser extent, a need for support among a sample of 280 men with a family history of this condition. These findings have implications for the delivery of health information to men at risk of prostate cancer and possibly for genetic services more broadly.
Sample considerations
We sought to recruit men who may be eligible to attend a cancer genetic service focusing on prostate cancer. In Australia, people at high risk of an inherited predisposition to cancer are eligible to attend cancer genetic services.15 Thirty percent of respondents in this study had two or more first- and second-degree relatives affected by prostate cancer and therefore represent those men who would be very likely to be eligible to attend a prostate cancer genetics service. The remainder may not meet “high-risk” criteria but might still seek advice from such a service, as has been observed of women at moderate or population-based risk of breast cancer.32 This supposition is supported by the significant association (P = .012) between reported interest in a multidisciplinary service and being self-selected for research because most of that sample had a low number of first- and second-degree relatives with prostate cancer. It is also worth noting that the self-selected sample seems to be a highly motivated group, with a response rate 22.3% greater than that of the population-based sample. Therefore, this study captured the opinions of men who might be eligible to attend a cancer genetic service or ineligible but concerned. Respondents, however, were not necessarily representative of the broader population of men with a family history of prostate cancer. Respondent education levels were consistent with those of current attendees of familial cancer clinics in Australia, who have above average educational levels.33,34
Information and support needs
Many respondents were concerned about their family history of prostate cancer and thought that the information they had previously received about their prostate cancer risk was inadequate. The majority (53%) preferred good information only. This is consistent with a study of people affected with cancer27 and contrasts with a study of Australian women at risk for ovarian cancer, in which only 1.6% said they wanted only good information, most preferring information about both good and adverse outcomes.35 The phrasing of the measure in the study of Tiller et al.35 was more specific to “good news,” and this may in part account for the discrepancy in results. However, many men have a functional approach to health, seeing it as a resource that gives them the ability to do what they want to do.36 Good information then may be that relating to maintaining health, and only this would be of interest. This supposition is consistent with risk-management advice being of greatest interest to respondents. Given the lack of agreement about factors that reduce the risk of prostate cancer37 and the current uncertainty about whether screening for prostate cancer reduces mortality,38 meeting these needs provides a potential challenge for health care providers in the short term.
Respondents also had high levels of interest in information about personal and family risk and the genetics of prostate cancer. Although empirical data are available to counsel men about their risk based on family history,24 providing information about the genetics of prostate cancer is less straightforward because the molecular basis of hereditary prostate cancer predisposition is poorly understood.13 Still, there may be benefit in responding to misconceptions held by these men about the effect of (hypothetical) genetic testing on health outcomes (Ruth Cowan, BSc, unpublished data) and to lay beliefs about inheritance that are commonly held by families with inherited conditions.39,40
Although items relating to counseling and peer support were the least endorsed by respondents, approximately half of the respondents did indicate some level of interest in each of these services, and the majority indicated they had not had any or enough support in relation to their family history. Prioritizing information over support was also observed in a study of women's expectations of cancer genetic services41 and is consistent with the content of genetic counseling consultations.42
Implications for service delivery
This study suggests that there is a need for delivery of information at the very least to some men with a family history of prostate cancer. As for women with a family history of breast cancer,41 respondents' first preference is generally for health professionals to deliver this information. The existing health care model for cancer genetics in many developed countries is of specialized clinics,15 often led by genetic specialists, providing information (i.e., risk estimates, inheritance, risk management options) and supportive counseling to those considered at high risk of an inherited cancer predisposition. Attendance at genetic counseling services has been found to increase knowledge and provide psychologic benefits,43 yet genetic specialists were the health professionals cited as the least preferred source of information. “Genetics” is commonly associated by lay people with reproduction and inheritance.44 Because these at-risk men are likely to be predominantly concerned about their own health rather than reproductive issues, it is perhaps understandable that they tend toward seeing urologists or family physicians, who may be perceived as able to provide information about management and risk, as well as genetics. A health service providing a coordinated approach, with different specialists providing clients with genetic information, risk assessment, surveillance options, and counseling, may be best suited to meet high-risk men's needs. This could be provided in conjunction with, or within, a urology service. There was a strong level of interest in such a multidisciplinary service, a service model successfully applied in colorectal cancer.1 Interest was positively associated with the number of relatives with prostate cancer, suggesting that a service targeting men at high risk of prostate cancer would attract those to whom it is targeted, that is, men with a strong family history of the disease.
A service for men at high risk is also likely to attract men at lower risks, because a sizable proportion of these men also expressed an interest in attending a multidisciplinary clinic. Alternative strategies to meet the needs of these men will need to be evaluated, and both resource issues and appropriate targeting of health messages must be considered. Clearly, health professionals such as family practitioners and urologists are an important source of information for respondents, and the information needed by men may be incorporated into other health care appointments. However, health professionals cannot be relied on as the sole source of information about prostate cancer risk because the uptake of health services by men is generally low,45 and men are less likely to have a regular doctor or to have had a general medical checkup in the last 12 months and had a lower number of visits to doctors in the same period.46 Written materials are a cost-effective option, and brochures were a popular source of information among respondents. These have the advantage of flexibility (for standalone use or to reinforce a face-to-face consultation), can potentially be accessed from sources other than health services, and are an “enduring resource.” Still, they may not be sufficient to reassure; a pilot study of women receiving cancer genetic risk information by letter suggests that a proportion of individuals will remain concerned about their risk or want additional information.32 If specialized services are established, then mechanisms to address the concerns and needs of the large group of men not eligible will also need to be established.
More than one third of men at potentially high risk in this study showed little interest in attending a multidisciplinary service; lower uptake by men of such services has also been observed for hereditary colorectal cancer. 2,33 Despite interest in information and concern about their family history, respondents generally had not been very active in obtaining information. The difficulties of engaging men in health services are well known, and providing information to women to pass on to their partners and family members is one of the strategies proposed to overcome barriers to health services.36 Partners' views seem to be influential in men's decisions to undergo genetic testing for BRCA1 and BRCA2 mutations.47 Anticipating that spouses may play a role in men's interest in information about their family history of cancer, we surveyed both men and their partners. However, respondents' interest in a combined service was not associated with their relationship status or the level of concern reported by their partners. Men with partners were no more satisfied with the amount of information and support they had in relation to their family history, regardless of the level of concern of their spouse. This suggests that, within this group of men, spouses may not have a great influence over men's health needs or attitudes relating to prostate cancer.
CONCLUSIONS
This study was undertaken to identify resources needed by men from families at risk of prostate cancer, prioritize their service needs, and ascertain the preferred modes of obtaining information. Their needs and preferred information sources were similar to those of women at risk of breast cancer, suggesting that existing services may be readily adapted for prostate cancer risk assessment. Certainly, the delivery of genetic risk and management advice to all concerned about their family history needs to be multidisciplinary and multifaceted. However, some caveats must be considered. Although the male relatives of 2% to 3% of men with prostate cancer are likely to be at risk of hereditary prostate cancer, and this study suggests a high level of interest in a multidisciplinary service, it is difficult to anticipate actual uptake because even respondents had only been somewhat active in obtaining information and are not necessarily representative of all men in this risk group. Second, many men may prefer only information that promotes positive outcomes, a need that may not be fulfilled with current levels of knowledge. This has considerable implications for the delivery of health care services for genetic conditions, particularly for conditions that are currently untreatable (e.g., Huntington disease) or, conversely, potentially treatable conditions such as familial hypercholesterolemia. This finding would benefit from duplication and further exploration in studies of other inherited conditions. If confirmed, it may inform the development of education material and genetic counseling for men at risk of a genetic condition.
References
Collins V, Halliday J, Warren R, Williamson R, et al. Assessment of education and counselling offered by a familial colorectal cancer clinic. Clin Genet 2000; 57: 48–55.
Holloway S, Porteous M, Cetnarskyj R, Rush R, et al. Referrals of patients to colorectal cancer genetics services in south-east Scotland. Fam Cancer 2005; 4: 151–161.
Taylor S . Gender differences in attitudes among those at risk for Huntington's disease. Genet Test 2005; 9: 152–157.
Marteau TM, Dundas R, Axworthy D . Long-term cognitive and emotional impact of genetic testing for carriers of cystic fibrosis: the effects of test result and gender. Health Psychol 1997; 16: 51–62.
Audrain J, Rimer B, Cella D, Garber J, et al. Genetic counseling and testing for breast-ovarian cancer susceptibility: what do women want?. J Clin Oncol 1998; 16: 133–138.
Hallowell N, Murton F, Statham H, Green J, et al. Women's need for information before attending genetic counselling for familial breast or ovarian cancer: a questionnaire, interview, and observational study. BMJ 1997; 314: 281–283.
Thewes B, Meiser B, Tucker M, Tucker K, et al. The unmet information and support needs of women with a family history of breast cancer: a descriptive survey. J Genet Couns 2003; 12: 61–76.
Carter BS, Bova GS, Beaty TH, Steinberg GD, et al. Hereditary prostate cancer: epidemiologic and clinical features. J Urol 1993; 150: 797–802.
Gronberg H, Wiklund F, Damber JE . Age specific risks of familial prostate carcinoma: a basis for screening recommendations in high risk populations. Cancer 1999; 86: 477–483.
Walsh PC, Partin AW . Family history facilitates the early diagnosis of prostate carcinoma. Cancer 1997; 80: 1871–1874.
Zegers M, Jellema A, Ostrer H . Empiric risk of prostate cancer carcinoma for relatives of patients with prostate carcinoma. Cancer 2003; 97: 1894–1903.
Bratt O . Hereditary prostate cancer. BJU Int 2000; 85: 588–598.
Edwards SM, Eeles RA . Unravelling the genetics of prostate cancer. Am J Med Genet C Semin Med Genet 2004; 129: 65–73.
Waggett D . Australian Health Technology Advisory Committee. Prostate Cancer Screening: Summary of the Review Prepared by the Australian Health Technology Advisory Committee. Vol 2001. Canberra: Commonwealth Department of Health and Family Services, 1996.
National Health and Medical Research Council. Familial Aspects of Cancer: A Guide to Clinical Practice. Canberra, Australia: National Health and Medical Research Council, 1999.
Edwards SM, Kote-Jarai Z, Meitz J, Hamoudi R, et al. Two percent of men with early-onset prostate cancer harbor germline mutations in the BRCA2 gene. Am J Hum Genet 2003; 72: 1–12.
Kirchhoff T, Kauff ND, Mitra N, Nafa K, et al. BRCA mutations and risk of prostate cancer in Ashkenazi Jews. Clin Cancer Res 2004; 10: 2918–2921.
Bratt O, Damber JE, Emanuelsson M, Kristoffersson U, et al. Risk perception, screening practice and interest in genetic testing among unaffected men in families with hereditary prostate cancer. Eur J Cancer 2000; 36: 235–241.
Jacobsen PB, Lamonde LA, Honour M, Kash K, et al. Relation of family history of prostate cancer to perceived vulnerability and screening behavior. Psychooncology 2004; 13: 80–85.
Miller SM, Diefenbach MA, Kruus LK, Watkins-Bruner D, et al. Psychological and screening profiles of first-degree relatives of prostate cancer patients. J Behav Med 2001; 24: 247–258.
Bratt O, Kristoffersson U, Lundgren R, Olsson H, et al. Sons of men with prostate cancer: their attitudes regarding possible inheritance of prostate cancer, screening, and genetic testing. Urology 1997; 50: 360–365.
Norcross WA, Ramirez C, Palinkas LA . The influence of women on the health care-seeking behavior of men. J Fam Pract 1996; 43: 475–480.
Parslow R, Jorm A, Christensen H, Jacomb P, et al. Gender differences in factors affecting use of health services: an analysis of a community study of middle-aged and older Australians. Soc Sci Med 2004; 59: 2121–2129.
Staples MP, Giles GG, English DR, McCredie MR, et al. Risk of prostate cancer associated with a family history in an era of rapid increase in prostate cancer diagnosis (Australia). Cancer Causes Control 2003; 14: 161–166.
Gaff CL, Aragona C, MacInnis RJ, Cowan R, et al. Accuracy and completeness in reporting family history of prostate cancer by unaffected men. Urology 2004; 63: 1111–1116.
Cassileth B, Zupkis RV, Sutton-Smith K, March V, et al. Information and participation preferences among cancer patients. Ann Intern Med 1980; 92: 832–836.
Butow P, Brindle E, MsConnell D, Boakes R, et al. Information booklets about cancer: factors influencing patient satisfaction and utilisation. Patient Educ Couns 1998; 33: 129–141.
Horowitz M, Wilner N, Alvarez W . Impact of Event Scale: a measure of subjective stress. Psychosom Med 1979; 41: 209–218.
Meiser B, Butow P, Barratt A, Friedlander M, et al. Breast cancer screening uptake in women at increased risk of developing hereditary breast cancer. Breast Cancer Res Treat 2000; 59: 101–111.
Miller SM . Monitoring and blunting: validation of a questionnaire to assess styles of information seeking under threat. J Pers Soc Psychol 1987; 52: 345–353.
Ponder BA . Setting up and running a familial cancer clinic. Br Med Bull 1994; 50: 732–745.
Phelps C, Platt K, France L, Gray J, et al. Delivering information about cancer genetics via letter to patients at low and moderate risk of familial cancer: a pilot study in Wales. Fam Cancer 2004; 3: 55–59.
Collins V, Halliday J, Warren C, Williamson R, et al. Assessment of education and counselling offered by a familial colorectal cancer clinic. Clin Genet 2000; 57: 48–55.
Meiser B, Butow P, Barratt A, Suthers G, et al. Attitudes to genetic testing for breast cancer susceptibility in women at increased risk of developing hereditary breast cancer. J Med Genet 2000; 37: 472–476.
Tiller K, Meiser B, Gould L, Tucker K, et al. Knowledge of risk management strategies, and information and risk management preferences of women at increased risk for ovarian cancer. Psychooncology 2005; 14: 249–261.
Hall RH . Promoting men's health. Aust Fam Physician 2003; 32: 401–407.
Villeneuve P, Johnson K, Kreiger N, Mao Y, et al. Risk factors for prostate cancer: results from the Canadian National Enhanced Cancer Surveillance System. The Canadian Cancer Registries Epidemiology Research Group. Cancer Causes Control 1999; 10: 355–367.
Cooperberg MR, Moul JW, Carroll PR . The changing face of prostate cancer. J Clin Oncol 2005; 23: 8146–8151.
McAllister M . Personal theories of inheritance, coping strategies, risk perception and engagement in hereditary non-polyposis colon cancer families offered genetic testing. Clin Genet 2003; 64: 179–189.
Chapple A, May C, Campion P . Lay understanding of genetic disease: a British study of families attending a genetic counseling service. J Genet Couns 1995; 4: 281–300.
Chalmers K, Luker K, Leinster S, Ellis E, et al. Information and support needs of women with primary relatives with breast cancer: development of the Information and Support Needs Questionnaire. J Adv Nurs 2001; 35: 497–507.
Butow PN, Lobb EA . Analyzing the process and content of genetic counseling in familial breast cancer consultations. J Genet Couns 2004; 13: 403–424.
Butow PN, Lobb EA, Meiser B, Barratt A, et al. Psychological outcomes and risk perception after genetic testing and counselling in breast cancer: a systematic review. Med J Aust 2003; 178: 77–81.
Kerr A, Cunningham-Burley S, Amos A . Drawing the line: an analysis of lay people's discussions about the new genetics. Public Underst Sci 1998; 7: 113–133.
Bayram C, Britt H, Kelly Z, Valente L, et al. Male Consultations in General Practice in Australia 1999-2000. Canberra: Australian Institute of Health and Welfare, 2003.
Kandrack MA, Grant KR, Segall A . Gender differences in health related behaviour: some unanswered questions. Soc Sci Med 1991; 32: 579–590.
Hallowell N, Ardern-Jones A, Eeles R, Foster C, et al. Men's decision-making about predictive BRCA1/2 testing: the role of family. J Genet Couns 2005; 14: 207–217.
Acknowledgements
We are grateful for the valuable contribution of all the men and their partners who participated in this study. We thank Dr. Rachel Iredale for helpful comments on the article and Professors Graham Giles and Anthony Costello for methodologic advice and facilitation of access to the study samples. Helen Crowe and Charmaine Payne assisted with recruitment, and Robert MacInnis advised on statistical analysis during the early stages of this project. Bettina Meiser was supported by a Career Development Award from The National Health and Medical Research Council of Australia (ID 350989).
Author information
Authors and Affiliations
Additional information
There are no conflicts of interest.
Rights and permissions
About this article
Cite this article
Gaff, C., Cowan, R., Meiser, B. et al. Genetic services for men: The preferences of men with a family history of prostate cancer. Genet Med 8, 771–778 (2006). https://doi.org/10.1097/01.gim.0000250204.97620.36
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1097/01.gim.0000250204.97620.36
This article is cited by
-
Monitoring style of coping with cancer related threats: a review of the literature
Journal of Behavioral Medicine (2014)
-
Unpacking the Blockers: Understanding Perceptions and Social Constraints of Health Communication in Hereditary Breast Ovarian Cancer (HBOC) Susceptibility Families
Journal of Genetic Counseling (2011)
-
Testicular Cancer and Genetics Knowledge Among Familial Testicular Cancer Family Members
Journal of Genetic Counseling (2008)