Abstract
Purpose: A randomized trial was conducted to test the effects of two counseling methods (genetic counseling and group counseling) against a control no-intervention condition on interest in genetic testing in lower risk women.
Methods: After completing baseline surveys, women (N = 357) were randomized to one of three conditions: to receive individual genetic risk counseling, to receive a group psychosocial group counseling, or to serve as a control group. Participants completed follow-up questionnaires 6 months after randomization.
Results: All participants had some familial history of breast cancer, but none had a family history indicative of autosomal dominant genetic mutation. At baseline over three fourths of the sample judged themselves to be appropriate candidates for testing. By the end of the survey, two thirds (70%) of the women in the counseling group still judged themselves to be appropriate candidates for testing. Findings were similar for interest in genetic testing. Changes in beliefs about genetic testing (e.g., beliefs about potential stigma associated with testing) altered the effects of counseling.
Conclusion: These results indicate that counseling can change interest in genetic testing only slightly and that changing women’s beliefs about the properties of testing might be one mechanism of doing so.
Similar content being viewed by others
Main
Genetic mutation testing to determine breast cancer risk is a relatively recent clinical option. Mutations in the BRCA1 and BRCA2 genes were discovered in 1995 to confer a relatively high risk of breast cancer in women with a strong family history of breast cancer.1,2 This type of genetic testing was offered to the public through physicians beginning in 1997. The low prevalence of the mutation in the general population combined with the difficulty in interpreting test results to any family except a high-risk family has caused most policy-making bodies to limit clinical testing to individuals with breast cancer and their family members in families with strong genetic histories.3–6
The extent to which genetic mutation testing is currently being used and will be used clinically in the near future is unknown. Several surveys of women from diverse samples indicate high interest, ranging from 55 to 80% of the respondents interested in obtaining testing.7–10 This high level of interest is astounding, as most women from the general public are not seen as appropriate medical candidates for breast cancer genetic testing. The few studies that have assessed actual use of the test indicate much lower uptake, as low as 10 to 20% in clinical studies.11 The reasons for this high interest and the potential methods of reducing it to more medically realistic levels are the topic of this article.
Contact with a counselor trained in assisting with risk-understanding could assist women in choosing their personal options for genetic mutation testing. We conducted a randomized trial to test the effects of two counseling types of settings against a control no-intervention condition. The first setting was genetic individual counseling in an individual setting. Genetic counselors were trained to fully explain the individual and family genetic risks for cancer and to address any worries and concerns associated with this risk information. The second counseling setting was group psychosocial group counseling, where a trained health counselor discussed risk, worry, and psychosocial issues in a group of four to eight women. We tested this counseling method because it is commonly implemented in hospitals and other clinical settings to help patients cope with health problems. Therefore, it is likely to be used for issues of genetic risk.
One of the reasons for studying uptake of BRCA1 and BRCA2 testing is that interpretation of the test results is sometimes unclear and ambiguous in the context of minimal genetic risk.12 Other research has indicated that an individual’s ability to tolerate ambiguity can determine responses to a situation that is not clearly defined or is still open to interpretation.13 We reasoned that for most individuals from the general public, low or nonexistent family history of breast cancer would make the results of genetic mutation testing confounding and ambiguous. Therefore, variance in tolerance for this ambiguity might help to determine an individual’s interest in obtaining testing.
Finally, we wanted to better understand the role of beliefs about the properties of cancer genetic tests in choosing to be tested. We reasoned that low-risk women wanted genetic testing because of a lack of knowledge about the properties of the genetic test. In previous research, we had identified three categories of knowledge about genetic testing: the possible stigma associated with getting a genetic test, the ability of a person to access genetic testing no matter what the risk background, and the ease of flow of information about the test results.7,14 We hypothesized that each of these knowledge categories would be likely to change as a result of counseling and could alter any effects of counseling on awareness of genetic testing for cancer risk, on interest in obtaining genetic testing, and on judgments of oneself as a good candidate for testing. We tested for each of these effects.
The purpose of this study was to test the effects of breast cancer risk counseling on interest in pursuing genetic testing in women with a family history of breast cancer. We predicted that counseling would reduce interest in obtaining genetic testing and reduce judgments of oneself as an appropriate candidate for genetic testing compared with a control group that received no counseling. We further hypothesized that this effect would be affected by an individual’s baseline tolerance level for ambiguous situations.13 Finally, we hypothesized that the effects of counseling would be affected by changes in beliefs about genetic testing, specifically beliefs targeted by counseling such as possible stigmatization due to testing and access issues around testing.
METHODS
Recruitment of subjects
Two forms of recruitment were used to recruit 357 women from the greater Seattle area, as described fully in another report.15 Eligible women were between the age of 18 and 74 years, lived within 60 miles of the research center, agreed to participate in counseling and complete the questionnaires, and had at least one relative (any degree) affected by breast cancer. Women were ineligible if more than one close relative was affected by breast cancer. Grandmothers, mothers, sisters, and aunts were counted as close relatives.
Measures
Background: Baseline demographics
Ethnicity, age, education level, current religion, marital status, sexual orientation, and annual income were sociodemographic factors measured on the initial surveys using common single item questions.
Outcomes: Awareness, candidacy, and interest in genetic testing
The participants were asked about their interest in genetic testing for breast cancer risk. The first of three questions read, “How much have you read or heard about genetic testing for breast cancer risk?” They could answer with one of the following responses, scaled 1 to 4: almost nothing, relatively little, a fair amount, or a lot. Participants were then asked, “Do you think you would be an appropriate candidate for genetic testing?” and “Are you interested in obtaining a genetic test?” with a response scale of 1 to 4, with 1 being “definitely not” and 4 being “definitely yes.” These variables were measured at baseline and at follow-up and defined as the main outcome measures for this study. For our main outcome analysis, the response items 3 and 4 were combined to form a trichotomous response scale (1, 2, 3/4) for each question.
Predictor: Tolerance for ambiguity
Tolerance for ambiguity was measured using questions modified from previous research.14 In this set of questions, participants were asked to what extent they agreed or disagreed with seven statements assessing the level of an individual’s ability to feel comfortable with clear or unclear situations. The responses to the questions were summed to provide an overall Tolerance for Ambiguity score for each participant, ranging from 7 to 42, with higher scores indicating greater Tolerance for Ambiguity.
Mediator: Beliefs about genetic testing
We measured specific beliefs about breast cancer genetic testing using three scales. All items for these scales consisted of belief statements with 5-point response scales ranging from strongly disagree to strongly agree. First, we adapted a 3-item scale measuring the fear of stigma associated with genetic testing for cystic fibrosis14 to stigma potentially associated with breast cancer. We drafted and included items measuring beliefs about unrestricted access to genetic testing (initial n = 5) and about unrestricted flow of information about test results among family members and physicians (initial n = 3). An example item for the access belief scale included, “Anyone who wants genetic testing for breast cancer risk should be able to get it, regardless of whether or not they can pay for it” and an item for the information flow included, “Physicians have an obligation to inform their patients’ relatives of the results of genetic testing.” We performed a factor analysis of principal components on the scales we developed, and the resulting scale items (final access scale n = 2 and final information flow scale n = 3) were averaged to form two separate scores. For each of the three scales (stigma, access, and information flow), higher values of the scale score indicated higher fear of stigma, more unrestricted access to genetic testing, and more free flow of information about test results. Alpha coefficients for each of these scales were reasonably high (α = 0.83, 0.78, and 0.82, respectively), indicating good internal consistency.
Description of counseling interventions
Two types of interventions were used, individual genetic individual counseling and psychosocial group counseling. Participants randomized to the individual genetic individual counseling arm met once, with a genetic counselor. The genetic individual counseling was a nondirective counseling focused on the individual participant and her family background. The participant was contacted by telephone to review the individual’s pedigree information and schedule a session with the genetic counselor. The second step was the 2-hour counseling session. This session followed a protocol based on standard genetic individual counseling practice. Each participant was provided with information regarding her own personal risk for breast cancer using a risk sheet that presented a participant’s Gail and Claus scores along with population data.16 In the session, the counselor gave information about genetic testing, current knowledge about nonhereditary risk factors for breast cancer, and current screening techniques. Participants were encouraged to ask questions and discuss their own concerns throughout the session. All genetic individual counseling participants received a summary letter after the session.
Participants randomized to the psychosocial group counseling arm met with a group four times. The group was lead by a health counselor and consisted of four to six women. Each session lasted 2 hours. During each session, introductory activities were done to encourage group participation, approximately 20 minutes of information was given, and a discussion was held to help the participant understand the relevancy of the information to their individual lives. The four main concepts of the psychosocial group counseling intervention were risk assessment and perception, education, stress management and problem-solving, and social support. The participant received educational information on her personal risk for breast cancer, interpretation of her level of estimated risk, and appropriate screening behaviors. Relaxation, coping with psychological distress, and coping with future health problems were the stress management techniques emphasized in the counseling sessions. The problem-solving skills discussed were assertiveness, cognitive restructuring to reduce intrusive thoughts about cancer, and using active rather than passive coping skills to resolve problems. Identifying potential supportive persons and institutions, defining needs for types of support, and eliciting support from these sources were taught as social support skills.
In both types of counseling, confidentiality of personal information was maintained and promoted. Personal risk information was only provided to the relevant person, and participants discussed issues of medical record information flow during the counseling sessions. In both counseling types, the participants were cautioned about free information flow between patient and medical record, about potential stigma associated with testing, and about barriers to access.
Procedures
Each potential participant completed a screening survey over the telephone to determine eligibility. During the screening survey, the women were also asked if they were interested in continuing with the study and where they had heard about the study. Those women eligible and interested in the study after the telephone survey were sent baseline surveys in the mail. The baseline survey measured demographics, knowledge and beliefs about cancer, tolerance for ambiguity, how much the individual had heard about genetic testing, whether she thought she was an appropriate candidate for genetic testing, and whether she was interested in obtaining a genetic test. After completion of the baseline survey, women were randomly assigned to one of two counseling conditions or a control group. The women then received either group psychosocial group counseling, individual genetic individual counseling, or served as a control group, receiving no counseling until after the final follow-up. The control participants were then offered their choice of counseling modalities to honor their participation in the study.
Six months after randomization, all participants were mailed a follow-up survey. If participants did not return the completed survey, study staff called up to 10 times and attempted to complete the survey over the telephone.
Analyses
First, we examined the demographic patterns of the study sample by randomization arms. The aims of these initial analyses were 2-fold: first, to confirm the effectiveness of randomization, and second, to identify potential bias by follow-up status and follow-up method. We then examined the relationship of counseling on average responses to baseline Tolerance for Ambiguity and on changing belief scores about genetic testing. Finally, we used polytomous logistic regression17 to examine the patterns of responses to awareness, interest, and candidacy judgments for genetic testing. This statistical technique, a special case of the more common dichotomous logistic regression, allowed us to test intervention effects on three levels of each outcome variable. Standard dichotomous logistic regression only allows for two levels of outcome variable. For each analysis, we included the participant’s Gail score18 as an indicator of medical risk. Gail score was not related to any outcome or predictor variable.
RESULTS
A total of 799 participants called the study line from the two recruitment sources. Seven hundred twenty-one participants were reached by telephone for the screening contact (579 were recruited from media contact and 142 from case) and 561 were eligible after the screening. Reasons for ineligibility at screening were lack of family history of breast cancer (3.2%), more than one close relative with breast cancer (14.1%), age outside the range (0.1%), living outside the catchment area (0.7%), and lack of interest in completing the study procedures (7.1%). A total of 160 participants were ineligible, 114 due to criteria and 46 from disinterest. The remaining 561 participants received a baseline survey in the mail to complete. A total of 357 participants returned surveys and were randomized to the study, 120 to genetic individual counseling, 114 to psychosocial group counseling, and 123 to delayed counseling. At follow-up, we attempted to collect survey data from all randomized participants. We received 317 surveys by mail and collected a further 31 surveys by telephone, for a final response from 348 women. Individuals with missing data for any scales or items were dropped from analyses, and the final sample size for the regression analyses was 317. Ninety-eight percent of participants completed the full counseling protocol.
Table 1 shows the demographic data by randomization arm of the study. In general, our participants were mostly white, of early middle age, mostly with college degrees, mostly married, heterosexual women. The household income data showed a range, with most participants’ households earning greater than $30,000. None of the demographic variables differed significantly by randomization arm, indicating that the randomization was effective in balancing characteristics in each group. We also tested for differences in demographic variables at baseline for individuals that did and did not provide 6-month follow-up data and for individuals that provided follow-up data by mail versus telephone. No significant differences in these comparisons were detected.
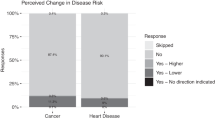
We present the analysis of the main outcome variables, baseline, and follow-up data on awareness, interest, and candidacy judgments by arm of study in Table 2. Visual inspection of Table 2 revealed that two thirds of the sample had heard nothing or relatively little about genetic testing at baseline, across all arms of the study. At follow-up, the responses in all arms had shifted toward “a fair amount” or “a lot” in all arms, with delayed counseling participants reporting somewhat fewer responses in the two high categories. Judgments of one’s candidacy for genetic testing followed a somewhat similar pattern. At baseline, over three fourths of the sample judged themselves to be appropriate candidates. By the end of the survey, only two thirds still judged themselves to be appropriate candidates for testing, although more control participants remained positive in their candidacy judgments. Most participants were interested in taking a genetic test for breast cancer risk at baseline, and that interest remained relatively strong at follow-up, changing least of the three judgment variables. Many individuals in all three arms, however, altered their judgments from the most definitive positive category to the two middle categories.
Data on two potential psychological predictors, baseline Tolerance for Ambiguity scores and changes in belief scores about genetic testing, are presented in Table 3. As seen in this table, Tolerance for Ambiguity scores did not differ among any of the counseling groups at baseline. The counseling intervention did change beliefs about genetic testing over time, as the interaction of time and arm was significant for two of the three sets for stigma and access specifically. For stigma, both counseling groups increased their belief ratings by 0.23, while the control group decreased its stigma score by −0.24 scale points. For access, both intervention groups decreased their ratings (−0.27 and −0.29 for Psychosocial and Genetic, respectively), while the control group increased its score by 0.19. These specific comparisons were significant using a post hoc Tukey test.
In Tables 4–6, we examined the predictors of difference in frequency of follow-up responses to the three outcomes of interest: awareness of genetic testing, candidacy judgments for genetic testing, and interest in getting genetic testing. Predictor variables were consistent across models: arm, age, education, baseline Tolerance for Ambiguity, and change in genetic testing belief scales. An odds ratio different from 1, with confidence intervals that do not include 1, indicates a significant predictor. We compared the frequency of two extreme responses for each question with the middle response. In other words, we compared the likelihood that someone would say “I’ve read almost nothing about genetic testing”and “I’ve read a lot/a fair amount” separately to the likelihood of saying “I’ve read relatively little,” in this case the middle response.
Table 4 presents the regression model predicting a likelihood of responses to an awareness of genetic testing question. The only significant predictor of response differences was counseling arm. Both counseling arms decreased the likelihood that participants would report the lowest extreme response (e.g., read about nothing). In contrast, genetic individual counseling was clearly predictive of increased awareness responses, while psychosocial group counseling was only slightly predictive of increasing awareness. Changes in the three belief scales were not related to the intervention effects or their significance.
The data for outcomes of candidacy judgments is presented in Table 5. Again, the strongest significant predictor of 6-month response differences in candidacy judgments was counseling arm, and the only other significant predictor in the model was educational level. Participants in both counseling arms were significantly more likely to report being an appropriate candidate for genetic testing. Individuals with lower educational levels were also more positive in their judgments of themselves as good candidates for testing. Two of the three belief scales change variables significantly predicted the candidacy judgment (data not shown). Increase in belief about stigma were related to women reporting more negatively in their perception of themselves as candidates (χ2 = 11.48;P < 0.02). Reporting that access should be controlled caused women to be more negative in their personal candidacy judgments (χ2 = 12.58;P < 0.01).
Finally, both counseling arm and educational level significantly predicted responses to interest in genetic testing, as shown in Table 6. Participants in both counseling arms were significantly more likely to report lower interest via movement to the “no” responses, compared with the control group. However, relative to delayed counseling, genetic individual counseling increased the likelihood of “definitely yes” responses, while psychosocial group counseling decreased likelihood of “definitely yes” (right-hand column). Education also had a mixed effect on interest responses. In both response patterns tested, the post-high school category increased the likelihood of extreme responding, while participants in the high school or less and the college degree categories reported decreased likelihood of extreme responding. Finally, changes in stigma significantly predicted interest changes in that increases in beliefs that testing produced stigma were related to women reporting less interest in testing (χ2 = 16.53;P < 0.002) (data not shown). No other belief change variables were significant predictors.
DISCUSSION
The results of this study indicate that counseling about breast cancer risk did slightly change the interest in genetic testing for breast cancer risk for women with a family history of breast cancer. These women had varied genetic risks, but all had some familial history of breast cancer, and none had a pattern of family history that would indicate the presence of autosomal dominant genetic mutations. Therefore, no participant in this study would be named a likely candidate for genetic testing, according to current recommendations for testing.19 Women who participated in the counseling sessions became less interested in obtaining genetic testing and less likely to judge themselves to be good candidates. This indicates that counseling did change participants’ desire to be tested for cancer risk.
Stigma and access beliefs about genetic testing were related to the effect of counseling on interest and candidacy judgments. We found that as women gained accurate information about the access issues, the potential stigma associated with breast cancer genetic testing, and the flow of information about testing, they would be less likely to want to participate. These findings suggest that if we could find ways to expose women to accurate information about the potential for stigma and difficulties with access regarding genetic testing, we would be able to reduce inflated interest and candidacy judgments in women who could not currently benefit from such testing. Other literature7–9 has documented strong interest in a woman with a variety of risks. Perhaps we should find ways to expose whole populations of women to this information instead of only research subjects who volunteer to be in a study.
However, there is one intriguing finding: counseling did not produce a very large or powerful decrease in interest or in candidacy judgments about breast cancer genetic testing. Indeed, everyone in the study reduced their interest and candidacy judgment levels somewhat across the course of the study based on visual review of the data. Simply participating in this study could have caused individuals in both the control group and the intervention group to learn more about the properties of genetic cancer risk testing. Everyone might have reduced her interest because of the increased knowledge. The local media covered the issue of breast cancer genetic testing more during the study period, and this increased public discussion could have contributed to the secular change. Counseling simply increased the effect in the intervention group.
There were several strengths to the present study, including the strong design, the broad risk levels of participants, and the practical nature of the counseling. There are also many limitations to the present study. Study sample ascertainment could result in bias here. The sample was not drawn to represent a population, but was composed of volunteers who saw a notice, heard about it from a network, or were contacted because of their relative with cancer. These women might be different from the general population of women in the local area. This program should be tested in a population-based sample. The requirements of the study were high enough (i.e., coming into the Fred Hutchinson Cancer Research Center to attend sessions, completing surveys) that not everyone could have participated. Reducing the research burden and participant travel burden will be important for future research. The interventions differed in contact time, a potential confound that could have influenced the outcomes. The short-term follow-up limits our understanding of these changes over time. The different amounts of contact time for each counseling method (one 2-hour session versus four 2-hour sessions) complicates interpretation of these findings. Finally, using candidacy judgments and interest in obtaining testing as outcomes is not as strong as using actual breast cancer genetic testing request or actual testing as the final outcome. We did not follow women for long enough to obtain actual testing choices. Therefore, we must conduct studies that actually assess women’s choice of cancer genetic testing or no testing to definitively determine the effects of counseling about personal risk on testing behavior.
References
Wooster R, Bignell G, Lancaster J, Swift S, Seal S, Mangion J, Collins N, Gregory S, Gumbs C, Micklem G . Identification of the breast cancer susceptibility gene BRCA2. Nature 1995; 378: 789–792.
Miki Y, Swensen J, Shattuck-Eidens D, Futreal PA, Harshman K, Tavtigian S, Liu Q, Cochran C, Bennett LM, Ding W . A strong candidate for the breast ovarian cancer susceptibility gene BCRC1. Science 1994; 266: 66–71.
American Society of Clinical Oncology Subcommittee on Genetic Testing for Cancer Susceptibility. Statement of American Society of Clinical Oncology: Genetic testing for cancer susceptibility. J Clin Oncol 1996; 14: 1730–1736.
National Advisory Council for Human Genome Research. Statement on use of DNA testing or presymptomatic identification of cancer risk. JAMA 1994; 271: 785.
American Society of Human Genetics Ad Hoc Committee on Breast and Ovarian Cancer Screening. Statement of the American Society of Human Genetics on genetic testing for breast ovarian predisposition. Am J Hum Genet 1994; 55: i–iv.
National Action Plan on Breast Cancer. Commentary on the ASCO statement on genetic testing for cancer susceptibility. J Clin Oncol 1996; 14: 1738–1740.
Durfy S, Bowen D, McTiernan A, Sporleder J, Burke W . Attitudes interest in genetic testing for breast ovarian cancer susceptibility in diverse groups of western Washington state women. Cancer Epidemiol Biomarkers Prev 1999; 8: 369–376.
Ulrich CM, Kristal AR, White E, Durfy S, Potter J . Genetic testing for cancer risk: a popular survey of attitudes intentions. Community Genet 1999; 1: 213–222.
Lerman C, Seay J, Balshem A, Audrain J . Interest in genetic testing among first-degree relatives of breast cancer patients. Am J Med Genet 1995; 57: 385–392.
Struewing J, Lerman C, Kase R, Giambarresi T, Tucker M . Anticipated uptake impact of genetic testing in hereditary breast ovarian cancer families. Cancer Epidemiol Biomarkers Prev 1995; 4: 169–173.
Codori AM, Petersen DL, Miglioretti DL, Larkin EK, Bushey MT, Young C, Brensinger JD, Johnson K, Bacon JA, Booker SV . Attitudes toward colon cancer gene testing: predicting test uptake. Cancer Epidemiol Biomarkers Prev 1999; 8: 345–352.
Slattery ML, Kerber R . A comprehensive evaluation of family history breast cancer risk. The Utah Population Database. JAMA 1993; 270: 1563–1568.
Geller G, Tambor ES, Chase G, Holtzman NA . Measuring physicians’ tolerance for ambiguity its relationship to the reported practices regarding genetic testing. Med Care 1993; 31: 989–1001.
Tambor ES, Bernhardt BA, Chase GA, Faden RR, Geller G, Hofman KJ, Holtzman NA . Offering cystic fibrosis carrier screening to an HMO population: factors associated with utilization. Am J Hum Genet 1994; 55: 626–637.
Bowen DJ, McTiernan A, Burke W, Powers D, Pruski J, Durfy S, Gralow J, Malone K . Participation in breast cancer risk counseling among women with a family history. Cancer Epidemiol Biomarkers Prev 1999; 8: 581–586.
Burke W, Bars J, Lowry D, Durfy S, Bowen DJ, McTiernan A . Genetic counseling for women with an intermediate family history of breast cancer. Am J Med Genet 1900; 90: 361–368.
Hosmer DW, Lemeshow S . Applied logistic regression. New York: Wiley, 1989.
Gail MH, Brinton LA, Byar DP, Corle DK, Green SB, Shairer C, Mulvihill JJ . Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst 1989; 81: 1879–1886.
Holtzman NA, Watson MS . Promoting safe and effective genetic testing in the United States: final report of the Task Force on Genetic Testing. Baltimore: Johns Hopkins University Press, 1998.
Acknowledgements
This research was supported by a grant from the National Cancer Institute and the National Human Genome Institute (HG01190).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Bowen, D., Burke, W., Yasui, Y. et al. Effects of risk counseling on interest in breast cancer genetic testing for lower risk women. Genet Med 4, 359–365 (2002). https://doi.org/10.1097/00125817-200209000-00007
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1097/00125817-200209000-00007
Keywords
This article is cited by
-
A Systematic Review of Randomized Controlled Trials to Assess Outcomes of Genetic Counseling
Journal of Genetic Counseling (2017)
-
Effects of a web-based intervention on women’s breast health behaviors
Translational Behavioral Medicine (2017)
-
A Rapid Systematic Review of Outcomes Studies in Genetic Counseling
Journal of Genetic Counseling (2017)
-
Effects of a Web-based intervention on women’s breast health behaviors
Translational Behavioral Medicine (2011)
-
Genetic testing for BRCA1: effects of a randomised study of knowledge provision on interest in testing and long term test uptake; implications for the NICE guidelines
Familial Cancer (2009)