Abstract
Purpose
The aim of this study was to examine the influence that the size of a neodymium:yttrium-aluminium-garnet (Nd:YAG) laser capsulotomy performed for posterior capsule opacification (PCO) has on visual acuity (VA), and on contrast VA and that in the presence of glare (glare VA).
Methods
A total of 41 consecutive eyes with PCO first underwent Nd:YAG laser capsulotomy of smaller than pupillary size, after which the capsulotomy was secondarily enlarged, 2 weeks later, to greater than pupillary size. Best-corrected VA, and contrast VA and glare VA under photopic and mesopic conditions were measured after the small and large capsulotomies were made.
Results
After enlargement, the mean capsulotomy area increased significantly from 4.8 to 15.3 mm2 (P<0.0001). Best-corrected VA did not improve significantly after enlargement (P=0.1282). However, photopic contrast VA and glare VA at moderate to low contrast visual target before enlargement were significantly worse than those after enlargement (P⩽0.0242); furthermore, mesopic contrast VA and glare VA improved significantly after enlargement (P⩽0.0431).
Conclusion
Contrast VA and glare VA with a small capsulotomy were significantly worse than those with a large capsulotomy, which suggests that a capsulotomy larger than the pupillary size is necessary to restore contrast sensitivity and glare disability.
Similar content being viewed by others
Introduction
It has been shown that posterior capsule opacification (PCO) following cataract surgery disturbs various visual functions, including visual acuity (VA), contrast sensitivity and glare disability, although controversy still remains as to which function is impaired most prominently due to PCO.1, 2, 3, 4, 5, 6, 7, 8, 9 However, we believe that the impairment of visual functions is related to the degree of PCO. In eyes with dense PCO that require neodymium:yttrium-aluminium-garnet (Nd:YAG) laser posterior capsulotomy, as all visual functions are impaired, VA is associated most strongly with the degree of PCO.7 When the PCO is slight, however, contrast sensitivity or glare disability deteriorates with no marked loss of VA.8
Nd:YAG laser posterior capsulotomy improves these visual functions. However, surgeons are often perplexed about what size of capsulotomy should be made. When a large capsulotomy is made, adverse effects of the Nd:YAG capsulotomy, such as retinal detachment,10, 11, 12 cystoid macular oedema12, 13 or a rise in intraocular pressure (IOP),14, 15 tend to occur. On the other hand, if the capsulotomy is too small, visual function may not be recovered. Indeed, previous studies showed that glare disability in eyes with a small capsulotomy is worse than those with a large capsulotomy despite no significant difference in VA.16, 17, 18 However, to date, there is no study about the relationship between capsulotomy size and contrast sensitivity.
The aim of the study described herein was to examine the influence of Nd:YAG laser capsulotomy size on VA, and on contrast sensitivity with and without glare. Because contrast sensitivity and glare disability varies substantially from patient to patient, we made the Nd:YAG laser posterior capsulotomy of smaller and larger than the papillary size in one eye, and the visual function was strictly compared between the eyes with small capsulotomy and those with large capsulotomy.
Patients and methods
Patients
All pseudophakic patients who were consecutively scheduled for Nd:YAG laser posterior capsulotomy between May 2007 and July 2008 were screened for inclusion in this study. An Nd:YAG laser capsulotomy was scheduled when an eye lost two or more decimal lines of VA or when the patient complained of blurred vision. One of the authors (KH) verified the presence of definite PCO on slit-lamp biomicroscopy and also performed patient screening. When both eyes were affected, only the eye that was scheduled for Nd:YAG capsulotomy first was screened. Pre-laser exclusion criteria were any pathology of the macula or optic nerve, previous history of inflammation, severe contraction of the anterior capsule or liquefied after-cataract. Eyes of diabetic patients and of long axial length were not excluded. Post-laser exclusion criteria were best-corrected VA of <0.5 due to any pathology of unknown cause, media opacities other than PCO and any difficulties with data collection or analysis. A total of 45 eyes of 45 patients who met the inclusion criteria were identified and recruited. The study protocol was approved by the institutional review board. Informed consent was obtained from each patient, and the study was conducted in accordance with the tenets of the Declaration of Helsinki Principles.
Laser procedures
A surgeon (FN) first made an Nd:YAG laser capsulotomy of smaller than the pupillary diameter using a Q-switched Nd:YAG laser (YC-1300; Nidek, Gamagori, Japan). After topical anaesthesia, a contact lens was applied to enhance power density at the level of the posterior capsule. The central posterior capsule within the pupillary area was cleared as much as was possible without pupil dilation by emitting laser energy on the posterior capsule; energy levels were between 0.5 and 1.5 mJ. Special care was taken to not to pit the intraocular lens (IOL) optic.
At approximately 2 weeks after the first capsulotomy, after full pupil dilation, the capsulotomy opening was enlarged to greater than the pupillary area (approximately 5.0 mm in diameter) by the same surgeon who used almost the same technique as was used for the smaller capsulotomy.
Outcome measures
Best-corrected VA on decimal charts, and contrast VA and that in the presence of a glare source (glare VA) were measured at 2 weeks after the first capsulotomy and at 2 weeks after the enlargement. Contrast VA and glare VA were examined using the Contrast Sensitivity Accurate Tester (CAT-2000; Menicon, Tokyo, Japan).8 This device measures the logarithm of the minimal angle of resolution (logMAR) VA using five contrast visual targets (100, 25, 10, 5 and 2.5%) under photopic and mesopic conditions. Measurement under photopic conditions was made with chart lighting of 100 cd/mm2, and that under the mesopic conditions was done with chart lighting of 3 cd/mm2. A glare light source of 200 lux was located in the periphery at 20° along the visual axis.
The area of the Nd:YAG capsulotomy opening was measured using the Scheimpflug photography system (EAS-1000; Nidek) at 2 weeks after the small capsulotomy was created and at 2 weeks after its enlargement. The refractive status (spherical and cylindrical powers) and keratometric cylinder were measured using an auto-refractometer (KR-7100; Topcon, Tokyo, Japan). The manifest spherical equivalent was determined as the spherical power plus half the cylindrical power. The pupillary diameter under photopic and mesopic conditions was examined using an electronic pupillometer (FP-10000; TMI, Saitama, Japan). The central retinal (foveal) thickness was measured using the Stratus optical coherence tomography-3 (OCT-3; Carl Zeiss Meditec, Dublin, CA, USA). IOP was measured by the same surgeon (FN) using an applanation tonometer before and at 2 h after the Nd:YAG laser capsulotomy. All other measurements were made by ophthalmic technicians who were not aware of the purpose of this study.
Statistical analysis
Decimal VA was converted to a logMAR scale for statistical analysis. Contrast VA and glare VA were also converted to the logarithm of inverse values for statistical analysis. Best-corrected VA, contrast VA and glare VA, area of the anterior capsule opening and other continuous variables before and after enlargement of the capsulotomy opening were compared using the Wilcoxon signed-rank test. Any differences showing a P-value of <0.05 were considered to be statistically significant.
Results
Of the 45 eyes of 45 patients originally enrolled, 4 eyes were excluded: 2 patients refused to undergo two-step YAG capsulotomy, and 2 did not appear for the follow-up examination because of a scheduling conflict. Accordingly, 41 eyes of 41 patients remained for analysis. The average age of the patients (±standard deviation (SD)) was 74.1±8.0 years, with a range of 49–88 years; there were 9 men and 32 women. All patients had Elschnig pearls type of PCO. Patient characteristics after small and large capsulotomies are shown in Table 1. No statistically significant differences were found in the mean manifest spherical equivalent value, keratometric cylinder or pupillary diameter under mesopic conditions. However, the pupillary diameter under photopic conditions after enlargement of the capsulotomy was significantly greater than that after the initially made small capsulotomy. The average time interval between the Nd:YAG capsulotomy and final follow-up was 13.5±5.1 months, with a range of 4–21 months.
After the small capsulotomy was made with the Nd:YAG laser, the mean area of capsulotomy opening was 4.8±1.5 mm2. After enlargement to large capsulotomy, the opening area increased to 15.3±4.7 mm2, which was significantly greater than that before enlargement (P<0.0001). All eyes showed an increase in the capsulotomy opening area after the enlargement.
Mean best-corrected decimal VA was 0.49±0.27 before Nd:YAG capsulotomy, 0.95±0.14 after the small capsulotomy and 0.96±0.14 after enlargement of the capsulotomy. Mean corrected VA improved significantly even after the small capsulotomy (P⩽0.0001), and it did not improve significantly more after enlargement (P=0.1729). No eye showed a decrease in corrected VA due to either Nd:YAG capsulotomy.
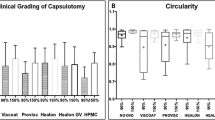
Under photopic lighting conditions (Figure 1), contrast VA and glare VA at moderate to low contrast visual targets after enlargement of the capsulotomy were significantly better than those before enlargement (P⩽0.0242), although no significant difference was found at high contrast visual targets. Under mesopic conditions (Figure 2), contrast VA and glare VA at high to moderate visual targets improved significantly after enlargement to the large capsulotomy (P⩽0.0136), but no significant difference was found in the contrast VA and glare VA at low contrast visual target primarily because it was immeasurable in most of the patients (Figure 2).
Mean contrast visual acuity (VA) and that in the presence of a glare source (glare VA) under photopic conditions after small and large capsulotomies using the Nd:YAG laser. Mean contrast VA and glare VA under photopic conditions at moderate to low contrast visual targets after small capsulotomy were significantly worse than that after large capsulotomy.
Mean contrast visual acuity (VA) and that in the presence of a glare source (glare VA) under mesopic condition after small and large capsulotomies using the Nd:YAG laser. Mean contrast VA and glare VA under mesopic conditions at high to moderate visual targets after small capsulotomy were significantly worse than that after large capsulotomy, and that at low visual targets could not be measured.
After both small and large capsulotomies, no significant correlation was found between the opening area created by the capsulotomy and best-corrected VA, and between the opening area and the contrast VA or glare VA. In addition, there was no significant correlation between the pupillary diameter and best-corrected VA, contrast VA or glare VA. However, significant correlations were found between patient's age and the contrast VA and glare VA at some high and moderate contrast visual targets.
The types of IOL implanted were three-piece spherical hydrophobic acrylic IOL in 29 eyes, three-piece aspheric hydrophobic acrylic IOL in 8, single-piece spherical hydrophobic acrylic IOL in 3 and single-piece spherical polymethyl methacrylate IOL in 1. No significant differences were found in best-corrected VA, contrast VA and glare VA between four types of IOL as well as between spherical IOL and aspheric IOL.
The mean foveal thickness as determined with the OCT-3 was almost the same at baseline (before the small capsulotomy), before the large capsulotomy (at 2 weeks after the small capsulotomy) and at 2 weeks after the large capsulotomy (Table 2). During the follow-up, no eye showed cystoid macular oedema and retinal breaks as well as retinal detachment due to the Nd:YAG laser capsulotomy. The mean IOP was similar just before the small capsulotomy, at 2 h after the small capsulotomy, immediately before enlargement of the capsulotomy and at 2 h after conversion to the large capsulotomy (Table 2). The increase in IOP before and after the small capsulotomy and before and after enlargement to a large capsulotomy was also similar.
Figure 3 shows a representative eye that underwent this two-step Nd:YAG laser capsulotomy. The Elschnig pearls type of PCO was seen 38 months after cataract surgery (Figure 3, top). An Nd:YAG laser posterior capsulotomy smaller than the pupillary area was first made (Figure 3, middle), then at 2 weeks after the small capsulotomy, the capsulotomy opening was enlarged to greater than the pupillary area (Figure 3, bottom).
Retro-illumination photographs of a representative eye that underwent two-step neodymium:yttrium-aluminium-garnet (Nd:YAG) laser capsulotomy. The Elschnig pearls type of posterior capsule opacification is seen before Nd:YAG laser capsulotomy (top). An Nd:YAG laser posterior capsulotomy of smaller than the pupillary size was first made (middle). At 2 weeks after this small capsulotomy, the capsulotomy opening was enlarged to greater than pupillary size (bottom).
Conclusion
Our study has demonstrated that, in eyes with PCO, mean VA with Nd:YAG laser capsulotomy of smaller than the pupillary area did not differ significantly from that with capsulotomy of larger than the pupillary area. However, photopic contrast VA and glare VA at moderate to low contrast visual target with the large capsulotomy were significantly better than those with the small capsulotomy. Furthermore, mesopic contrast VA and glare VA improved significantly after enlargement of the capsulotomy. This suggests that Nd:YAG laser posterior capsulotomy of larger than the pupillary area is necessary to recover substantially the contrast sensitivity and to lessen substantially glare disability in eyes with PCO.
When surgeons make a large Nd:YAG laser capsulotomy, they are often concerned about the occurrence of adverse effects, such as retinal detachment,10, 11, 12 cystoid macular oedema12, 13 or an increase in IOP.14, 15 Accordingly, we examined the occurrence of these adverse effects, although the sample size was small. In this series, retinal breaks and retinal detachment did not occur up to the final follow-up. The foveal thickness did not increase after enlargement to a large capsulotomy, and no cystoid macular oedema was seen. In addition, the increase in IOP after either the small or large capsulotomy was slight, and no significant difference was found in increase in IOP between the small and large capsulotomies. Furthermore, it has been shown that the incidence of retinal detachment and cystoid macular oedema after Nd:YAG laser capsulotomy is uncommon in eyes that have previously undergone phacoemulsification and in-the-bag implantation of an IOL.19, 20, 21, 22 These findings suggest that the incidence of the adverse effects may not differ markedly between eyes with a small capsulotomy and those with a large capsulotomy.
Previous studies have shown that PCO impairs various visual functions, including VA, contrast sensitivity and glare disability.1, 2, 3, 4, 5, 6, 7, 8, 9 Our studies showed that VA is correlated most strongly with the degree of PCO when it is so dense as to require an Nd:YAG capsulotomy,7 whereas contrast sensitivity or glare disability is deteriorated most prominently, without significant loss of VA, when the PCO is slight.8 It is clear that all of the visual functions improved after Nd:YAG capsulotomy, but the degree of improvement may depend on the size of the capsulotomy. Indeed, several studies showed that glare disability was worse with a small capsulotomy than with a large capsulotomy.16, 17 Holladay et al23 assumed that Nd:YAG capsulotomy of equal or larger than the pupillary diameter under scotopic conditions is necessary for recovering image intensity and for lessening glare disability. We verified that both contrast VA and glare VA are recovered in eyes that undergo capsulotomy of larger than the pupillary size.
The impairment of contrast VA and glare VA in eyes with a small capsulotomy can be explained as follows. The amount of light entering into the eye is dependent on the pupillary size. When the Nd:YAG laser capsulotomy opening is smaller than the pupillary size, the light entering into the eye, and ultimately reaching the macula, is intercepted by the unopened part of the opaque posterior capsule, which may lead to the decrease in contrast sensitivity. Furthermore, as the entering light passes through the residual capsule, it will be scattered, which may cause glare disability. However, even when the capsulotomy is small, the optical centre of the pupillary area is not occluded, and light entering along the visual axis may thus not be restricted enough to decrease markedly the VA.
In conclusion, contrast VA and glare VA with an Nd:YAG laser capsulotomy of larger than the pupillary size are better than that with a capsulotomy of smaller than the pupillary size, although size of the capsulotomy does not influence significantly the VA. The incidence of adverse effects after Nd:YAG laser capsulotomy did not differ markedly between eyes with a small capsulotomy and those with a large capsulotomy. Accordingly, to restore contrast sensitivity and to lessen glare disability, the surgeon should elect to make an Nd:YAG laser capsulotomy of larger than pupillary size. Further study using a larger sample is called for to clarify the incidence of adverse effects due to this large Nd:YAG laser capsulotomy.
References
Nadler DJ, Jaffe NS, Clayman HM, Jaffe MS, Luscombe SM . Glare disability in eyes with intraocular lenses. Am J Ophthalmol 1984; 97: 43–47.
Knighton RW, Slomovic AR, Parrish II RK . Glare measurements before and after neodymium-YAG laser posterior capsulotomy. Am J Ophthalmol 1985; 100: 708–713.
Sunderraj P, Villada JR, Joyce PW, Watson A . Glare testing in pseudophakes with posterior capsule opacification. Eye 1992; 6: 411–413.
Wilkins M, McPherson R, Fergusson V . Visual recovery under glare conditions following laser capsulotomy. Eye 1996; 10: 117–120.
Tan JCH, Spalton DJ, Arden GB . Comparison of methods to assess visual impairment from glare and light scattering with posterior capsule opacification. J Cataract Refract Surg 1998; 24: 1626–1631.
Magno BV, Datiles MB, Lasa MSM, Fajardo MRQ, Caruso R, Kaiser-Kupfer MI . Evaluation of visual function following neodymium:YAG laser posterior capsulotomy. Ophthalmology 1997; 104: 1287–1293.
Hayashi K, Hayashi H, Nakao F, Hayashi F . Correlation between posterior capsule opacification and visual function before and after neodymium:YAG laser posterior capsulotomy. Am J Ophthalmol 2003; 136: 720–726.
Hayashi K, Hayashi H . Posterior capsule opacification in the presence of an intraocular lens with a sharp vs rounded optic edge. Ophthalmology 2005; 112: 1550–1556.
van Bree MCJ, Zijlmans BLM, van den Berg TJTP . Effect of neodymium:YAG laser capsulotomy on retinal straylight values in patients with posterior capsule opacification. J Cataract Refract Surg 2008; 34: 1681–1686.
Leff SR, Welch JC, Tasman W . Rhegmatogenous retinal detachment after YAG laser posterior capsulotomy. Ophthalmology 1987; 94: 1222–1225.
Javitt JC, Tielsch JM, Canner JK, Kolb MM, Sommer A, Steinberg EP . National outcomes of cataract extraction: increased risk of retinal complications associated with Nd:YAG laser capsulotomy. The Cataract patient Outcomes Research Team. Ophthalmology 1992; 99: 1487–1497; discussion 1497–1498.
Steinert RF, Puliafito CA, Kumar SR, Dudak SD, Patel S . Cystoid macular edema, retinal detachment, and glaucoma after Nd:YAG laser posterior capsulotomy. Am J Ophthalmol 1991; 112: 373–380.
Shah GR, Gills JP, Durham DG, Ausmus WH . Three thousand YAG lasers in posterior capsulotomies: an analysis of complications and comparison to polishing and surgical discission. Ophthalmic Surg 1986; 17: 473–477.
Channell MM, Beckman H . Intraocular pressure changes after neodymium-YAG laser posterior capsulotomy. Arch Ophthalmol 1984; 102: 1024–1026.
Stark WJ, Worthen D, Holladay JT, Murray G . Neodymium:YAG lasers: an FDA report. Ophthalmology 1985; 92: 209–212.
Lohmann CP, Goble R, O'Brart D, Fitzke F, Marshall J, Gabel V-P . Blendungsempfindlichkeit vor und nach Nd:YAG-kapsulotomie: ein vergleich zwischen kleiner und groβer kapsulotomie [The role of glare and light scatter in the degradation of visual performance before and after Nd:YAG capsulotomy: a comparison of small and large size capsultomies]. Klin Monatsbl Augenheilkd 1994; 205: 65–69.
Goble RR, O'Brart DP, Lohmann CP, Fitzke F, Marshall J . The role of light scatter in the degradation of visual performance before and after Nd:YAG-capsulotomie. Eye 1994; 8: 530–534.
Yilmaz S, Ozdil MA, Bozkir N, Maden A . The effect of Nd:YAG laser capsulotomy size on refraction and visual acuity. J Refract Surg 2006; 9: 719–721.
Olsen G, Olson RJ . Update on a long-term, prospective study of capsulotomy and retinal detachment rates after cataract surgery. J Cataract Refract Surg 2000; 26: 1017–1021.
Jahn CE, Richter J, Jahn AH, Kremer G, Kron M . Pseudophakic retinal detachment after uneventful phacoemulsification and subsequent neodymium:YAG capsulotomy for capsule opacification. J Cataract Refract Surg 2003; 29: 925–929.
Lewis H, Singer TR, Hanscom TA, Straatsma BR . A prospective study of cystoid macular edema after neodymium:YAG laser posterior capsulotomy. Ophthalmology 1987; 94: 478–482.
Billotte C, Berdeaux G . Adverse clinical consequences of neodymium:YAG laser treatment of posterior capsule opacification. J Cataract Refract Surg 2004; 30: 2064–2071.
Holladay JT, Bishop JE, Lewis JW . The optimal size of a posterior capsulotomy. Am Intraocul Implant Soc J 1985; 11: 18–20.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no proprietary interest in any of the materials mentioned in this article and have received no financial support.
Rights and permissions
About this article
Cite this article
Hayashi, K., Nakao, F. & Hayashi, H. Influence of size of neodymium:yttrium-aluminium-garnet laser posterior capsulotomy on visual function. Eye 24, 101–106 (2010). https://doi.org/10.1038/eye.2009.41
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.41