Abstract
Objective
To investigate whether anxiety plays a role in self-recruitment for non-population-based glaucoma screening.
Methods
In a non-population-based pre-publicised trial, self-recruited Caucasian participants were screened for glaucoma, and also completed the Trait Anxiety Inventory and Shortened Health Anxiety Inventory questionnaires. In pre-publicity for the trial, information on risk factors for glaucoma was given. Participants classified as possible glaucoma cases later underwent a detailed glaucoma investigation.
Results
Of the 120 total participants (72 females, 48 males), 12 were considered glaucoma suspects at the screening, although only three (2.5%) were ultimately diagnosed with glaucoma. Health anxiety showed significant correlation with trait anxiety (r=0.525, P<0.001). Trait anxiety was similar for both the genders; this score was significantly below the normal Hungarian population value in women (P<0.001) and at the normal population level in men (P=0.560). In contrast, health anxiety was significantly higher than for both the ‘normal’ and ‘anxious’ reference groups (P<0.001), although smaller than that for hypochondriacs (P<0.001). Participants with pre-existing ocular symptoms, and those who attended because of fear of blindness, had significantly higher trait- and health-anxiety scores (P<0.05 for all comparisons).
Conclusion
In this screening trial, the health anxiety of the self-recruited participants was significantly above normal, whereas the prevalence of glaucoma was within the usual range for a Caucasian population. This suggests that providing pre-publicity information on risk factors for glaucoma does not necessarily increase the prevalence of glaucoma among self-recruited participants in non-population-based screening, as some individuals may participate on account of elevated health anxiety, rather than because of higher potential risk for glaucoma.
Similar content being viewed by others
Introduction
Glaucoma is one of the leading causes of severe visual impairment and blindness worldwide.1 The prevalence of chronic open-angle glaucoma is approximately 1.5–3% in Caucasians over 40 years of age.2, 3, 4, 5, 6, 7 As chronic open-angle glaucoma develops without clinical symptoms, it frequently happens that progression to the stage of severe damage may occur before the patient becomes aware of the disease. Even in the developed countries, it is estimated that 50% of glaucoma sufferers remain undetected.8, 9 Detection and treatment of early glaucoma is likely to provide a better long-term outcome than detection, and initiation of treatment, at a late stage. However, systematic, population-based mass screening for glaucoma is very expensive and even then, with the techniques used up to now, it is only moderately accurate.10, 11, 12 A less expensive approach is to provide free public glaucoma screening sessions, advertised in the media, at which self-recruited subjects with no visual symptoms can be screened. Such non-population-based screenings, however, can only be accurate if the diagnostic methods (or combination of methods) used have high positive likelihood ratio, and if the prevalence of glaucoma in the screened population is relatively high.13, 14 Thus, non-population-based glaucoma screening should ideally be focused on a target population with high risk for glaucoma.11, 13, 14, 15, 16 To increase the prevalence of glaucoma among the self-recruited participants (as compared with the general population), such screening sessions may need pre-publicity, and the information given should focus on the risk factors for chronic open-angle glaucoma, encouraging those with glaucoma risk factors to attend. Screening for a severe disease, however, can induce anxiety among potential participants, which might reduce their willingness to attend.17 On the other hand, subjects with elevated health anxiety, though without elevated glaucoma risk, may attend in over-representative numbers at the screening session after becoming aware of the publicised information. To our knowledge, this problem has not as yet been investigated. In this study, in an attempt to clarify the role of anxiety as a predictor factor in glaucoma screening participation, we investigated the trait anxiety and health anxiety levels of the participants in a pre-publicised public glaucoma screening event.
Patients and methods
Participants, screening methods and psychological tests
The screening protocol and the informed consent form were approved by the Institutional Review Board for Human Research of Semmelweis University, and all procedures adhered to the tenets of the Helsinki Declaration. Inclusion criteria for participation in the study consisted of the subject understanding and signing the informed consent form, and also of their being capable of understanding and responding to the questions in the sociodemographic and psychological tests. The availability of the free public glaucoma screening sessions (provided over a 4-day period including a weekend) was publicised in a general-information radio programme broadcast in the late morning. Participation in our screening session offered two special advantages. First, in Hungary at the time when the event was held (2007), patients, even though insured by the state health-care system, had to pay a fee for medical visits; thus, a normal visit to an ophthalmologist (in contrast to the screening event) was not free. Second, two of the four screening days were at the weekend, so that attendance was less likely to be restricted by the participant's working hours. The publicity (Table 1) also gave background information on the seriousness of the disease and its risk factors (age over 60 years, positive family history for glaucoma, myopia, visual-field deterioration), as well as on the treatment methods. The screening sessions were held in December 2007, in the Budapest headquarters of the Hungarian Federation for the Blind and Partially Sighted. The five-step ophthalmic examination protocol was performed in the following order: (1) standard decimal visual-acuity test from 5 m with determination of best refractive correction performed by a trained medical student; (2) recording of ophthalmic and general medical history, and a detailed slit-lamp examination performed by a glaucoma specialist (P.K.); (3) retinal nerve fibre layer measurement using the GDx-VCC equipment (Carl Zeiss Meditec Inc., Dublin, CA, USA) performed by a trained PhD student (M.T.); (4) IOP measurement with Goldmann applanation tonometry performed by a glaucoma specialist (P.K.) and (5) stereoscopic evaluation of the optic nerve head with a 90-diopter non-contact, aspheric lens after pupil dilation, the evaluation being performed by a glaucoma specialist (P.K.). Possible glaucoma was defined in terms of glaucomatous optic nerve head damage (diffuse or localised neuroretinal rim loss; notching; neuroretinal rim width differing from the normal pattern of inferior>superior>nasal>temporal; disc haemorrhage; baring of at least one circumlinear vessel at the edge of the neuroretinal rim area; retinal nerve fibre layer defect visible with green light; abnormal or borderline retinal nerve fibre layer thickness result with GDx-VCC), and/or intraocular pressure higher than 21 mmHg. Each participant with possible glaucoma on at least one eye was scheduled for detailed clinical examination in the Glaucoma Unit of the Department of Ophthalmology of Semmelweis University within 2 months from the date of screening. This detailed examination in the Glaucoma Unit comprised: diurnal IOP curve, central corneal thickness measurement, slit-lamp examination and optic nerve head evaluation, gonioscopy, and Octopus G2 automated threshold visual field testing, and was performed by the leader of the glaucoma team (G.H.). The final classification (glaucoma vs normal) and, in case of diagnosis of glaucoma, the classification of the type of glaucoma, was made by the same specialist (G.H.) for all the referred persons, based on the results of the detailed clinical examination using the standard criteria.13, 18
At the screening, before the above-described eye examinations each participant, with the assistance of trained psychologist interviewers, completed psychological and socioeconomic questionnaires. Trait anxiety was measured using the trait anxiety questionnaire of the Hungarian version of the State-Trait Anxiety Inventory (STAI), which has been validated for the Hungarian adult population.19 Health anxiety was measured using the Shortened Health Anxiety Inventory (SHAI), which was developed to identify and grade all forms and severity stages of health-related anxiety.20 The SHAI is able to identify and grade hypochondriasis, hypochondriasis with panic disorder, panic disorder alone and health anxiety. The SHAI has not yet been validated for the Hungarian population, but it is based on broad ranging patient and control populations involving substantial numbers of subjects. Depressive symptomatology was identified using the Hungarian version of the Shortened Beck Hopeless Scale.21, 22 A summary of the demographic details and socioeconomic status of the participants is shown in Table 2.
Statistical analysis
The Stata 8.1 software package was used for statistical analysis. The Shapiro–Wilk test was used to test for normal distribution of the anxiety scores. Results on trait anxiety and health anxiety were compared with those for the normal population and the reference groups using the unpaired t-test. One-way ANOVA with the Tukey test, the unpaired t-test or linear contrast in ANOVA (as appropriate) was used to compare mean values of trait anxiety and health anxiety in the different categories. Pearson's correlation coefficient was calculated to investigate the relationship between age and anxiety as well as between trait anxiety and health anxiety. Spearman's correlation coefficient was calculated to investigate the relationship between best-corrected visual acuity and anxiety. No correction for multiple testing was applied. P-values of 0.05 or lower were considered to indicate statistical significance.
Results
Each of the 120 self-recruited attendees (72 females, 48 males) completed the questionnaires. Twelve participants were considered as glaucoma suspects at the screening, but only three (2.5%) were ultimately diagnosed with glaucoma. Two of these newly detected cases had primary open-angle glaucoma in both the eyes, and the other person had secondary open-angle glaucoma (because of congenital cataract surgery in infancy) in one eye. Three further participants with no glaucomatous damage or symptoms underwent preventive laser iridotomy for occludable anterior chamber angle. Of the 75 participants with some previous ocular symptom or complaint, 62 indicated symptoms typical for ocular surface disorders, one experienced vitreous floaters, four reported uncorrected presbyopia, seven had clinically significant cataract, and one person reported an amaurosis fugax-like symptom in their respective histories.
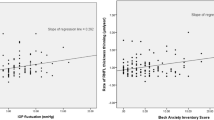
The score distributions for trait- and health anxiety showed no significant deviation from normality, as assessed by the Shapiro–Wilk test. The trait and health-anxiety scores of the participant population are summarised in Table 3. Trait anxiety and health anxiety showed significant correlation between each other (r=0.525, P<0.001; Figure 1); but neither of them was correlated with the age of the participants (r=0.024, P=0.792 and r=0.065, P=0.480, respectively). Trait anxiety was significantly lower than the corresponding normal population value in women (P<0.001), but did not differ from the normal value in men (P=0.560). In contrast, health anxiety was significantly elevated compared both with the ‘normal’ and ‘anxious’ reference groups (P<0.001), but was lower than that in the ‘hypochondriac’ reference group (P<0.001). The relationships between trait anxiety, health anxiety and the different socioeconomic variables are shown in Table 2. Participants who had previous ocular symptoms or complaints had higher trait- and health-anxiety scores than those who had no such symptoms (42.10±9.11 vs 38.56±8.22, P=0.039; and 32.85±6.43 vs 30.27±5.34, P=0.025, respectively). Best-corrected visual acuity of the left eye showed a significant negative correlation with health anxiety (r=−0.251, P=0.006) but not with trait anxiety (r=−0.084, P=0.365). For the right eye, no correlation was seen between best-corrected visual acuity and anxiety (r=−0.084, P=0.364 and r=0.046, P=0.618, respectively). The scores for both trait- and health anxiety of those who participated because of ‘fear of blindness’ were significantly higher than the scores for those who indicated ‘awareness of the importance of screening’ as the reason for attending the screening trial (43.49±8.67 vs 38.16±7.89, P=0.003; and 34.17±7.39 vs 29.68±4.80, P=0.021, respectively). Participants reporting severe visual impairment (from any cause) among their close relatives showed elevated trait anxiety (42.92±7.98 vs 38.55±9.10, P=0.007), but no increase of health anxiety (32.50±5.55 vs 31.20±6.53, P=0.253), compared with those with no such problems in the close family. The other socioeconomic variables, as well as the presence or absence of depressive symptoms (based on the responses to the Shortened Beck Hopeless Scale), were not found to have any influence on trait anxiety or health anxiety (Table 2).
Discussion
In this study, we investigated whether anxiety plays a role in self-recruited participation in non-population-based, pre-publicised glaucoma screening. The reason for this investigation was that non-population-based public glaucoma screening is frequently organised in different communities, and recent data suggest that by combining different diagnostic methods and/or criteria, the accuracy and the positive likelihood ratio of the screening can be significantly increased.13, 14 However, as the prevalence of glaucoma in the adult Caucasian general population is far below the value optimal for screening,2, 3, 4, 5, 6, 7 it is very desirable to increase the prevalence of glaucoma among the self-recruited screening participants.11, 13 To specifically motivate persons to attend who have a high probability of having the disease, information on the risk factors for glaucoma needs to be provided when the screening event is publicised in the media. Such publicity information may, however, also motivate some low-risk individuals, but who have elevated health anxiety, to attend. If this does happen to a marked extent, the overall prevalence of glaucoma among the screened subjects may not be increased as desired, which can in turn result in decreased screening accuracy.
In our screening exercise, detailed information on the significance of and risk factors for glaucoma was given in a radio programme broadcast before the screening event. In fact, however, the prevalence of glaucoma among the self-recruited attendees was only 2.5%, which is within the usual prevalence limits found for Caucasian adults over 40 years of age.1, 2, 3, 4, 5, 6, 7 Thus, emphasising the risk factors for glaucoma in the radio broadcast apparently did not in this case result in the desired higher-than-normal prevalence of glaucoma among the screened participants, even though their age (mean age: 65 years) was indeed within the targeted range. As regards the psychological characteristics of the participants, trait anxiety, which reflects the general aspect of a person's anxiety level,19 was not elevated in comparison to the population-based value. But we found that the other measured variable, health anxiety, was very significantly elevated as compared with the ‘healthy’ reference group, or even the ‘anxious’ reference group.20 Although determination of the population-based normal health-anxiety scores has not yet been completed, we are confident that there is no systematic difference between our population and the reference groups,20 which consist of separate normal and patient populations each of several hundred persons. The health-anxiety score on the Shortened Health Inventory specifically quantifies anxiety caused by the given person's propensity to misinterpret bodily variations and health-related medical information, and represents anxiety resulting from a hypothetical serious physical disease.20 Thus, trait anxiety and health anxiety represent different categories, the mean values for which can differ from each other. This was seen in the results for our self-recruited attendees, even though there was significant positive correlation between the trait- and the health-anxiety scores.
We did not correct for multiplicity and, thus, some caution may be appropriate in interpreting our results. However, we believe our conclusion to be clinically meaningful as described below. As our screening trial addressed an eye disease, it is of course not surprising that participants who had previously experienced some ocular symptom or complaint represented two thirds of the attendees (Table 2), and that these had higher anxiety scores than those who did not report any such problem. Similarly, those who participated only because of fear of blindness (n=35) had significantly higher anxiety scores than those in the other group (n=45) who participated only because of awareness of the importance of glaucoma screening. Considering the fact that the mean best-corrected visual acuity for the participants was in fact reasonably good (better than 0.7 for both the left and right eyes), and in addition that state-provided ocular health care was available for all the tested participants, the fear of blindness as a motivation for attendance appears not to be supported by rational factors. In addition, it is interesting that those who reported visual impairment because of any eye disease among their close relatives (n=52) showed significantly elevated trait anxiety, as compared with those who did not report on such a circumstance (n=66), even though health anxiety did not differ significantly between these two subgroups. The ophthalmologically neutral demographic and socioeconomic variables, and the presence or absence of depressive symptoms, had no influence on the anxiety scores. The fact that, in addition, reported confidence in successful treatment of glaucoma had no influence on the anxiety scores suggests that the publicity information on glaucoma treatment had played a limited role in the decision to participate in the screening trial.
Our study has a number of limitations because of its design and the relatively small number of participants. As our participants were all Caucasians, no conclusion from our results can be derived in respect of other ethnic groups. Because of the non-population-based nature of the study, the results cannot be considered valid for the rural population or the entire adult Hungarian population, or for Caucasians in general. Further studies with more participants are necessary to clarify whether the results of the present investigation can be considered typical for non-population-based, pre-publicised glaucoma screening sessions. Whether other types of publicity may be more advantageous for the recruitment of participants with increased prevalence of glaucoma also remains to be specified. We are not aware of any other published investigation with similar design, and thus comparison with other similar studies was not possible.
In summary, in our non-population-based glaucoma screening trial, the health-anxiety score of the self-recruited participants was significantly increased, whereas the actual prevalence of glaucoma was within the normal range for a Caucasian population. This result suggests that providing information on the risk factors for glaucoma during the pre-publicity for such an event does not necessarily result in an above-average prevalence of glaucoma among self-recruited participants in non-population-based screening, as is the intention. It appears that some individuals may participate because of their elevated health anxiety, rather than because of having an elevated risk for glaucoma. This suggests that attaining a higher-than-normal prevalence of glaucoma among the screened population (which is needed for good screening accuracy) at a pre-publicised screening event may be difficult to achieve. Thus, our present results appear to support the position that in Caucasian subjects case finding screening trials that provide information on the risk factors for glaucoma may not represent an ideal approach for the detection of glaucoma.
References
Quigley HA, Broman AT . The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol 2006; 90: 262–267.
The Eye Diseases Prevalence Research Group. Prevalence of open-angle glaucoma among adults in the United States. Arch Ophthalmol 2004; 122: 532–538.
Bonomi L, Marchini G, Marraffa M, Bernardi P, De Franco I, Perfetti S et al. Prevalence of glaucoma and intraocular pressure distribution in a defined population: The Egna-Neumarkt study. Ophthalmology 1998; 105: 209–215.
Tielsch JM, Sommer A, Katz J, Royall RM, Quigley HA, Javitt J . Racial variations in the prevalence of primary open-angle glaucoma: the Baltimore Eye survey. JAMA 1991; 266: 369–374.
Wolfs RCW, Borger PH, Ramrattan RS, Klaver CC, Hulsman CA, Hofman A et al. Changing views on open-angle glaucoma: definitions and prevalences—The Rotterdam study. Invest Ophthalmol Vis Sci 2000; 41: 3309–3321.
Antón A, Andrada MT, Mujica V, Calle MA, Portela J, Mayo A . Prevalence of primary open-angle glaucoma in a Spanish population: the Segovia study. J Glaucoma 2004; 13: 371–376.
Nizankowska MH, Kaczmarek R . Prevalence of glaucoma in the Wroclaw population. The Wroclaw epidemiological study. Ophthalmic Epidemiol 2005; 12: 363–371.
Quigley HA . Number of people with glaucoma worldwide. Br J Ophthalmol 1996; 80: 389–393.
Topouzis F, Coleman AL, Harris A, Koskosas A, Founti P, Gong G et al. Factors associated with undiagnosed open-angle glaucoma: the Thessaloniki Eye Study. Am J Ophthalmol 2008; 145: 327–335.
Wong EYH, Keeffe JE, Rait JL, Vu HT, Le A, McCarty C et al. Detection of undiagnosed glaucoma by eye health professionals. Ophthalmology 2004; 111: 1508–1514.
Quigley HA, Park CK, Tracey PA, Pollack IP . Community screening for eye disease by laypersons: the Hoffberger Program. Am J Ophthalmol 2002; 133: 386–392.
Wilson MR . Screening paradigms in glaucoma. J Glaucoma 2001; 10 (Suppl 1): S25–S27.
Tóth M, Kóthy P, Vargha P, Holló G . Accuracy of combined GDx-VCC and Matrix FDT in a glaucoma screening trial. J Glaucoma 2007; 16: 462–470.
Kumar S, Giubilato AG, Morgan W, Jitskaia L, Barry C, Bulsara M et al. Glaucoma screening: analysis of conventional and telemedicine-friendly devices. Clin Exp Ophthalmol 2007; 35: 237–243.
Harasymowycz PJ, Papamatheakis DG, Fansi AK, Gresset J, Lesk MR . Validity of screening for glaucomatous optic nerve damage using confocal scanning laser ophthalmoscopy (Heidelberg Retina Tomograph II) in high-risk populations: a pilot study. Ophthalmology 2005; 112: 2164–2171.
Hernandez R, Burr JM, Vale LD . Economic evaluation of screening for open angle glaucoma. Int J Technol Assess Health Care 2008; 24: 203–211.
Brown Sofiar J, Lehlbach M . The role of anxiety in a mammography screening program. Psychosomatics 2008; 49: 49–55.
European Glaucoma Society. Terminology and Guidelines for Glaucoma, 2nd ed. DOGMA s.r.l., Savona, 2008.
Sipos K, Sipos M . The development and validation of the Hungarian form of the STAI. In: Spielberger CD, Guerrero D (eds). Cross-Cultural Anxiety, 2nd ed. Hemisphere Publ. Corp.: Washington-London, 1978, pp 51–56.
Salkovskis PM, Rimes KA, Warwick HMC, Clark DM . The Health Anxiety Inventory: development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychol Med 2002; 32: 843–853.
Rózsa S, Szádóczky E, Füredi J . Validation of the shortened version of BDI. Psychiatria Hungarica 2001; 16: 384–402.
Perczel Forintos D, Sallai J, Rózsa S . Reliability and validity of the Beck Hopeless Scale. Psychiatria Hungarica 2001; 16: 632–643.
Acknowledgements
The authors thank Márta Tóth for her assistance in the clinical examinations, and Cecilia Hlavács, Kornélia Németh, Katalin Lányi and Nikoletta Pázmándi for their assistance in administration and evaluation of the questionnaires. Supported by Hungarian National Health Grant (ETT) 001/2009 (Dr Holló).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author declares no conflict of interest..
Rights and permissions
About this article
Cite this article
Holló, G., Kóthy, P., Géczy, A. et al. Health anxiety in a non-population-based, pre-publicised glaucoma screening exercise. Eye 24, 699–705 (2010). https://doi.org/10.1038/eye.2009.131
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.131