Abstract
Purpose
To determine the effectiveness of staining an epiretinal membrane (ERM) with triamicinolone acedonide (TA) during vitrectomy for a retinal detachment (RD) due to a macular hole (MH) in highly myopic eyes.
Patients and methods
Thirty-four highly myopic eyes (>−6.0 dioptres) of 34 patients with an RD caused by an MH underwent vitrectomy with TA-assisted ERM removal. The excised ERMs from five eyes were examined by transmission electron microscopy (TEM). The main outcome measures were the retinal status and best-corrected visual acuity (BCVA). The anatomic status of the MH was determined by optic coherence tomography (OCT) in 24 successfully retinal-reattached eyes. The follow-up periods ranged from 5 to 20 months.
Results
The granules of TA adhered to the ERM and the residual posterior hyaloid, which made them more visible and facilitated their removal. Tissues resembling the internal limiting membrane were not detected in any of the five excised tissues. The retinal reattachment rate was 88% after the first surgery. The mean log MAR BCVA significantly improved from 1.83±0.50 (mean±SD) before surgery to 1.22±0.35 at the final follow-up (P<0.001, Wilcoxon signed rank test). OCT showed a normal concave appearance in 11 of 24 eyes (46%), but a central neural epithelial defect was present in 13 of 24 eyes (54%).
Conclusions
TA facilitates the complete removal of both the ERM and residual posterior hyaloid, thus ensuring high anatomical and visual success rates in highly myopic eyes with an RD due to MH.
Similar content being viewed by others
Introduction
The retinal detachment (RD) due to a macular hole (MH) in highly myopic eye is a special type of RD and can lead to severe vision decrease if not appropriately treated. A tangential traction of the macular area is believed to be a major factor although the mechanism causing the MH-RD in highly myopic eyes is still not been conclusively determined.1, 2, 3, 4, 5, 6, 7
Pars planar vitrectomy (PPV) with the removal of a macular epiretinal membrane (ERM) and gas tamponade is a common and effective method to treat the RD caused by an MH in highly myopic eyes. The complete removal of the ERM has been shown to lead to a high success rate of 84–100%, and to reduce the incidence of a reopening of the MH and resultant RD.3, 4, 5 To ensure the complete removal of ERM during surgery, the internal limiting membrane (ILM) has been removed with or without staining with indocyanine green (ICG) or by using a diamond-dusted membrane brush. These procedures have led to a success rate of 93.2–100%.6, 7, 8
Peyman et al9 were the first to report that an intravitreal injection of triamicinolone acedonide (TA) during vitrectomy made the ERM more visible and facilitated the complete removal of not only the ERM but also residual posterior hyaloid during the surgery. Since then, Yamamoto et al10 and Sakaguchi et al11 have described the usefulness of TA during vitrectomy for treatment of RD due to an MH in small series of highly myopic eyes and reported a 100% successful rate after the first surgery. However, Yamamoto and co-workers10 examined only six eyes, and Sakaguchi et al11 reported only one case. Thus, more data are needed to determine the efficacy of TA during vitrectomy for treatment of RD due to an MH.
The purpose of this study was to determine the effectiveness and safety of staining the ERM with TA during vitrectomy for an RD due to an MH in highly myopic eyes.
Patients and methods
The medical records of 34 eyes of 34 consecutive highly myopic patients (range, −6 to −23 dioptres (D)) who had undergone PPV with TA-assisted ERM removal for an RD due to an MH from November 2005 to March 2007 were reviewed.
Approval of the study was obtained from the Ethics Committee of the second Affiliated Hospital of Zhejiang University and included permission to collect and analyse histological samples. The risks and benefits of the surgery were described in detail to each patient, and a written informed consent was obtained from each patient prior to the surgery in accordance with our institutional procedures.
All patients had a thorough ocular examination preoperatively. The preoperative data recorded from the patients included age, gender, eye affected, refractive error, best-corrected visual acuity (BCVA) by Snellen, estimated duration of the visual symptoms, axial length, lens status, presence of a posterior vitreous detachment (PVD), an ERM, presence of a staphyloma, and the extent of the RD. The presence of a staphyloma was confirmed by B-mode ultrasonography. A PVD was determined to be present by the detection of a Weiss ring.
A conventional three-port PPV with TA-assisted ERM removal was performed in each eye. Simultaneous phacoemulsification for a cataract with/without posterior-chamber intraocular lens implantation was performed on three eyes. After the central vitreous was excised, a posterior fluid cavity was encountered. The posterior vitreous hyaloid was separated from the retina by active aspiration with the vitrectomy probe and any visible vitreous strands that were adherent to the retina were removed.
To prepare the suspension of TA, a single-use 1-ml vial of TA suspension (Kenalog-40; Bristol–Meyers Squibb) was centrifuged for 5 min at 1000 r.p.m. The supernatant was removed and one millilitre of balanced salt solution (BSS; Alcon) was added to the bottle. Just before use, the bottle was vigorously shaken, and 0.1 ml of the solution (4 mg/0.1 ml) was withdrawn and carefully injected into the posterior vitreous cavity over the posterior pole, with the infusion temporarily stopped. The TA was washed out after approximately 1–2 min. In some eyes with an extensive RD, subretinal fluid was drained through the MH to flatten the detached retina prior to the TA injection.
The extent of the ERM and residual posterior hyaloid was observed after TA injection. A microhooked needle (20-gauge) was used to create a flap of the ERM along the posterior retinal surface. Then, a horizontal forceps was used to grasp the flap, and the ERM was removed in a curvilinear fashion. The residual posterior hyaloid was subsequently separated from the retina and cut as far peripherally as possible. The peripheral retina was carefully examined for retinal breaks with scleral depression. Fluid–air exchange was then performed with simultaneous drainage of subretinal fluid though the MH. Subsequently, 14% perfluoropropane (C3F8) was used to tamponade the retina. Retinal laser coagulation was not performed around the MH in any case.
The excised ERMs from five eyes were transferred to a vial containing 2% glutaraldehyde in 0.1 M phosphate buffer and fixed for transmission electron microscopy (TEM). After surgery, all of the patients were instructed to maintain a face-down position for 2 weeks. The postoperative outcomes included the anatomic results, BCVA, and the postoperative complications.
Optical coherence tomography (Stratus OCT; Carl Zeiss Meditee, Dublin, CA, USA) was used to evaluate the morphology of the retina and MH in 24 successfully reattached eyes.
The preoperative and postoperative BCVA was converted to logarithm of the minimal angle of resolution. The preoperative BCVA of counting fingers and hand motion were considered to be 20/2500 and 20/5000, and were converted to log MAR 2.1 and 2.4 units. An improvement or reduction in the visual acuity was defined as change ⩾0.2 log MAR units. Wilcoxon signed rank test was used to analyse the preoperative and postoperative BCVA. A P-value <0.05 was considered significant.
Results
Thirty-four eyes of 34 patients were studied. There were 21 women and 13 men, and their mean age was 57.7±9.1 years (mean±standard deviation (SD), range, 36–71 years). There were 19 right eyes and 15 left eyes, and the mean duration of the visual symptoms was 6.4±5.3 months (range, 2–20 months). The mean axial length was 28.5±1.8 mm (range, 27.0–31.5 mm). The extent of the RD was posterior pole, 3 eyes; posterior pole +1 quadrant, 12 eyes; posterior pole +2 quadrants, 8 eyes; posterior pole+ 3 quadrants, 9 eyes; and total, 2 eyes. A PVD was observed in 10 eyes, and an ERM in 5 eyes. Thirty-one eyes were phakic and three eyes were pseudophakic.
During the surgery, a thin sheet of tissue, the ERM, was clearly observed overlying the macular and posterior staphyloma after it was made visible by the white-coloured TA granules in 33 of 34 eyes. The increased visibility of the membrane greatly facilitated its complete removal as a sheet. The ERM around the staphyloma was found to extend towards the posterior hyaloid. The residual posterior hyaloid beyond the ERM and in the periphery was also made visible by TA granules and was easily separated from the retina and incised with the vitreous cutter as far peripherally as possible (Figure 1a–e).
Intraoperative view of the fundus in a highly myopic eye with a retinal detachment (RD) due to a macular hole (MH). (a) RD due to an MH can be seen prior to the injection of TA. No obvious ERM can be seen. (b) After the intravitreal injection of TA, white granules can be seen on the surface of a previously undetected thin ERM. Granules can also be seen on the posterior staphyloma. A microhooked needle was used to grasp a flap of the ERM to separate it from the underlying membrane. (c) Surgical forceps hold and peel the ERM around the MH. The edge between the peeled and unpeeled membrane can be seen. (d) Continued peeling of the ERM on the posterior staphyloma by surgical forceps. (e) Vitrectomy probe is used to aspirate and cut the epiretinal membrane and residual posterior hyaloid.
The mean postoperative follow-up period was 11.7±5.2 months (range, 5–20 months). The retina was anatomically reattached in 30 (88%) of 34 eyes and remained detached in four (12%) eyes after the first surgery. In two of these four failed eyes, a retinal redetachment occurred with unclosed MH in one eye and a small newly formed hole near the inferior margin of the posterior staphyloma in the other eye. Both eyes were treated with additional gas injection and laser coagulation, and the retina was ultimately reattached. The other two eyes developed a retinal redetachment at 6 and 12 months after surgery because of a reopening of the MH. These two cases refused to undergo a second operation.
The preoperative and final postoperative BCVAs in the 30 initially successful eyes were compared. The mean preoperative BCVA was 1.94±0.45 log MAR units, and the final mean postoperative BCVA significantly improved to 1.27±0.34 log MAR units (P<0.001, Wilcoxon signed rank test). The postoperative BCVA was improved in 25 of 30 eyes (83%) and unchanged in 5 of 30 eyes (17%). A scattergram of the preoperative and postoperative BCVA of the 30 initially successful eyes is shown in Figure 2.
A scattergram of the preoperative and postoperative log MAR Snellen best-corrected visual acuity of 30 initially successful eyes. The preoperative BCVA of counting fingers and hand motion was considered to be 20/2500 and 20/5000, respectively. These values were converted to log MAR 2.1 and 2.4 units.
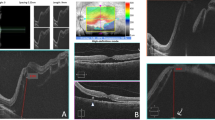
The morphology of the postoperative macula was evaluated by optic coherence tomography (OCT) in 24 eyes with an anatomical reattachment. OCT showed that the macula had a normal concave configuration in 11 of the 24 eyes (46%), and the margins around the MH in the other 13 cases (54%) were firmly attached to the underlying RPE but a central defect of the neural retina was present. A very shallow local RD was detected near the closed MH in 2 of 24 eyes (9%). Tiny folds on the retina pointing to the vitreous cavity were detected near the fovea in 3 of 24 cases (13%; Figure 3a–d).
Optical coherence tomographies of the macula during the follow-up period. (a) Retina is reattached postoperatively and the normal concave configuration of macula can be seen (arrow). (b) The margin of the MH is adherent to the RPE but a central neural epithelium defect can be seen (arrow). (c) The previous MH showed normal concave configuration but an RD in the parafoveal region is still present (arrow). (d) The circumference of the previous MH is adherent to the RPE but two small parafoveal minor folds pointing to vitreous cavity can be seen (arrows).
TEM showed that the excised ERM was made up of one or more cellular layers. Fibroblast-like cells, a collagen matrix, and cellular debris were observed. Tissues resembling the ILM were not detected in any of the five excised tissues (Figure 4a–c).
Tiny amounts of TA granule were seen in the subretinal space during the operation in all 34 eyes, but most were aspirated during the fluid–air exchange. TA granules left in the subretinal space were completely absorbed during the follow-up period.
There was no infectious endophthalmitis or elevated ocular pressure during the follow-up period.
Discussion
Vitrectomy with ERM removal and gas tamponade has become a common and effective method for MH-RD in highly myopic eye.3, 4, 5, 6, 7, 8 Oshima et al3 reported that the initial success rate was 90.9%, and the recurrence rate was 9.1% in 11 eyes with complete ERM removal using a diamond-dust silicone cannula. On the other hand, the success rate was 6.7% and the recurrence rate was 83.3% in six eyes with incomplete ERM removal. Seike et al4 reported that the initial success rate was 100% with no re-opening of the MH in five eyes with a complete removal of the ERM, whereas the success rate was 20% and the re-opening rate was 80.0% in six eyes with an incomplete removal of the ERM. Chen et al12 reported a success rate of 50%, and they attributed the low success rate to the incomplete removal of the ERM because they found it difficult to grasp and remove the ERM. TA was not used during the surgery in any of these reports. Taken together, these findings indicate that a complete removal of the ERM during vitrectomy is critical for the successful closure of the MH with fewer re-opening of the MH (Table 1).
Our success rate was 88% after the initial surgery. The complete removal of the ERM and residual posterior hyaloid with the TA during the surgery most likely contributed to our favourable results.
An accurate identification of an ERM is essential for its complete removal. However, in most cases, the ERM is thin, translucent, and difficult to identify and remove with conventional membrane-peeling instruments.3, 4, 10, 12 To facilitate the complete removal of the ERM, a diamond-dusted membrane scraper or ICG staining with ILM peeling has been reported to help.3, 7, 13 In our study, most of the ERMs were not visible prior to the TA injection and might have been overlooked and left attached to the retina. However, the white-coloured granules of TA stuck to the rough surface of the ERM and the residual vitreous, thus delineating the ERM, which ensured the complete removal of the ERM and the residual posterior hyaloid. The beneficial effect of TA during the MH-RD surgery in highly myopic eye was also reported by Yamamoto et al.10
Although high success rates have been reported after ILM peeling during vitrectomy for MH-RD in highly myopic eyes,7, 8, 14 we did not intentionally peel the ILM for the following reasons. First, we assumed that the TA-assistant ERM removal ensured the complete removal of the overlying residual posterior hyaloid and ERM, which had not been seen before the TA injection. The removal should release any traction caused by the residual premacular vitreous or ERM. Second, it has still not been determined whether the ILM around an MH should be removed during vitrectomy because of the unknown long-term effects and adverse effects of ILM peeling.15, 16 Third, it is technically difficult to peel the thin and fragile ILM off the detached retina in highly myopic eyes. Our high success rate demonstrated the importance of the complete removal of ERM and suggests that the intentional ILM removal maynot be needed during the initial surgery for RD with an MH in highly myopic eyes.
The use of OCT and cross-sectional images of the retina has been valuable in determining the anatomic status of an MH in highly myopic eyes, which are otherwise undetectable by conventional ophthalmoscope because of the severe degenerative myopic changes in the posterior pole. Thus, Ikuno17 reported that only 7 of the 16 highly myopic eyes (44%) had a normal concave configuration of the macula using OCT, even though all of the retinas were reattached after surgery. In another similar OCT study,18 the rate of MH closure was found to be only 10%. In our series, OCT showed that the fovea recovered to a normal concave configuration in 11 cases (46%), and the entire circumference of the MH was pressed against the RPE but a central neural epithelial defect remained or a very shallow parafoveal RD persisted in the other 13 cases (54%). Taken together, these results showed that even with a reattachment of the retina, most of the maculas do not recover their normal anatomical configuration in highly myopic eyes.
Our OCT images showed some minor folds with the peaks pointing to the vitreous cavity in three cases (12%). Ikuno et al19 reported that the incidence of the minor parafoveal folds was 24, 43, and 62% after 1, 3, and 6 months respectively. After examining three-dimensional OCT images, they suggested that the minor folds might result from a weak traction caused by an imbalance in the extension of retinal vessels and retinal tissues during the development of a posterior staphyloma.
Only tiny amounts of TA granule were left in the subretinal space after the operation in all the 34 eyes in our study. The TA granules were completely absorbed and the BCVA improved during the follow-up, suggesting that no serious damage to the retina occurred. Many reported clinical experiences have demonstrated that intravitreal use of TA during vitrectomy does not affect the closure rate and visual function although conflicting laboratory data about TA toxicity to the retina and RPE have been presented.20, 21, 22, 23, 24
TA-associated complications, such as elevated intraocular pressure, were not found in any of our cases. The three patients who developed a cataract during the follow-up period were most likely not related to the use of TA.
There are several limitations for our study. Not all of the operated eyes were followed up by OCT postoperatively, and only five excised specimens were collected for TEM. Several studies have shown that ILM fragments were present in the excised ERM specimens from highly myopic eye with RD due to an MH.10, 11 Thus, we cannot exclude the possibility of ILM fragments being attached to the excised ERM specimens. In addition, the follow-up period was short, and a control group is lacking in this study. Further controlled studies and longer follow-up are needed to support our conclusions.
In conclusion, vitrectomy with TA-assisted removal of the entire ERM and gas tamponade is an effective surgical procedure for the attachment of an RD due to an MH in highly myopic eyes. The intravitreal use of TA is safe and effective because it delineates the entire ERM and facilitates the complete removal of both the ERM and residual posterior hyaloid.
References
Marmor MF . Mechanisms of normal retinal adhesion. In: Ryan SJ, Glaser BM (eds). Retina, 2nd ed. Mosby-Year Book Inc.: St Louis, Missouri, 1994; 1931–1953.
Stripe M, Michels RG . Retinal detachment in highly myopic eyes duo to macular holes and epiretinal traction. Retina 1990; 10: 113–114.
Oshima Y, Ikuno Y, Motokura M, Nakae K, Tano Y . Complete epiretinal membrane separation in highly myopic eyes with retinal detachment resulting from a macular hole. Am J Ophthalmol 1998; 126: 669–676.
Seike C, Kusaka S, sakagami K, Ohashi Y . Reopening of macular holes in highly myopic eyes with retinal detachments. Retina 1997; 17: 2–6.
Uemoto R, Saito Y, Sato S, Imaizumi A, Tanaka M, Nakae K . Better success of retinal reattachment with long-standing gas tamponade in highly myopic eyes. Greafes Arch Clin Exp Ophthalmol 2003; 241: 792–796.
Kadonosono K, Yazama F, Itoh N, Uchio E, Nakamura S, Akura J et al. Treatment of retinal detachment resulting from myopic macular hole with internal limiting membrane removal. Am J Ophthalmol 2001; 131: 203–207.
Kusaka S, Hayashi N, Ohji M, Hayashi A, Kamei M, Yano Y . Indocyanine green facilitates removal of epiretinal and internal limiting membranes in myopic eyes with retinal detachment. Am J Ophthalmol 2001; 131: 388–390.
Uemoto R, Yamamoto S, Tsukahara I, Takeuchi S . Efficacy of internal limiting membrane removal for retinal detachments resulting from a myopic macular hole. Retina 2004; 24: 560–566.
Peyman GA, Cheema R, Conway MD, Fang T . Triamcinolone acetonide as an aid to visualization of the vitreous and the posterior hyaloids during pars planar vitrectomy. Retina 2000; 20: 554–555.
Yamamoto N, Ozaki N, Murakami K . Triamcinolone acetonide facilitates removal of the epiretinal membrane and separation of the residual vitreous cortex in highly myopic eyes with retinal detachment duo to a macular hole. Ophthalmologica 2004; 218: 248–256.
Sakaguchi H, Ikuno Y, Choi JS, Ohji M, Tano Y . Multiple components of epiretinal tissues detected by triamcinolone and Indocyanine Green in macular hole and retinal detachment as a result of high myopia. Am J Ophthalmol 2004; 138: 1079–1081.
Chen YP, Chen TL, Yan KR, Lee WH, Kuo Y H, Chao AN et al. Treatment of retinal detachment resulting from posterior staphyloma-associated macular hole in highly myopic eyes. Retina 2006; 26: 25–31.
Fang X, Chen Z, Weng Y, Shu Z, Ni H, Jiang J et al. Surgical outcome of idiopathic macular epiretinal membrane in young patients. Eye 2007; e-pub ahead of print 31 August 2007.
Ichibe M, Yoshizawa T, Murakami K, Ohta M, Oya Y, Yamamoto S et al. Surgical management of retinal detachment associated with myopic macular hole: anatomic and functional status of the macula. Am J Ophthalmol 2003; 136: 227–284.
Kuhn F . Point: to peel or not to peel, that is the question. Ophthalmology 2002; 109: 9–11.
Hassan TS, Williams GA . Counterpoint: to peel or not to peel: is that the question? Ophthalmology 2002; 109: 11–12.
Ikuno Y, Sayanagi K, Oshima T, Gomi F, Kusaka S, Kamei M et al. Optical coherence tomographic findings of macular holes and retinal detachment after vitrectomy in highly myopic eyes. Am J Ophthalmol 2003; 136: 477–481.
Lam RF, Lai WW, Cheung BT, Yuen CY, Wong TH, Shanmugam MP et al. Pars planar vitrectomy and perfluoropropane (C3F8) tamponade for retinal detachment due to myopic macular hole: a prognostic factor analysis. Am J Ophthalmol 2006; 142: 938–944.
Ikuno Y, Komi F, Tano Y . Potent retinal arteriolar traction as a possible cause of myopic foveoschisis. Am J Ophthalmol 2005; 139: 462–467.
Takeuchi M, Katagiri Y, Usui M . Residual triamcinolone acetonide in the macular hole after vitrectomy. Am J Ophthalmol 2003; 136: 1174–1176.
Takasu I, Shiraga F, Otsuki H . Triamcinolone acetonide-assisted internal limiting membrane peeling in macular hole surgery. Retina 2004; 24: 620–622.
Kampougeris G, Cheema R, McPherson R, Gorman C . Safety of Triamcinolone acetonide (TA)-assisted pars plana vitrectomy in macular hole surgery. Eye 2007; 21: 591–594.
Change YS, Wu CL, Tseng SH, Kuo PY, Tseng SY . Cytotoxicity of triamcinolone acetonide on human retinal pigment epithelial cells. Invest Ophthalmol Vis Sci 2007; 48: 2792–2798.
Szurman P, Sierra A, Kaczmarek R, Jaissle GB, Wallenfel-Thilo B, Grisanti S et al. Different biocompatibility of crystalline triamcinolone deposits on retinal cells in vitro and in vivo. Exp Eye Res 2007; 85: 44–53.
Acknowledgements
This work was supported by a grant from the national natural science foundation (no. 60671005), China.
Author information
Authors and Affiliations
Corresponding author
Additional information
Proprietary interest: None
Rights and permissions
About this article
Cite this article
Fang, X., Zheng, X., Weng, Y. et al. Anatomical and visual outcome after vitrectomy with triamcinolone acedonide-assisted epiretinal membrane removal in highly myopic eyes with retinal detachment due to macular hole. Eye 23, 248–254 (2009). https://doi.org/10.1038/eye.2008.60
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2008.60
Keywords
This article is cited by
-
Inverted internal limiting membrane flap technique for retinal detachment due to macular holes in high myopia with axial length ≥ 30 mm
Scientific Reports (2022)
-
Vitreo-retinal relationship and post-operative outcome of macular hole repair in eyes with high myopia
Graefe's Archive for Clinical and Experimental Ophthalmology (2016)
-
Optical coherence tomographic characteristics and surgical outcome of eyes with myopic foveoschisis
Eye (2009)