Abstract
Purpose
To investigate whether new classes of glaucoma medication have influenced glaucoma filtration surgery over a 20-year period in the southeast region of Ireland.
Methods
All patients undergoing glaucoma filtration surgery between January 1986 and December 2005 in Waterford Regional Hospital were identified. The following data were recorded for each patient: age; sex; and type of filtration procedure.
Results
Over the 20-year study period two consultant ophthalmic surgeons performed a total of 760 glaucoma filtration procedures on patients aged over 20 years. The annual average number of glaucoma surgeries declined steadily, defined by availability of different topical anti-glaucoma medications, from an average of 23.75 surgeries per surgeon per year in the subperiod 1986–1995, to 21 in 1996, 20 in 1997, and 12.69 surgeries per surgeon per year in 1998–2005, these differences being statistically significant (general linear model, P<0.001). The age profile of patients did not change significantly over the course of the study period.
Conclusions
The volume of patients requiring glaucoma filtration surgery under the care of two consultant ophthalmic surgeons decreased over the 20-year study period, an era in which three classes of anti-glaucoma medications were made available. However, an increase in the age profile of patients undergoing glaucoma filtration surgery during the same period was not observed. Further study is required to resolve whether introduction of the new topical anti-glaucoma medications has led to a real reduction in the demand for glaucoma filtration surgery, or has just led to the deferral of such a demand.
Similar content being viewed by others
Introduction
Glaucoma, one of the most common causes of blindness worldwide, may be defined as ‘a characteristic form of optic neuropathy, with some regard to intraocular pressure.’1 In 2003, in the Republic of Ireland (RoI), glaucoma accounted for 12% of all cases of blind registration.2
Intraocular pressure (IOP) is the leading risk factor for, and remains the only modifiable feature of, glaucoma. Therefore, IOP reduction remains the primary aim for management of this condition.
Medical therapies available for lowering IOP may be classed as topical or systemic, the latter being reserved for short-term use only.3 Topical anti-glaucoma medications include β-blockers, prostaglandin analogues, miotics, carbonic anhydrase inhibitors, and α-agonists.4 Glaucoma filtration surgery for glaucoma is generally reserved for those cases where disease progression is observed in spite of maximal tolerable medical therapy.4
Given that many topical anti-glaucoma medications have become available to ophthalmologists only in the last 10–15 years, we designed a study to investigate the impact of availability of these medications on the volume and age profile of patients undergoing glaucoma filtration surgery over a 20-year period, and whether any observed changes in either of these outcomes relate to the availability of topical anti-glaucoma medications.
Materials and Methods
The surgical logbooks of the ophthalmic theatres in Waterford Regional Hospital were reviewed for all glaucoma filtration procedures performed between January 1986 and December 2005. From 1986 to 1995, there was one ophthalmic operating theatre in the Department of Ophthalmology at Waterford Regional Hospital, and a second ophthalmic operating theatre was opened in 1995.
All patients undergoing glaucoma filtration surgery during the 20-year study period were identified. During this time, the decision to convert from medical to surgical therapy was made when medical treatment failed (ie IOP not controlled to the clinician's satisfaction, in the presence of progressive loss of visual field and/or optic nerve damage), where anti-glaucoma therapy could not be tolerated or in those cases where non-compliance with prescribed therapy was suspected or confirmed.
Recently introduced imaging modalities, such as confocal scanning laser ophthalmoscopy, optical coherence tomography, or scanning laser polarimetry, are increasingly used in the decision-making process with respect to the need for glaucoma filtration surgery. However, these technologies were unavailable in Waterford Regional Hospital at any time during the study period, and therefore their introduction did not contribute to the clinical decision to convert from medical to surgical management of glaucoma in this study.
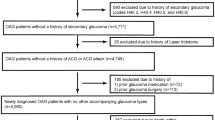
Of note, patients aged 20 years and less were excluded from the study. We felt that most cases of glaucoma in patients aged ⩽20 years are either congenital or developmental in origin, and where surgical intervention is invariably indicated (and, therefore, where the availability of anti-glaucoma medication is unlikely to influence the surgical decision-making process).
The following data were recorded for each patient: age; sex; type of filtration procedure (trabeculectomy, deep sclerectomy, viscocanalostomy) and whether cataract extraction was performed concomitantly. Only two consultant ophthalmic surgeons were present in Waterford Regional Hospital throughout the entire study period, and data collected was restricted to procedures carried out by these surgeons. Due to the nature of the data collection method, and the extended study time period, information regarding the type of glaucoma, for which surgery was performed, was not available.
Glaucoma medications were categorized according to their generic class, determined by mode of action. Details germane to the date of availability of these drugs in the RoI are given in Table 1. Of note, the date of launch of an anti-glaucoma medication in the Republic of Ireland often does not coincide with its authorization by the local drug regulatory body (Irish Medicines Board; www.imb.ie).
We divided the 20 years of the study into four periods, as follows: 1986–1995, 1996, 1997, and 1998–2005. These periods were determined by the year of availability of each new glaucoma medication (Table 1); in each case, allowing for a 1-year time lag between availability and a clinically apparent effect of any new medication and for a change in prescribing habits. Thus, carbonic anhydrase inhibitors were available from 1995 (period 2 therefore commences in 1996), α-agonists were available from 1996 (period 3 commences in 1997), and prostaglandin analogues from 1997 (period 4 commences 1998).
The annual numbers of glaucoma filtration surgeries performed were analysed using a general linear model with the following three factors: period (4 levels, as above); surgeon (2 levels); gender (2 levels). We did a similar three-factor analysis with patient age as the dependent variable.
Results
A total of 778 glaucoma filtration surgeries were performed by either of the two consultant ophthalmic surgeons over the 20-year study period. After exclusion of patients aged 20 years or less, 760 remained.
The mean age (±SD) was 71.4 (±10.0) years, and the men to women ratio was 480:280 (63:37%). Of note, the observed higher proportion of men undergoing glaucoma filtration surgery was statistically significant (P=0.001).
Table 2 illustrates the impact of period and gender on the mean number of glaucoma filtration surgeries performed. For both of these factors, the differences are highly statistically significant, with P=0.001 and P<0.001 for gender and period, respectively, in the general linear model with factors period, gender, and surgeon. However, the gender–period interaction was not statistically significant (P=0.661). The results in Table 2 were obtained by collapsing over the third factor (surgeon). The surgeon factor was not statistically significant, either as a main effect (P=0.158) or interacting with other effects (P>0.05 in all cases).
Hence, there is strong sample evidence that the mean annual per-surgeon number of glaucoma filtration operations differed for different time periods, and for men and women, but there is no evidence to suggest that the gender effect is significantly different for the different time periods. In other words, there is no evidence that drug availability in different periods affected frequency of surgeries in men more than women, or vice versa.
Post hoc analysis (Tukey's HSD test) revealed a highly significant (P<0.001) difference in mean annual per-surgeon number of operations between periods 1 and 4 (ie between 1986–1995 and 1998–2005), the 95% confidence interval for the mean difference being 5.4–16.7. Mean differences for other subperiods were not statistically significant using the Tukey test. It appears, therefore, that the main contributor to the overall statistically significant result is the marked drop in mean annual per-surgeon number of operations in 1998–2005 compared with 1986–1995 (Figure 1).
We also conducted an analysis with patient age as the dependent variable, using the same three factors (period, gender, and surgeon), as before. In this case, the only significant effect (main or interaction) was surgeon: average patient age for surgeon 1 was 70.6 years, and 74.1 years for surgeon 2 (P=0.01). Of note, there was no evidence of a systematic increase in patient age per subperiod, for either men or women (Table 3).
Discussion
In this study, we report the trends in glaucoma filtration surgery in the Department of Ophthalmology at Waterford Regional Hospital over a 20-year period between 1986 and 2006. We investigated the volume of surgeries being performed, the age profile of patients undergoing these surgeries, and the association, if any, between these variables and the introduction of new anti-glaucoma medications controlling for surgeon and gender.
The principal finding of this study is that, for both men and women, there was a statistically significant decline (95% confidence interval between 5.4 and 16.7 per year) in mean annual number of per-surgeon operations in 1997–2005 compared with 1986–1995. These findings are broadly comparable to the results of other studies, which have examined trends in glaucoma surgery across various time periods between 1992 and 2004. Fraser and Wormald,5 for example, recently reported a reduction in the number of trabeculectomies, laser trabeculoplasties, and laser peripheral iridotectomies by 51, 60, and 30%, respectively, in the National Health Service of England between 1994 and 2004. In a large Canadian study, Rachmiel et al6 observed a 37.7% increase in volume of glaucoma filtration surgery between 1992 and 1996, followed by a 17% decrease in volume between 1996 and 2004. This decrease in the volume of trabeculectomies correlated well with the introduction of prostaglandin analogues in December 1996. Bateman et al7 report that volumes of glaucoma filtration surgery in Scotland peaked in 1993, and subsequently fell by 45.9% between 1994 and 1999, a period when there was an increase of 24.9% in the number of topical anti-glaucoma medications prescribed. Other studies in Australia, France, and The Netherlands have provided similar findings.8, 9, 10, 11
However, the possibility that factors other than the introduction of new classes of anti-glaucoma medication contributed to the observed decline in the volume of glaucoma filtration procedures performed during the study period warrant discussion. Indeed, other variables that could influence the volume of glaucoma filtration procedures performed may be classed as socio demographic, economic, and clinical.
Socio-demographic factors that could influence the number of patients requiring glaucoma filtration surgery include changes in the population of subjects at risk for this condition. Of note, the Department of Ophthalmology in Waterford Regional Hospital is the regional ophthalmic centre for the southeast of Ireland. Available Republic of Ireland census of population data for the 65 year and over age group during the 20-year study period are as follows: 1986, 384 355; 1996, 413 882; 2002, 436 001; 2006, 467 926, representing an increase of approximately 20% in the size of this age group over the 20-year period.12 The corresponding figures for the 45–64 year age group were: 1986, 591 444; 1996, 703 800; 2002, 831 993; 2006, 928 868, representing a 57% increase in the size of this age group over the same 20-year study period. In other words, the significant decrease in the volume of glaucoma filtration surgery that we observed over the 20-year study period occurred in an era when the catchment population at risk of developing this condition increased substantially. Economic factors that could influence the volume of glaucoma filtration surgery include those that relate to the healthcare provider and those that relate to the method of surgeon remuneration. Access to ophthalmic surgical services in the regional ophthalmic unit increased in 1995, when a second ophthalmic operating theatre was opened. Indeed, the reduction in glaucoma filtration surgery was observed in conjunction with a simultaneous and dramatic rise in cataract surgery by the same two consultant ophthalmic surgeons, suggesting that the observed decrease in the number of trabeculectomies was not attributable to a reduction in access to ophthalmic surgical services.13 However, it is possible that, in a patient developing chronic angle-closure glaucoma, cataract extraction may result in reduced IOP and thus obviate the need for glaucoma filtration surgery.5
It is possible that the threshold for surgical intervention could be influenced by financial incentivization, such as the method of remuneration to the operating surgeon. In this study, both fee paying and non-fee paying patients undergoing glaucoma filtration surgery by either of the two consultant ophthalmic surgeons were included, and no change in method of remuneration occurred during the study period, thus negating the potential for bias in this respect.
Finally, the possibility that factors, which influence a surgeon's decision to perform glaucoma filtration surgery, might change with the passage of time warrants discussion. For example, changing perceptions regarding the management of glaucoma with respect to the relative merits of primary vs secondary surgical intervention were evaluated in the late 1980s and early 1990s.14, 15 Indeed, many authoritative authors recommended early trabeculectomy over conventional management of glaucoma during this period, possibly contributing to the variability in the volume of glaucoma filtration procedures observed in this study between 1986 and 1995. The variability in surgical volume between 1986 and 1995 might also be explained, at least in part, by the rapid evolution of automated perimetry threshold testing algorithms, and statistical modelling, during this time. However, we feel that, as all glaucoma filtration surgeries performed in this study were under the care of one of the two consultant ophthalmic surgeons over the entire 20-year study period, the potential for bias introduced by varying thresholds for glaucoma filtration surgery that may exist between ophthalmic surgeons was negated, to some extent at least. Furthermore, as Waterford Regional Hospital is the regional ophthalmic centre for the southeast of Ireland, we are very confident that few, if any, cases of chronic glaucoma in adult patients were referred outside of the region for surgical management of glaucoma, and we therefore feel that the observed reduction in the volume of glaucoma filtration surgery over the 20-year period cannot be attributed to referral outside the region.
We also wished to investigate whether available anti-glaucoma medication represented a true decrease in the need for glaucoma filtration surgery, or simply a deferral of such a need. This study does not provide any evidence that the age profile of patients undergoing glaucoma filtration surgery increased over the 20-year study period. The lack of an observed increase in the age profile in our study could be attributable, at least in part, to the fact that population growth in the Republic of Ireland was much greater (57%) for the 45–64 years age group during the study period when compared with the 65 years and over age group (approximately 20%), especially because the only epidemiological data from the Republic of Ireland reports a peak prevalence of primary open angle glaucoma and normal tension glaucoma in the 70–79 years age group.16 However, it is also possible that the 20-year period of this study, although longer than previous studies, is of insufficient duration to detect an increase in the age profile of patients undergoing glaucoma filtration because of slow progression of this disease.
In conclusion, the volume of patients undergoing glaucoma filtration surgery under the care of two consultant ophthalmic surgeons decreased between 1986 and 2006, in an era when the catchment population at risk of developing glaucoma increased substantially. This decrease appears to coincide with the introduction of three new classes of anti-glaucoma medications (prostaglandin analogues, carbonic anhydrase inhibitors, and α-agonists). Further study will be required to determine whether these medications will prevent, or just delay, the ultimate need for glaucoma filtration surgery. Nevertheless, our results do suggest that the introduction of novel anti-glaucoma medications has, at the very least, deferred the need for glaucoma surgery in many patients until a point in time that is beyond the demise of those patients. Whether this observed and encouraging reduction in the demand for surgical intervention in glaucoma patients can be maintained in an era of ever-increasing life expectancy is a question that will remain unanswered for some time.
References
Drance SM . Bowman Lecture. Glaucoma—changing concepts. Eye 1992; 6 (Pt 4): 337–345.
Kelliher C, Kenny D, O’Brien C . Trends in blind registration in the adult population of the Republic of Ireland 1996–2003. Br J Ophthalmol 2006; 90: 367–371.
Gross RL . Current medical management of glaucoma. In: Yanoff M, Duker JS (eds). Ophthalmology, 2nd ed. Mosby: Boston, 2004. pp 1543–1553.
Migdal C . What therapy to use in glaucoma?. In: Yanoff M, Duker JS (eds). Ophthalmology, 2nd ed. Mosby: Boston, 2004. pp 1539–1543.
Fraser SG, Wormald RP . Hospital Episode Statistics and changing trends in glaucoma surgery. Eye 2008; 22: 3–7.
Rachmiel R, Trope GE, Chipman ML, Gouws P, Buys YM . Effect of medical therapy on glaucoma filtration surgery rates in Ontario. Arch Ophthalmol 2006; 124: 1472–1477.
Bateman DN, Clark R, Azuara-Blanco A, Bain M, Forrest J . The effects of new topical treatments on management of glaucoma in Scotland: an examination of ophthalmological health care. Br J Ophthalmol 2002; 86: 551–554.
Baudouin C, Rouland JF, Le Pen C . Changes in medical and surgical treatments of glaucoma between 1997 and 2000 in France. Eur J Ophthalmol 2003; 13 (Suppl 4): S53–S60.
van der Valk R, Schouten JS, Webers CA, Beckers HJ, van Amelsvoort LG, Schouten HJ et al. The impact of a nationwide introduction of new drugs and a treatment protocol for glaucoma on the number of glaucoma surgeries. J Glaucoma 2005; 14: 239–242.
Kenigsberg PA . Changes in medical and surgical treatments of glaucoma between 1997 and 2003 in France. Eur J Ophthalmol 2007; 17: 521–527.
Walland MJ . Glaucoma treatment in Australia: changing patterns of therapy 1994–2003. Clin Experiment Ophthalmol 2004; 32: 590–596.
Central Statistics Office. Census 1986, 1996, 2002, 2006. Cork: Ireland.
O’Reilly P, Mahmoud U, Hayes P, Tormey P, Beatty S . Age and sex profile of patients having cataract surgery between 1986 and 2003. J Cataract Refract Surg 2005; 31: 2162–2166.
Jay JL, Murray SB . Early trabeculectomy versus conventional management in primary open angle glaucoma. Br J Ophthalmol 1988; 72: 881–889.
Migdal C, Gregory W, Hitchings R . Long-term functional outcome after early surgery compared with laser and medicine in open-angle glaucoma. Ophthalmology 1994; 101: 1651–1656; discussion 7.
Coffey M, Reidy A, Wormald R, Xian WX, Wright L, Courtney P . Prevalence of glaucoma in the west of Ireland. Br J Ophthalmol 1993; 77: 17–21.
Author information
Authors and Affiliations
Corresponding author
Additional information
None of the authors has any proprietary interests or research funding relating to the subject matter of this article.
Rights and permissions
About this article
Cite this article
Keane, P., Khan, M., Saeed, A. et al. The impact of available anti-glaucoma therapy on the volume and age profile of patients undergoing glaucoma filtration surgery. Eye 23, 1675–1680 (2009). https://doi.org/10.1038/eye.2008.335
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2008.335