Abstract
Purpose
The arteriole-to-venule ratio (AVR) is widely used for investigating subclinical cerebral microangiopathy. The possible occurrence of retinal vascular caliber changes was investigated in a population of hyperhomocysteinaemic (plasma total homocysteine (tHcy) >13 μmol/l) adult epileptic patients.
Methods
Retinal photographs of cases and controls were evaluated for generalized narrowing of the retinal arterioles, measured as AVR, by graders masked to case–control status using standardized protocols. Plasma total homocysteine (tHcy) levels were assayed by HPLC.
Results
Sixty-seven patients (36M/31F, 36.4±7.5 years of age; mean level of tHcy 22.8±11.4 μmol/l), and 75 control subjects (42M/33F, 35.4±8.5 years of age; mean level of tHcy 7.8±2.3 μmol/l) were enroled. No retinal caliber changes were detected in any patient and healthy subject. The analysis of retinal photographs failed to identify any difference in the venular diameters, arteriolar diameters, and AVR measurements between the two groups (P=0.98).
Conclusions
we showed that adult hyperhomocysteinaemic epileptic patients do not show any changes in retinal vascular caliber assessed by the measurement of AVR.
Similar content being viewed by others
Introduction
Retinal vessels share anatomic and functional properties with small cerebral arteries and their assessment provides a unique method for investigating subclinical cerebral microangiopathy.1 In particular, a generalized narrowing of the retinal arterioles, measured as retinal arteriole-to-venule ratio (AVR), has been associated with cerebrovascular diseases.1
A condition of mild hyper-total-homocysteinemia (hyper-tHcy levels <100 μmol/l) is considered an independent risk factor for cardiovascular2 and cerebrovascular diseases,3 and it is observed in 10–40% of epileptic patients.4
To clarify the effect of hyper-tHcy on retinal vessel diameters, we investigated whether hyper-tHcy is associated with retinal vascular caliber changes in an epileptic population exhibiting hyper-tHcy. As literature data support the view that patients with epilepsy exhibit an increased risk for stroke,5 early knowledge of the retinal vascular caliber might allow a prompt initiation of therapy to prevent stroke.
Patients and methods
Patients were consecutively recruited according to the following inclusion criteria: (a) firm diagnosis of epilepsy (at least 1 year), (b) stable therapy with antiepileptic drugs (i.e., no change of drug and drug dose for at least 6 months); (c) 18–50 years of age; (d) full compliance with the therapy; and (e) no use of vitamins or drugs other than antiepileptic drugs.
Retina findings observed in epileptic patients were compared with those of a group of healthy volunteers, matched for age and sex, exhibiting normal values of tHcy. Informed consent was obtained from all the participants. Plasma tHcy was assessed as described.4 According to our reference intervals, hyper-tHcy was defined when tHcy levels were higher than 13 μmol/l.
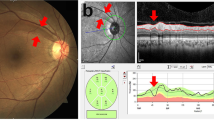
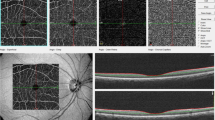
Retina investigation protocol
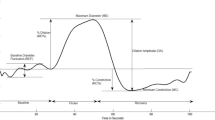
We performed a semiautomated system to evaluate retinal vessel diameters in accordance with the international guidelines.6 In particular, retinal photographs were converted to digital images by a high-resolution scanner centred in a zone surrounding the optic disc (measured directly by the computer's software—Heidelberg HRA angiograph) using standard settings for all photographs.6 On one eye of each subject, a sum value was calculated for the arteriolar blood column diameter and one for the venular (in μm), the AVR being the ratio of these.6 Focal arteriolar narrowing was graded as present or absent. The image was analysed by two trained graders, masked to the end points.
The intra- and interobserver agreements were evaluated through determination of Pearson's correlation coefficients.
Levene and Kolmogorov–Smirnov tests were used to assure the homogeneity and normality, respectively, of the distribution of the outcome variables when parametric tests were used. Most of the statistics were well powered referring to a type I error of P=0.05. Our ability to reject the null hypothesis was ⩾0.8. Continuous variables were evaluated by a Student t-test and analysis of variance (one-way ANOVA) followed by Tukey's test. Categorical variables were analysed by a χ2-test. Statistics were computed using STATISTICA version 6 (USA). A P-value <0.05 was considered to be statistically significant.
Results
Sixty-seven patients (mean epilepsy duration: 8.2±3.6 years) and 75 control subjects fulfilled the listed inclusion criteria (Table 1). There was no statistically significant difference in the characteristics of subjects and patients belonging to the two groups, with the exclusion of tHcy levels (P=0.0092). The mean AVR was 0.84±0.07 in the patient group and 0.88±0.06 in the healthy subjects. The analysis of retinal photographs failed to identify any difference in the venular diameters, arteriolar diameters, and AVR measurements between the two groups (P=0.98; Table 1). Moreover, no arteriovenous crossing signs (i.e., arterio–venous nicking) or focal narrowing were found.
Pearson's correlation coefficients ranged from 0.67 to 0.91 for inter- and intragrader reliability (P<0.05).
Discussion
Our study failed to show that elevated levels of tHcy are associated with generalized arteriolar narrowing in a series of epileptic patients in chronic treatment with anticonvulsants. To the best of our knowledge, the effects of increased tHcy levels on the structural changes in the retinal vascular caliber have not been previously explored. Compared with other retinal signs like haemorrhages, focal arteriolar narrowing or arterio–venous nicking, the AVR was the more reliable and commonly used parameter of vascular damage.6
This study was designed to eliminate any possible confounder factors, and in particular, we included subjects aged under 50 years to minimize the effect of age on both tHcy levels and the retinal vasculature structure.3, 7
Over the last years, the medical literature has been flooded with data indicating that hyper-tHcy is a risk factor for retinal vascular occlusion.8, 9, 10 However, because of the conflicting results from other studies, firm conclusions cannot be achieved yet.11, 12 Thus, it remains still to be assessed whether hyper-tHcy is merely a biochemical marker of atherogenesis or rather a causative factor.11 The possibility that advanced age plays a role in facilitating the detrimental effects of hyper-tHcy on retinal vascular occlusion should be also be considered.11
Further, studies should definitely assess the role of retinal microvascular changes in predicting the risk of cerebrovascular disease in patients with mild hyper-tHcy.
References
Wong TY . Is retinal photography useful in the measurement of stroke risk? Lancet Neurol 2004; 3: 179–183.
Nygard T, Vollset SE, Refsum H . Total homocysteine and cardiovascular disease. J Intern Med 1999; 246: 425–454.
Welch GN, Loscalzo J . Homocysteine and atherothrombosis. N Engl J Med 1998; 338: 1042–1050.
Belcastro V, Gorgone G, Italiano D, Oteri G, Caccamo D, Pisani LR et al. Antiepileptic drugs and MTHFR polymorphisms influence hyperhomocysteinemia recurrence in epileptic patients. Epilepsia 2007; 48: 1990–1994.
Cleary P, Shorvon S, Tallis R . Late-onset seizures as a predictor of subsequent stroke. Lancet 2004; 10: 1184–1186.
Hubbard LD, Brothers RJ, King WN, Clegg LX, Klein R, Cooper LS et al. Methods for evaluation of retinal microvascular abnormalities associated with hypertension/sclerosis in the Atherosclerosis Risk in Communities Study. Ophthalmology 1999; 106: 2269–2280.
Kotliar KE, Mücke B, Vilser W, Schilling R, Lanzl IM . Effect of aging on retinal artery blood column diameter measured along the vessel axis. Invest Ophthalmol Vis Sci 2008; 49: 2094–2102.
Cahill MT, Stinnett SS, Fekrat S . Meta-analysis of plasma homocysteine, serum folate, serum vitamin B12, and thermolabile MTHFR genotype as risk factors for retinal vascular occlusive disease. Am J Ophthalmol 2003; 136: 1136–1150.
Chua B, Kifley A, Wong TY, Mitchell P . Homocysteine and retinal vein occlusion: a population-based study. Am J Ophthalmol 2005; 139: 181–182.
Narayanasamy A, Subramaniam B, Karunakaran C, Ranganathan P, Sivaramakrishnan R, Sharma T et al. Hyperhomocysteinemia and low methionine stress are risk factors for central retinal venous occlusion in an Indian population. Invest Ophthalmol Vis Sci 2007; 48: 1441–1446.
Di Crecchio L, Parodi MB, Sanguinetti G, Iacono P, Ravalico G . Hyperhomocysteinemia and the methylenetetrahydrofolate reductase 677C-T mutation in patients under 50 years of age affected by central retinal vein occlusion. Ophthalmology 2004; 111: 940–945.
Pinna A, Carru C, Zinellu A, Dore S, Deiana L, Carta F . Plasma homocysteine and cysteine levels in retinal vein occlusion. Invest Ophthalmol Vis Sci 2006; 47: 4067–4071.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Belcastro, V., Striano, P., Ciampa, C. et al. Is retinal assessment useful in epileptic patients with hyperhomocysteinemia?. Eye 23, 1532–1534 (2009). https://doi.org/10.1038/eye.2008.326
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2008.326