Abstract
Preimplantation genetic diagnosis (PGD) is an alternative to prenatal diagnosis for patients at risk of transmitting an inherited disease such as myotonic dystrophy type 1(DM1) to their offspring. In this paper, the clinical application of preimplantation diagnosis for DM1 upon request to children born is described in a large cohort of risk couples. PGD could be offered to all 78 couples opting for PGD regardless of the triplet repeat size. The incidence of major complications was minimalised following a careful assessment in affected DM1 females anticipating possible cardiological, obstetrical and anaesthetical problems. A live-birth delivery rate per cycle with oocyte retrieval of 20% was the outcome. Forty-eight of the 49 children born are in good health and have normal psychomotor development.
Similar content being viewed by others
Introduction
Myotonic dystrophy type 1 (DM1) is the most common form of inherited muscular dystrophy in adults (OMIM 160900). DM1 is an autosomal dominant disorder with an incidence of 1/8000.1 It is a multisystemic disorder affecting several tissues, such as distal limb (rather than proximal) and facial muscles, smooth muscles (gastrointestinal, uterus), the heart (primarily the conduction system), the eye (cataract) and the endocrine system (eg insulin resistance, hypotestosteronism). Phenotypic expression and age of onset are highly variable, ranging from an asymptomatic adult to a congenital form in which the neonate presents with severe hypotonia, respiratory distress and feeding difficulties often leading to death.1, 2 DM1 can be divided into four main categories presenting specific clinical features: the neonatal congenital form, the juvenile form, the classic adult form and the minimally affected late-onset form.2, 3
The molecular genetic defect involves the expansion of an unstable CTG repeat in the 3′ untranslated region of the DMPK gene on the long arm of chromosome 19 (19q13.2–q13.3). The trinucleotide repeat size is highly polymorphic and relatively stable in the general population, ranging from 5 to 37 CTG repeats in normal individuals. Alleles greater than 55 repeats are associated with disease, highly unstable in the germ line and can expand to several hundreds or even thousands of CTG trinucleotide repeats.4, 5 There is a broad correlation between the CTG expansion size and the severity of the disease, but there is considerable variability within the different categories and even within a family.3 Anticipation, defined as the worsening of disease severity in successive generations, is usually observed in association with an increase in the number of repeats.6
For couples at risk wanting to prevent transmission of the disease to their offspring, prenatal diagnosis (PND) followed by a termination of pregnancy (TOP), in the case of an affected child, used to be the only option apart from gamete donation, adoption or remaining childless.7 Since 1995, preimplantation genetic diagnosis (PGD) became an alternative.8 PGD avoids the need for termination of an affected pregnancy. The embryos are obtained after in vitro fertilisation (IVF) by intracytoplasmatic sperm injection (ICSI) and once cultured up to the eight-cell stage, blastomeres can be removed and used for diagnosis, followed by the transfer of embryos diagnosed as healthy with regard to the disease under consideration.
This report presents the outcome in a large cohort of consecutive DM1 patients undergoing PGD for DM1 from request to child. Data on PGD requests, treatment cycles (number of oocytes, fertilisation rate, embryo biopsy and transfers), pregnancies, confirmation of PGD during pregnancy by PND, deliveries, disease-specific complications, children born and follow-up of the children (medical outcome and psychomotor development) are discussed.
Materials and methods
Patients and counselling
From January 1992 to December 2005, 118 couples inquired about the possibility of undergoing PGD for DM1. Ninety-eight couples were seen at the outpatient clinic by a clinical geneticist, a gynaecologist and a nurse co-ordinator who informed them about the procedure in detail. This included the need for IVF by ICSI with ovarian hyperstimulation, embryo biopsy and a single-cell diagnostic procedure on a biopsied blastomere. Furthermore, the possibilities of a control PND and the need for pregnancy and children follow-up were discussed.9 An informed consent explaining the above was signed by both partners before treatment. Data on country of residence, age of the female at the moment of the first cycle, gender of the affected partner, CTG repeat sizes of the patients and reason for opting for PGD were recorded. Seventy-eight couples enrolled in the PGD program. Female patients were asked to undergo a cardiological assessment including an electrocardiogram and an echocardiography to detect asymptomatic conduction disturbances before their treatment because of the cardiac disease involvement in DM1 patients.10, 11
Preliminary genetic testing
CTG repeat numbers of normal and affected alleles in both partners were analysed before PGD. The first single cell polymerase chain reaction (PCR) assay developed for PGD-DM1 allowed selection of unaffected embryos based on the presence of the ‘normal repeat’ of the affected and one of the repeats of the unaffected partner in the biopsied cell.8, 12 As the expanded repeat of the affected parent cannot be amplified by conventional PCR at the single cell level, only fully informative couples, with the normal allele of the affected partner clearly different from the alleles of the unaffected partner, were eligible for PGD. From 1997 onwards, with the development of the triplet-primed PCR (TP-PCR) based test, half-informative couples with both partners sharing one allele size and non-informative couples with three identical normal alleles, could also be offered treatment.13, 14
Ovarian stimulation and oocyte retrieval
Controlled ovarian hyperstimulation (COH) was carried out in a GnRH agonist or antagonist protocol.15 Oocyte retrieval was carried out under premedication with a paracervical block and exceptionally, under general anaesthesia.15
ICSI and embryo biopsy procedure
To obtain embryos, IVF with ICSI with ejaculated sperm and exceptionally with testicular sperm as described before was the method of choice rather than classical IVF. This method was applied to prevent contamination of the biopsied blastomeres with DNA from residual sperm stuck to the zona pellucida (ZP).9, 16, 17 Fertilisation and embryo development were assessed daily before embryo biopsy. From the six-cell stage onwards, blastomere biopsy was performed. Till 1998, only one cell was removed from six-cell embryos and two cells were removed from embryos containing seven or more blastomeres. After 1998, following a misdiagnosis, two cells were biopsied from all embryos and the transfer policy was thoroughly revised. Only embryos with concordant results in both blastomeres were transferred.18 To perform the biopsy, the embryo was immobilized with a holding pipette; the ZP was then breached using acidic Tyrode's solution or a diode laser.19 A biopsy pipette was introduced through the hole and one or two blastomeres were carefully aspirated. Each blastomere was washed and transferred to a PCR tube containing lysis buffer.8
Single-cell genetic diagnosis
For informative couples, both DNA fragments containing the DM1-related CTG repeat were amplified at the single cell level. At first, a nested PCR approach was taken, but this was later replaced by fluorescent PCR techniques.8, 12 For half-informative or non-informative couples, a TP-PCR procedure was performed.13, 14
Embryo transfer, cryopreservation, pregnancy and delivery
If available, one or two and, exceptionally, three or four unaffected embryos of good quality were transferred into the uterus on day 3, 4 or 5 post insemination.20 Supernumerary unaffected embryos were, if possible, cryopreserved for later transfer.9 Implantation was confirmed with two consecutively rising β-HCG concentrations at 10 and 13 days after embryo transfer. When an intrauterine gestational sac was seen at ultrasound at least 5 weeks after embryo transfer, a clinical pregnancy was recorded. An ongoing pregnancy was registered when a foetal heartbeat at ≥12 weeks was recorded. A miscarriage was defined as a loss of a foetus of a gestational age less than 20 weeks. Expulsions after 20 complete weeks of gestation were defined as stillborn. Perinatal deaths are intrauterine or intrapartum and neonatal deaths ≤7 days after birth at a gestational age of ≥20 weeks.21 As of the risk of misdiagnosis, the possibility of a PND for confirmation of the PGD-DM1 diagnosis was offered to all pregnant couples. The following data about the course of the pregnancy and the delivery were recorded through questionnaires given to the parents and the obstetrician at the moment of treatment and in the third trimester of gestation: ultrasound data, pregnancy complications such as antepartum haemorrhage, defined as bleeding after 22 weeks,22 preterm labour (defined as the onset of labour after 20–28 weeks of gestation and before 37 weeks of pregnancy23), hypertensive disorder, the result of the PND if performed, the mode of delivery, complications during delivery, gestational age at birth.21
Children follow-up
Data on the children born were collected through questionnaires addressed to the parents and their paediatricians. Children were examined at the age of 2 months, 1 year and 2 years, by clinical geneticists, when compliant. Major malformations were defined as malformations causing general functional impairment or requiring surgical correction; all other malformations were considered minor malformations.21, 24
Results
Patients and preliminary genetic testing
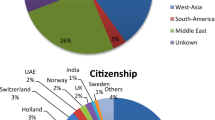
The country of residence of the 118 couples requesting PGD for DM1 and the 78 couples undergoing PGD is summarised in Table 1 and shows that 62 couples (52.5.%) and 36 (46.2%), respectively, resided outside Belgium. The reasons for considering PGD in the 118 and the 78 couples, respectively, are summarised in Table 2. In 80 couples (67.8%) the female partner was affected by DM1, whereas in 38 couples (33.2%) the male partner was affected. Of the total of 118 couples requesting PGD, 20 did not present at the outpatient clinic and they refrained from further treatment after receiving information by mail.
Ninety-eight couples were seen before PGD and had pre-PGD informativity testing. Of these, 64 couples were informative (65.3%), 33 were half-informative (33.7%) and one couple was non-informative (1%). Twenty couples out of 98 eventually did not proceed to PGD for the following reasons: one couple was psychologically not ready for PGD, one couple had financial problems, one couple had reservations about the safety of the treatment, two couples had relationship problems and two couples opted for spontaneous pregnancy and PND by chorionic villous sampling. Five couples postponed their PGD cycle to a later period. For the eight remaining couples who did not proceed to treatment, the reason was not traceable.
Of the 78 couples with PGD, the female partner was affected in 54 (69.2%) couples. The mean age of the women was 31.2 years (20–41years). On the basis of clinical information, the majority of the patients could be classified in the category of the adult classical form of DM1. The mean CTG-triplet repeat size of the affected allele was 430 (50–1330) in the women and 350 (65–370) in the men.15 Cardiac evaluation was documented in 45 of the 54 affected women (83%), seven (13%) of which showed mild conduction and rhythm disturbances, six (11%) showed valvular disease (five with a mitral valve prolaps, one with an aorta insufficiency).Two (4%) had myocardial disease (left ventricle wall dysfunction and relative large heart at the ultrasound). For nine of the 54 affected women there was a lack of written information. Fifty-one (64.5%) of the couples were informative; 26 (33.3%) were half-informative and one (1.3%) non- informative.
Oocyte retrieval, ICSI and embryo biopsy embryo transfer and cryopreservation
In total, seventy-eight patients underwent 205 cycles with oocyte retrieval (Figure 1). Thirteen oocyte retrievals in five patients were performed under general anaesthesia; the others were carried out under premedication and paracervical anaesthesia. The reasons for opting of general anaesthesia were earlier history of tonic convulsions as the result of use of xylocaine in one patient, unbearable pain at an earlier oocyte retrieval in three patients and in one patient it was performed at the patient's explicit request.
Of a mean of 11.0 (7.0 SD) cumulus–oocyte complexes (COC) collected per cycle, a mean of 9.5 (6.4 SD) metaphase II oocytes were microinjected with one single sperm. Of these, a mean of 7.4 (5.0 SD) were fertilised and a mean of 4.9 (5 SD) embryos were biopsied. Of these 419 (41.5%) were unaffected, 453 (44.9%) affected and in 138 (13.7%) embryos there was no diagnosis. Forty embryos or a mean of 0.2 (0.8 SD) embryos could be cryopreserved.
Of the 205 cycles started, 151 (73.7%) had an embryo-transfer procedure (Figure 1).
Pregnancy outcome
In 51 of the 151 cycles with embryo transfer, two consecutive positive serum β-hCG measurements were observed resulting in 48 clinical pregnancies and 43 ongoing pregnancies with 53 foetal heartbeats (34 singleton, 8 twin, 1 triplet pregnancies), leading eventually to 41 deliveries with the birth of 49 children. No perinatal deaths were recorded. Twenty–one pregnancies were obtained (48.8%) after one PGD cycle and 12 (27.9%) after two cycles. Four (9.3%) pregnancies were obtained after three and another four (9.3%) after five cycles, and one (2.3%) after six and another one (2.3%) after seven cycles. One singleton pregnancy resulted in a spontaneous miscarriage at 10 weeks and one singleton pregnancy was terminated because of a misdiagnosis seen after chorionic villous sampling and CTG repeat analysis. One triplet was reduced to a twin pregnancy, and one twin was reduced to a singleton pregnancy. Twenty-six of the 41 deliveries occurred in DM1-affected women.
Expressed per cycle with oocyte retrieval, 23.7% of the cases resulted in a clinical pregnancy and 20.0% in a live birth. Expressed per transfer, 31.7% of the cases resulted in a clinical pregnancy and 27.1% in a live birth. Thirty-six couples had at least one child after a mean of 2.1 cycles.
The PGD-DM1-not-affected diagnosis was confirmed by PND in 26 foetuses (16 chorionic villous samples, 10 amniocenteses). In all foetuses the karyotype was normal. One misdiagnosis was reported after chorionic villous sampling and CTG-trinucleotide repeat analysis of the DMPK gene. In one case, a postnatal molecular confirmation of a normal preimplantation diagnosis was reported. Clinical examination up to 2 years of age did not show any suspicion of DM1 in another 10 children.
Of the 41 deliveries, 19 deliveries were by caesarean section (C/S). Nine C/S were primary: one repeat C/S, three for foetal breech presentation (one twin pregnancy), one for fetopelvine disproportion, two for twin pregnancies (one with gestational diabetes) and two at maternal request. Ten C/S were secondary: one for preterm vaginal bleeding and suspected partial placental abruption at a gestational age of 36 weeks and two for failure to progress in labour after induction of labour, four because of preeclampsia, one for preterm premature rupture of membranes (PPROMs) and two for suspected foetal distress in labour. In 10 of the C/S the woman was affected. Six of the 19 C/S were performed in twin pregnancies. One vacuum extraction and two forceps deliveries were recorded, all in DM1-affected women. There were 19 normal vaginal deliveries (NVDs), 11 of which were in affected women.
One major obstetrical complication occurred in a female DM1 patient pregnant with twins after a reduction of triplets. She presented with acute respiratory distress, pulmonary oedema, associated HELLP syndrome (hypertension, elevated liver enzymes, low platelets) and renal insufficiency after induction of labour at 38 weeks of gestation, followed by an emergency C/S under general anaesthesia, performed at another hospital, for suspected foetal distress during labour. After delivery, the patient needed to be intubated for supportive ventilation. Weaning off the ventilator was difficult and tracheotomy was necessary. Other obstetrical complications in 26 pregnancies of affected women included antepartum bleeding in two, preterm labour in four and hypertensive disorder in another four: preeclampsia in two and HELPP syndrome in two.
Children follow-up
Forty-nine were children born (33 singletons and 16 twins) after PGD. The mean gestational age at delivery for singletons and twins was 38.7 and 36.5 weeks, respectively, and the mean birth weight for singletons and twins was 3294 g and 2484 g, respectively. The Apgar score at 5 min ranged from 7 to 10. Eight children were admitted to the neonatal unit: five for a short observation period only and three (one born after 35 weeks of pregnancy and a twin born at 31.6 weeks) because of assisted feeding requirements. At birth, no major malformations were listed. Minor malformations included two transient cardiac anomalies in two children and a capillary haemangioma in both twin members, aplasia cutis at both legs of one newborn and a unilateral metatarsus adductus in one child. Karyotypes were checked in 30 of the 49 children either pre- or postnatally and were normal. Follow-up information was available for 46 (93.9%) of the 49 children at 2 months of age and for 36 (73.5%) when they had reached the age of 2 years. At 2 months of age, several minor anomalies not mentioned at birth were registered. These were: preauricular tag, supernumerary nipple, umbilical hernia, sacral dimple, congenital nevus, Mongolian spot, simian crease, nasolacrimal stenosis and café au lait spot. In one child, galactosemia was already diagnosed before 2 months of age. No developmental delay was recorded except in the child with galactosemia, who presented a global developmental delay of 6 months at 2 years of age. Two children presented with a mild transient language delay.
Discussion
This study describes the clinical application of PGD from request to delivery and children born in a large cohort of couples at risk of transmitting DM1. Specific attention was paid to the feasibility of PGD, disease-specific complications of treatment and pregnancy in DM1-affected women, the success rate in terms of live born delivery rate and the health of the children. The main findings of this paper were as follows: (i) after careful pre-treatment assessment with regard to disease-specific complications, it was safe to perform PGD in DM1-affected women; (ii) the live born delivery rate per treatment cycle was 20%, with at least one baby after two PGD cycles in almost half of the couples; (iii) the children born were generally in good health up to 2 years of age and comparable to children born after ICSI for infertility and after PGD for other genetic conditions.
Residence of patients
Of the 118 couples requesting PGD, less then half resided in Belgium. The remaining couples were referred from a variety of other countries, either because PGD was not allowed in their home country or because PGD for DM1 was not available at that time in their country.
Reasons for opting for PGD
The data regarding reasons for opting for PGD are in line with the literature.25, 26, 27 We did not observe a higher percentage of couples who chose PGD because of the existing fertility problems in DM1.28, 29 These figures may be biased because in the total group there were more affected female patients than affected males and whether females with DM1 are less fertile is still controversial.15 The higher proportion of affected females in our group can be partly explained by the referral policy of one PGD centre in The Netherlands, where PGD for DM1 is offered to male patients but not to female patients. It is interesting to note the uptake for PGD (88%) in the couples requesting PGD because they objected to TOP. Conversely, and surprisingly, a lower uptake (69%) for PGD was observed in the infertile couples, although they needed IVF to conceive, and also a lower uptake (54%) in the fertile couples who had experienced TOP in the past, possibly because after receiving full information they decided that PND remained the less burdensome option for them.
Preliminary genetic testing
From the genetic point of view, PGD could be offered to all couples regardless of the informativity of the trinucleotide repeat sizes in affected and unaffected partners. In the early years, PGD could be offered only to informative couples.8 From 1997 onwards, all couples could be accepted for PGD because of the development of a single-cell test TP-PCR test.13, 14 Currently, which means since 2008, the use of multiplex PCR with linked markers combined, with the detection of the repeat fragments has increased the accuracy of the diagnosis through the detection of contamination of the sample and allele drop out and allowed us also to change our biopsy policy from an obligate two-cell to one-cell analysis.30, 31, 32
Disease-associated complications
Women affected by DM1 should only be accepted in a PGD programme after careful assessment and counselling regarding potential cardiological, anaesthetical and obstetrical problems.11, 33, 34, 35 The cardiac anomalies found in the affected females of this study corresponded to the typical anomalies usually observed in DM1 patients, that is, conduction anomalies and valve disease.11 However, these anomalies were not severe enough to be a contra-indication for ovarian stimulation or pregnancy for any of the females involved. As of the progression and the unpredictable course of cardiac disease in individuals, female patients should be re-evaluated before every further PGD treatment. Specific expertise and preoperative assessment before invasive interventions (oocyte retrieval, operative deliveries) is needed in DM1 patients because of the known sensitivity to anaesthetic drugs. General anaesthesia should be avoided because of the risk of respiratory insufficiency and the need for aspiration because of incompetence of the lower oesophageal sphincter.34, 35 After a careful cardiac work up leading to the use of adjusted anaesthetic drugs no complications occurred in the five patients who underwent oocyte retrieval under general anaesthesia. An emergency C/S procedure under general anaesthesia in a woman affected by DM1 lead to one major complication.
The possible obstetric complications during spontaneous pregnancies in DM1 patients were recently reviewed by Rudnik-Schöneborn and Zerres33 and are mostly owing to uterine dysfunction and abnormal placentation. In our study, the miscarriage rate in affected females was not increased compared with a normal reference population.33 Our findings of antepartum bleeding (7.7%) and preeclampsia (7.7%) were consistent with the literature although preeclampsia has not been very well studied.33 Preterm labour was observed in 15.4% of the affected pregnant females without major effect on the mean gestational age probably because none of our affected and pregnant females suffered from a severe clinical form of DM1. An instrumental delivery was needed in 50% of the pregnant affected women, probably to be explained by the prolonged labour in DM1 patients because of the uterine dysfunction in the first stage of labour.33 Four of the five twin pregnancies in affected women were delivered by C/S. Recognising the limitations of our results in terms of sample size and the intrinsically lower perinatal risk as a result of the selection of healthy embryos, the higher risk of obstetrical complications in a DM1 patient, as well as in a multiple pregnancy justifies a transfer policy that restricts the number of embryos. The Belgian law on the financial means of hospitals of 2003,36 which regulates selective single-embryo transfer in patients aged <36 years in first or second IVF trial, has already resulted in a decrease of twin birth rates in our small group from 27.3% (6 twins/22 pregnancies) before 2003 to 6.9% (2 twins/29 pregnancies) after 2003. This decrease was also recorded in the general ICSI pregnancies.37
Pregnancy and delivery rates
As reported earlier, our reported clinical pregnancy rate per cycle with oocyte retrieval of 23.4% is in line with the EHSRE PGD consortium data for DM1 and pregnancy rates reported for other dominant diseases.38
A live born delivery rate of 20% per cycle with oocyte retrieval was observed. Almost half (48.8%) the pregnancies and an equal percentage (48.7%) of the deliveries of live born occurred after one cycle and 76.7% were obtained after one or two cycles. Five couples had more than one pregnancy. This means that 46.1% of the couples had at least one baby after a mean of 2.1 cycles. This is useful information to be discussed when counselling couples who are considering PGD.
Prenatal diagnosis
In 53% of the foetuses reaching at least 10 weeks of pregnancy, PGD results were checked through CVS or amniocentesis. In only 19% of the couples opting for PND, the woman was over 35 years old, suggesting that advanced maternal age was not the reason for PND in the majority of the patients. This observation was also seen in pregnancies obtained after ICSI in the early days.39 The reason of not opting for PND could not fully be explained by the objection to TOP because only 62.5% of the couples not opting for PND were against TOP and the remaining had fertility problems. Surprisingly, 70% of the couples in whom PND was performed were against TOP, although those couples would never contemplate a TOP in case of misdiagnosis, but probably wanted to be reassured. As was described earlier one misdiagnosis was recorded in 1998.18 This is our only recorded misdiagnosis in 170 foetuses tested pre- or postnatal for monogenic diseases until 2005. As the residual risk of misdiagnosis, we continue to offer the possibility of PND to confirm the PGD-DM1 analysis despite the risk of miscarriage because of the PND procedure.9 Postnatal DNA analysis is not systematically proposed, because of ethical implications associated with pre-symptomatic testing of minors and what has so far been a lack of specific guidelines for DM1 testing.40, 41 Although recognising that most of them are still young, no signs of the disease have as yet been observed at the follow-up of the children born after PGD-DM1.
Children follow-up
So far, 49 children were born after PGD for DM1 and information at birth was available for all of them. Birth parameters were comparable to the birth parameters of IVF, ICSI and PGD children.21, 38, 42 At birth, no major malformations were recorded and the incidence of 12.2% minor malformations was comparable to ICSI children or other PGD children in general.21, 38
Considering galactosemia as a major malformation recorded at 2 months of age, the overall incidence was 2%, which is within the normal range. Follow-up at 2 months of age showed a higher percentage (22.4%) of minor anomalies compared with the number recorded at birth. This could be explained by the fact that, at birth, the minor malformations were reported by the parents and paediatricians, whereas at 2 months of age they were observed by a dedicated team of clinical geneticists at our Centre and according to a standardised checklist.21, 24 At the age of 2 years, data on 73.5% of the children born after PGD-DM1 were available. The majority of the children lost for follow-up by the age of two lived in another country. This is probably the explanation for their lower compliance. In general, the children born and seen for follow-up were in good health.
In conclusion, until 1995, couples at 50% risk of transmitting DM1 had three possible alternatives to prevent the transmission of the condition, that is, PND and TOP in case of an affected fetus, the use of donor gametes or remaining childless. The data in this report illustrate that PGD for DM1 is now a well-established procedure resulting in the birth of unaffected and mostly healthy children. Therefore, PGD for DM1 should be discussed as a valuable alternative to PND in a setting of careful counselling and clinical management regarding the IVF procedure and DM1-related problems, especially in couples with concomitant infertility and couples reluctant to undergo TOP.
References
Meola G : Clinical and genetic heterogeneity in myotonic dystrophies. Muscle Nerve 2000; 23: 1789–1799.
Machuca Tzili L, Brook D, Hilton Jones D : Clinical and molecular aspects of the myotonic dystrophies: a review. Muscle Nerve 2005; 31: 1–18.
Salehi L, Bonifazi E, Di Stasio E et al: Risk prediction for clinical phenotypes in myotonic dystrophy type 1: data from 2650 patients. Gene Test 2007; 11: 84–90.
Brook J, Mc Currah M, Harley H, Buckler A, Church D, Aburatani H : Molecular basis of myotonic dystrophy: expansion of trinucleotide (CTG) repeats at 3′ end of transcript encoding a protein kinase family member. Cell 1997; 68: 799–808.
Mahadevan M, Tsilfidis C, Sabourin L et al: Myotonic dystrophy mutation: an unstable CTG repeat in the 3′ untranslated region of the gene. Science 1992; 255: 1253–1255.
Harper PS, Harley HG, Reardon W, Shaw DJ : Anticipation in myotonic dystrophy: new light on an old problem. Am J Hum Genet 1992; 51: 10–16.
Martorell L, Cobo AM, Baiget M, Naudó M, Poza JJ, Parra J : Prenatal diagnosis in myotonic dystrophy type 1. Thirteen years of experience: implications for reproductive counselling in DM1 families. Prenat Diagn 2007; 27: 68–72.
Sermon K, Lissens W, Joris H et al: Clinical application of preimplantation diagnosis for myotonic dystrophy. Prenat Diagn 1997; 17: 925–932.
Sermon K, Van Steirteghem A, Liebaers I : Preimplantation diagnosis. Lancet 2004; 363: 1633–1634.
Pelargonio G, Dello Russo A, Sanna T, De Martino G, Bellocci F : Myotonic dystrophy and the heart. Heart 2002; 88: 665–670.
Sovari AA, Bodine CK, Farokhi F : Cardiovascular manifestations of myotonic dystrophy-1. Cardiol Rev 2007; 15: 191–194.
Sermon K, De Vos A, Van de Velde H et al: Fluorescent PCR and automated fragment analysis for the clinical application of preimplantation genetic diagnosis (Steinert's disease). Mol Hum Reprod 1998; 4: 791–796.
Warner JP, Barron LH, Goudie D et al: A general method for the detection of large CAG repeat expansions by fluorescent PCR. J Med Genet 1996; 33: 1022–1026.
Sermon K, Seneca S, De Rycke M et al: PGD in the lab for triplet repeat diseases-myotonic dystrophy, Huntington's disease and fragile-X syndrome. Mol Cell Endocrinol 2001; 183: S77–S85.
Verpoest W, De Rademaeker M, Sermon K et al: Real and expected delivery rates of patients with myotonic dystrophy undergoing intracytoplasmatic sperm injection and preimplantation genetic diagnosis. Hum Reprod 2008; 23: 1654–1660.
Van Steirteghem A, Joris H, Liu J et al: Protocol for intracytoplasmatic sperm injection. Hum Reprod Update 1995; 1: 3, CD ROM.
Liebaers I, Sermon K, Staessen C, Joris H, Lissens W, Van Assche E : Clinical experience with preimplantation genetic diagnosis and intracytoplasmatic sperm injection. Hum Reprod 1998; 13: 186–195.
Sermon K, Goossens V, Seneca S et al: Preimplantation diagnosis for Huntington's disease: clinical application and analysis of the HD expansion in affected embryos. Prenat Diagn 1998b; 18: 1427–1436.
De Vos A, Van Steirteghem A : Aspects of biopsy procedures prior to preimplantation genetic diagnosis. Prenat Diagn 2001; 21: 767–780.
Van Landuyt L, De Vos A, Joris H, Verheyen G, Devroey P, Van Steirteghem A : Blastocyst formation in in vitro fertilisation versus intracytoplasmic sperm injection cycles: influence of the fertilisation procedure. Fertil Steril 2005; 83: 1397–1403.
Bonduelle M, Liebaers I, De Ketelaere V, Derde M-D, Camus M, Devroey P, Van Steirteghem A : Neonatal data on a cohort of 2889 infants born after ICSI (1991–1999) and of 2995 infants born after IVF (1983–1999). Hum Reprod 2002; 17: 671–694.
Konje CJ, Walley RJ : Bleeding in late pregnancy; in James DK, Steer PJ, Weiner CP, Gonik B (eds): From High risk pregnancy management options. WB Saunders Company Ltd, Philadelphia, 1996.
Svigos JM, Robinson JS, Vigneswaran R : Threatened and actual preterm labor including mode of delivery; in James DK, Steer PJ, Weiner CP, Gonik B (eds): From High Risk Pregnancy Management Options. WB Saunders Co Ltd, Philadelphia, 1996, pp 151–152.
Bonduelle M, Ponjaert I, Van Steirteghem A, Derde M-P, Devroey P, Liebaers I : Developmental outcome at 2 years of age for children born after ICSI compared with children born after IVF. Hum Reprod 2006; 18: 342–350.
Harper JC, Boelaert K, Geraerdts J et al: ESHRE PGD Consortium data collection V cycles from January to December 2002 with pregnancy follow-up to October 2003. Hum Reprod 2006; 21: 3–21.
Vandervorst M, Staessen C, Sermon K et al: The Brussels' experience of more than 5 years of clinical preimplantation genetic diagnosis. Hum Reprod Update 2000; 6: 364–373.
Kakourou G, Dhanjal S, Mamas T et al: Preimplantation genetic diagnosis for myotonic dystrophy type 1 in the UK. Neuromuscul Disord 2008; 18: 131–136.
Sagel J, Distiller L, Morley J, Isaacs H, Kay G, van der Walt A : Myotonoca dystrophica studies on gonadal function using luteinising-releasing-hormone (LRH). J Endocr Metab 1975; 40: 1110–1113.
Sarkare PS, Paul S, Han J, Reddy S : Six 5 gene is required for spermatogenic cell survival spermiogenesis. Hum Mol Genet 2004; 13: 1421–1431.
Sermon K : Current concepts in preimplantation genetic diagnosis (PGD): a molecular biologist's view. Hum Reprod Update 2002; 8: 11–20.
Goossens V, DeRycke M, DeVos A et al: Diagnostic efficiency, embryonic development and clinical outcome after the biopsy of one or two blastomeres for preimplantation genetic diagnosis. Hum Reprod 2008; 223: 481–492.
Spits C, De Rycke M, Verpoest W et al: Preimplantation genetic diagnosis for Marfan syndrome. Fertil Steril 2006; 86: 310–320.
Rudnik-Schöneborn S, Zerres K : Outcome in pregnancies complicated by myotonic dystrophy: a study of 31 patients and review of the literature. Eur J of Obstet Gynecol Reprod Biol 2004; 114: 44–53.
White RJ : Case report. Anaesthetic management of a patient with myotonic dystrophy. Paed Anaesth 2001; 11: 494–497.
White RJ, Bass SP : Myotonic dystrophy paediatric anaesthesia. Paed Anaesth 2003; 13: 94–102.
Gerris JM : Single embryo transfer and IVF/ICSI outcome: a balanced appraisal. Hum Reprod Update 2005; 11: 105–121.
Van Landuyt L, Verheyen G, Tournaye H, Camus M, Devroey P, Van Steirteghem A : New Belgian embryo transfer policy leads to sharp decrease in multiple pregnancy rate. Reprod Biomed Online 2006; 13: 765–771.
Goossens V, Harton G, Moutou C et al: ESHRE PGD consortium data collection VIII: cycles from December 2005 with pregnancy follow-up to October 2006. Hum Reprod 2008; 23: 2629–2645.
Bonduelle M, Van Assche E, Joris H et al: Prenatal testing in ICSI pregnancies: incidence of chromosomal anomalies in 1586 karyotypes and relation to sperm parameters. Hum Reprod 2002; 17: 2600–2614.
Fokstuen S, Myring J, Evans C, Harper PS, Fokstuen S : Presymptomatic testing in myotonic dystrophy: genetic counselling approaches. J Med Genet 2001; 38: 846–850.
Borry, Goffin T, Nys H, Dierickx K : Attitudes regarding predictive genetic testing in minors a survey of European P clinical geneticists. Am J Med Genet C Semin Med Genet 2008; 15: 148C:78–148C:83.
Van Steirteghem A, Bonduelle M, Devroey P, Liebaers I : Follow-up of children born after ICSI. Hum Reprod Update 2002; 8: 111–116.
Acknowledgements
We thank Michael Whitburn of the language centre of the Vrije Universiteit Brussel for proofreading the paper. We also thank the secretarial staff and colleagues at the Centre of Medical Genetics and the colleagues at the Centre of Reproductive Medicine, the ‘Wetenschappelijke Fonds Willy Gepts (WFWG)’ for supporting our PGD research, and Schering-Plough (Organon International) for an unconditional educational grant allowing the follow-up of the pregnancies and children born after PGD.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
De Rademaeker, M., Verpoest, W., De Rycke, M. et al. Preimplantation genetic diagnosis for myotonic dystrophy type 1: upon request to child. Eur J Hum Genet 17, 1403–1410 (2009). https://doi.org/10.1038/ejhg.2009.56
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejhg.2009.56
Keywords
This article is cited by
-
Preimplantation genetic diagnosis in female and male carriers of reciprocal translocations: clinical outcome until delivery of 312 cycles
European Journal of Human Genetics (2012)