Abstract
Background/Objectives:
The objectives of this study were to investigate the relationship between inflammatory parameters (CRP, c-reactive protein; AGP, α1-acid glycoprotein), iron status indicators (SF, serum ferritin; sTfR, soluble transferrin receptor) and body mass index (BMI) z-score, fat-free mass (FFM) and fat mass (FM) in European adolescents. Differences in intake for some nutrients (total iron, haem and non-haem iron, vitamin C, calcium, proteins) were assessed according to BMI categories, and the association of nutrient intakes with BMI z-score, FM and FFM was evaluated.
Methods:
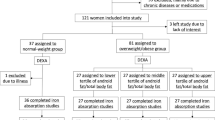
A total of 876 adolescents participating in the Healthy Lifestyle in Europe by Nutrition in Adolescence-Cross Sectional Study were included in the study sample.
Results:
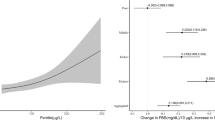
Mean CRP values (standard error; s.e.) were significantly higher in overweight/obese adolescents (1.7±0.3 and 1.4±0.3 mg/l in boys and girls, respectively) than in thin/normal-weight adolescents (1.1±0.2 and 1.0±0.1 mg/l in boys and girls, respectively) (P<0.05). For boys, mean SF values (s.e.) were significantly higher in overweight/obese adolescents (46.9±2.7 μg/l) than in thin/normal-weight adolescents (35.7±1.7 μg/l) (P<0.001), whereas median sTfR values did not differ among BMI categories for both boys and girls. Multilevel regression analyses showed that BMI z-score and FM were significantly related to CRP and AGP (P<0.05). Dietary variables did not differ significantly among BMI categories, except for the intake of vegetable proteins, which, for boys, was higher in thin/normal-weight adolescents than in overweight/obese adolescents (P<0.05).
Conclusions:
The adiposity of the European adolescents was sufficient to cause chronic inflammation but not sufficient to impair iron status and cause iron deficiency.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Day CP . From fat to inflammation. Gastroeneterology 2006; 130: 207–210.
Trayhurn P, Wood IS . Signalling role of adipose tissue: adipokines and inflammation in obesity. Biochem Soc Trans 2005; 33: 1078–1808.
Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW Jr . Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest 2003; 112: 1796–1808.
Xu H, Barnes GT, Yang Q, Tan G, Yang D, Chou CJ et al. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest 2003; 112: 1821–1830.
van Dielen FMH, van’t Veer C, Schols AM, Soeters PB, Buurman WA, Greve JWM . Increased leptin concentrations correlate with increased concentrations of inflammatory markers in morbidly obese individuals. In J Obes 2001; 25: 1759–1766.
Visser M, Bouter LM, McQuillan GM, Wener MH, Harris TB . Elevated C-reactive protein levels in overweight and obese adults. JAMA 1999; 282: 2131–2135.
Visser M, Bouter LM, McQuillan GM, Wener MH, Harris TB . Low grade systemic inflammation in overweight children. Pediatrics 2001; 107: 1–6.
Maachi M, Piéroni L, Bruckert E, Jardel C, Fellahi S, Hainque B, Capeau J, Bastard J-P . Systemic low-grade inflammation is related to both circulating and adipose tissue TNFa, leptin and IL-6 levels in obese women. In J Obes 2004; 28: 993–997.
Benedek IH, Blouin RA, McNamara PJ . Serum protein binding and the role of increased alpha 1-acid glycoprotein in moderately obese male subjects. Br J Clin Pharmacol 1984; 18: 941–946.
Nead KG, Halterman JS, Kaczorowski JM, Auinger P, Weitzman M . Overweight children and adolescents: A risk group for iron deficiency. Pediatrics 2004; 114: 104.
Zimmermann MB, Zeder C, Muthayya S, Winichagoon P, Chaouki N, Aeberli I et al. Adiposity in women and children from transition countries predicts decreased iron absorption, iron deficiency and a reduced response to iron fortification. Int J Obes 2008; 32: 1098–1104.
Moschonis G, Chrousos GP, Lionis C, Mougios V, Manios Y . Healthy Growth Study group. Association of total body and visceral fat mass with iron deficiency in preadolescents: the Healthy Growth Study. Br J Nutr 2012; 108: 710–719.
Lecube A, Carrera A, Losada E, Hernández C, Simó R, Mesa J . Iron deficiency in obese postmenopausal women. Obesity 2006; 14: 1724–1730.
Gillum RF . Association of serum ferritin and indices of body fat distribution and obesity in Mexican American men: the Third National Health and Nutrition Examination Survey. Int J Obes 2001; 25: 639–645.
Kant AK . Reported consumption of low nutrient density foods by American children and adolescents, nutritional health correlates, NHANES III, 1988 to 1994. Arch Pediatr Adolesc Med 2003; 157: 789–796.
Failla ML, Kennedy ML, Chen ML . Iron metabolism in genetically obese (ob/ob) mice. J Nutr 1988; 118: 46–51.
Anonymous. Dietary reference intake for vitamin A, vitamin K, arsenic, borium, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium and zinc. National Academy Press: Washington, D.C., 2001, pp 290–393.
Aeberli I, Hurrel RF, Zimmermann MB . Overweight children have higher circulating hepcidin concentrations and lower iron status but have dietary iron intakes and bioavailability comparable with normal weight children. In t J Obes 2009; 33: 1111–1117.
Manios Y, Moschonis G, Chrousos GP, Lionis C, Mougios V, Kantilafti M et al. The double burden of obesity and iron deficiency on children and adolescents in Greece: the Healthy Growth Study. J Hum Nutr Diet 2013; 26: 470–478.
Cheng HL, Bryant C, Cook R, O’Connor H, Rooney K et al. The relationship between obesity and hypoferraemia in adults: a systematic review. Obes Rev 2012; 13: 150–161.
Beguin Y . Soluble transferring receptor for the evaluation of erythropoiesis and iron status. Clin Chim Acta 2004; 329: 9–22.
Moreno LA, De Henauw S, González-Gross M, Kersting M, Molnár D, Gottrand F et al. Design and implementation of the healthy lifestyle in Europe by nutrition in adolescence Cross-Sectional Study. Int J Obes 2008; 32: S4–S11.
Béghin L, Castera M, Manios Y, Gilbert CC, Kersting M, De Henauw S et al. Quality assurance of ethical issues and regulatory aspects relating to good practices in the HELENA Cross-Sectional Study. Int J Obes 2008; 32S: S12–S18.
Béghin L, Huybrechts I, Vicente-Rodríguez G, De Henauw S, Gottrand F, Gonzales-Gross M et al. Main characteristics and participation rate of European adolescents included in the HELENA study. Arch Public Health 2012; 70: 14.
Nagy E, Vicente-Rodriguez G, Manios Y, Béghin L, Iliescu C, Censi L, Dietrich S, Ortega FB et al. Harmonization process and reliability assessment of anthropometric measurements in a multicenter study in adolescents. Int J Obes 2008; 32S: S58–S65.
Moreno LA, Rodríguez G, Guillén J, Rabanaque MJ, León JF, Ariño A . Anthropometric measurements in both sides of the body in the assessment of nutritional status in prepubertal children. Eur J Clin Nutr 2002; 56: 1208–1215.
Slaughter MH, Lohman TG, Boileau RA, Horswill CA, Stillman RJ, van Loan MD et al. Skinfold equation for estimation of body fatness in children and youths. Hum Biol 1988; 60: 709–723.
Cole TJ, Freeman JV, Preece MA . Body Mass Index References curves for the UK, 1990. Arch Dis Child 1995; 73: 25–29.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH . Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000; 320: 1240–1243.
Tanner JM, Whitehouse RH . Clinical longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch Dis Child 1976; 51: 170–179.
Erhardt JG, Estes JE, Pfeiffer CM, Biesalski HK, Craft NE . Combined measurement of ferritin, soluble transferrin receptor, retinol binding protein, and C-reactive protein by an inexpensive, sensitive, and simple sandwich enzyme-linked immunosorbent assay technique. J Nutr 2004; 134: 3127–3132.
Vereecken CA, Covents M, Matthys C et al. Young adolescent’s nutrition assessment on computer (YANA-C). Eur J Clin Nutr 2005; 59: 658–667.
Vereecken CA, Covents M, Sichert-Hellert W, Alvira JM, Le Donne C, De Henauw S et al. Development and evaluation of a self-administered computerized 24-h dietary recall method for adolescents in Europe. Int J Obes 2008; 32S: S26–S34.
Haubrock J, Hartting U, Souverein O, Boeing H . An improved statistical tool for estimating usual intake distributions: the Multiple Source Method (MSM). Arch Public Health 2010; 68: 14–15.
Hallberg L . Bioavailable nutrient density: a new concept applied in the interpretation of food iron absorption data. Am J Clin Nutr 1981; 34: 2242–2247.
Thurnham D, McCabe LD, Haldar S, Wieringa FT, Northrop-Clewes CA, McCabe GP . Adjusting plasma ferritin concentrations to remove the effects of subclinical inflammation in the assessment of iron deficiency: a meta analysis. Am J Clin Nutr 2010; 92: 546–555.
Pardo A, Ruiz MA, San Martin R . How to fit and interpret multilevel models using SPSS. Psicothema 2007; 19: 308–321.
Ford ES, Galuska DA, Gillespie C, Will JC, Giles WH, Dietz WH . C-reactive protein and body mass index in children: findings from the third National Health and Nutrition Examination Survey, 1988–1994. J Pediatr 2001; 138: 486–492.
Benedek IH, Blovin RA, Mc Namara PJ . Serum protein binding and the role of increate alpha 1-acid glycoprotein in moderately obese male subjects. Br J Clin Pharmacol 1984; 18: 941–946.
Bogdański P, Chyrek R, Pupek-Musialik D, Jabłecka A . Evaluation of selected acute phase proteins in patients with metabolic syndrome. Pol Merkur Lekarski 2006; 21: 12–14.
Northrop-Clewes CA . Interpreting indicators of iron status during an acute phase response – lessons from malaria and HIV. Ann Clin Biochem 2008; 45: 18–32.
Zimmermann MB, Hurrell RF . Nutritional iron deficiency. Lancet 2007; 370: 511–520.
Wärnberg J, Nova E, Moreno LA, Romeo J, Mesana MI, Ruiz JR et al. Inflammatory proteins are related to total and abdominal adiposity in a healthy adolescent population: the AVENA Study. Am J Clin Nutr 2006; 84: 505–512.
Mena NP, Esparza A, Tapia V, Valdés P, Núñez MT . Hepcidin inhibits apical iron uptake in intestinal cells. Am J Physiol Gastrointest Liver Physiol 2008; 294: 192–198.
Pinhas-Hamiel O, Newfield RS, Koren I, Agmon A, Lilos P, Philip M . Greater prevalence of iron deficiency in overweight and obese children and adolescents. Int J Obes 2003; 27: 416–418.
Cepeda-López AC, Aeberli I, Zimmermann MB . Does obesity increase risk for iron deficiency? A review of the literature and the potential mechanism. Int J Vitam Nutr Res 2010; 80: 263–270.
Amato A, Santoro N, Calabrò P, Grandone A, Swinkels DW, Perrone L, del Giudice EM . Effect of body mass index reduction on serum hepcidin levels and iron status in obese children. Int J Obes 2010; 34: 1772–1774.
del Giudice EM, Santoro N, Amato A, Brienza C, Calabrò P, Wiegerinck ET et al. Hepcidin in obese children as a potential mediator of the association between obesity and iron deficiency. J Clin Endocrinol Metab 2009; 94: 5102–5107.
Knowles JM, Thurnham DI, Phengdy B et al. Impact of inflammation on biomarkers of iron status in a cross-sectional survey of Lao women and children. Brit J Nutr 2013; 110: 2285–2297.
Aeberli I, Kaspar M, Zimmermann MB . Dietary intake and physical activity of normal weight and overweight 6- to 14-year-old Swiss Children. Swiss Med Wkly 2007; 137: 424–430.
Cepeda-López AC, Osendarp SJ, Melse-Boonstra a, Aeberli I, Gonzalez-Salazar F, Feskens E et al. Sharply higher rates of iron deficiency in obese Mexican women and children are predicted by obesity-related inflammation rather than by differences in dietary iron intake. Am J Clin Nutr 2011; 93: 975–983.
Stang J, Story MT, Harnack L, Neumark-Sztainer D . Relationships between vitamin and mineral supplement use, dietary intake, and dietary adequacy among adolescents. J Am Diet Assoc 2000; 100: 905–910.
Acknowledgements
The HELENA Study has taken place with the financial support of the European Community Sixth RTD Framework Programme (Contract FOOD-CT-2005–007034). Additional support was obtained from the Spanish Ministry of Education (AGL2007-29784-E/ALI; AP-2005-3827; AP-2008-03806). Jara Valtueña was financially supported by the Universidad Politécnica de Madrid. Augusto César F. de Moraes was given scholarship from São Paulo Research Foundation – FAPESP (proc. 2011/11137-1 and 2011/20662-2). Luis A. Moreno was given scholarship of visiting professor from Brazilian government by Science without Borders Program by CNPq (National Counsel of Technological and Scientific Development) and CAPES (Coordination of Improvement of Higher Education Personnel) (proc. 007/2012). The content of this article reflects only the authors’ views, and the European Community is not liable for any use that may be made of the information contained therein. We thank all adolescents who participated in the study. We also thank Lorenza Mistura for her assistance in the statistical analysis.
Disclosure
The content of this paper reflects only the authors’ view and the rest of HELENA Study members are not responsible for it. The writing group takes sole responsibility for the content of this article.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Appendix
Appendix
**Helena Study Group
Co-ordinator: Luis A. Moreno
Core Group members: Luis A. Moreno, Fréderic Gottrand, Stefaan De Henauw, Marcela González-Gross, Chantal Gilbert.
Steering Committee: Anthony Kafatos (President), Luis A. Moreno, Christian Libersa, Stefaan De Henauw, Jackie Sáchez, Fréderic Gottrand, Mathilde Kesting, Michael Sjostrom, Dénes Molnár, Marcela González-Gross, Jean Dallongeville, Chantal Gilbert, Gunnar Hall, Lea Maes, Luca Scalfi.
Project Manager: Pilar Meléndez
1. Universidad de Zaragoza (Spain): Luis A. Moreno, Jesús Fleta, José A. Casajús, Gerardo Rodríguez, Concepción Tomás, María I. Mesana, Germán Vicente-Rodríguez, Adoración Villarroya, Carlos M. Gil, Ignacio Ara, Juan Revenga, Carmen Lachen, Juan Fernández Alvira, Gloria Bueno, Aurora Lázaro, Olga Bueno, Juan F. León, Jesús Mª Garagorri, Manuel Bueno, Juan Pablo Rey López, Iris Iglesia, Paula Velasco, Silvia Bel.
2. Consejo Superior de Investigaciones Científicas (Spain): Ascensión Marcos, Julia Wärnberg, Esther Nova, Sonia Gómez, Esperanza Ligia Díaz, Javier Romeo, Ana Veses, Mari Angeles Puertollano, Belén Zapatera, Tamara Pozo.
3. Université de Lille 2 (France): Laurent Beghin, Christian Libersa, Frédéric Gottrand, Catalina Iliescu, Juliana Von Berlepsch.
4. Research Institute of Child Nutrition Dortmund, Rheinische Friedrich-Wilhelms-Universität Bonn (Germany): Mathilde Kersting, Wolfgang Sichert-Hellert, Ellen Koeppen.
5. Pécsi Tudományegyetem (University of Pécs) (Hungary): Dénes Molnar, Eva Erhardt, Katalin Csernus, Katalin Török, Szilvia Bokor, Mrs. Angster, Enikö Nagy, Orsolya Kovács, Judit Repásy.
6. University of Crete School of Medicine (Greece): Anthony Kafatos, Caroline Codrington, María Plada, Angeliki Papadaki, Katerina Sarri, Anna Viskadourou, Christos Hatzis, Michael Kiriakakis, George Tsibinos, Constantine Vardavas Manolis Sbokos, Eva Protoyeraki, Maria Fasoulaki.
7. Institut für Ernährungs- und Lebensmittelwissenschaften –Ernährungphysiologie. Rheinische Friedrich Wilhelms Universität (Germany): Peter Stehle, Klaus Pietrzik, Marcela González-Gross, Christina Breidenassel, Andre Spinneker, Jasmin Al-Tahan, Miriam Segoviano, Anke Berchtold, Christine Bierschbach, Erika Blatzheim, Adelheid Schuch, Petra Pickert.
8. University of Granada (Spain): Manuel J. Castillo, Ángel Gutiérrez, Francisco B. Ortega, Jonatan R Ruiz, Enrique G. Artero, Vanesa España-Romero, David Jiménez-Pavón, Palma Chillón, Magdalena Cuenca-Garcia.
9. Istituto Nazionale di Ricerca per gli Alimenti e la Nutrizione (Italy): Davide Arcella, Elena Azzini, Emma Barrison, Noemi Bevilacqua, Pasquale Buonocore, Giovina Catasta, Laura Censi, Donatella Ciarapica, Paola D’Acapito, Marika Ferrari, Myriam Galfo, Cinzia Le Donne, Catherine Leclercq, Giuseppe Maiani, Beatrice Mauro, Lorenza Mistura, Antonella Pasquali, Raffaela Piccinelli, Angela Polito, Raffaella Spada, Stefania Sette, Maria Zaccaria.
10. University of Napoli ‘Federico II’ Dept of Food Science (Italy): Luca Scalfi, Paola Vitaglione, Concetta Montagnese.
11. Ghent University (Belgium): Ilse De Bourdeaudhuij, Stefaan De Henauw, Tineke De Vriendt, Lea Maes, Christophe Matthys, Carine Vereecken, Mieke de Maeyer, Charlene Ottevaere, Inge Huybrechts.
12. Medical University of Vienna (Austria): Kurt Widhalm, Katharina Phillipp, Sabine Dietrich.
13. Harokopio University (Greece): Yannis Manios, Eva Grammatikaki, Zoi Bouloubasi, Tina Louisa Cook, Sofia Eleutheriou, Orsalia Consta, George Moschonis, Ioanna Katsaroli, George Kraniou, Stalo Papoutsou, Despoina Keke, Ioanna Petraki, Elena Bellou, Sofia Tanagra, Kostalenia Kallianoti, Dionysia Argyropoulou, Katerina Kondaki, Stamatoula Tsikrika, Christos Karaiskos.
14. Institut Pasteur de Lille (France): Jean Dallongeville, Aline Meirhaeghe.
15. Karolinska Institutet (Sweden): Michael Sjöstrom, Patrick Bergman, María Hagströmer, Lena Hallström, Mårten Hallberg, Eric Poortvliet, Julia Wärnberg, Nico Rizzo, Linda Beckman, Anita Hurtig Wennlöf, Emma Patterson, Lydia Kwak, Lars Cernerud, Per Tillgren, Stefaan Sörensen.
16. Asociación de Investigación de la Industria Agroalimentaria (Spain): Jackie Sánchez-Molero, Elena Picó, Maite Navarro, Blanca Viadel, José Enrique Carreres, Gema Merino, Rosa Sanjuán, María Lorente, María José Sánchez, Sara Castelló.
17. Campden & Chorleywood Food Research Association (United Kingdom): Chantal Gilbert, Sarah Thomas, Elaine Allchurch, Peter Burgess.
18. SIK—Institutet foer Livsmedel och Bioteknik (Sweden): Gunnar Hall, Annika Astrom, Anna Sverkén, Agneta Broberg.
19. Meurice Recherche & Development asbl (Belgium): Annick Masson, Claire Lehoux, Pascal Brabant, Philippe Pate, Laurence Fontaine.
20. Campden & Chorleywood Food Development Institute (Hungary): Andras Sebok, Tunde Kuti, Adrienn Hegyi.
21. Productos Aditivos SA (Spain): Cristina Maldonado, Ana Llorente.
22. Cárnicas Serrano SL (Spain): Emilio García.
23. Cederroth International AB (Sweden): Holger von Fircks, Marianne Lilja Hallberg, Maria Messerer.
24. Lantmännen Food R&D (Sweden): Mats Larsson, Helena Fredriksson, Viola Adamsson, Ingmar Börjesson.
25. European Food Information Council (Belgium): Laura Fernández, Laura Smillie, Josephine Wills.
26. Universidad Politécnica de Madrid (Spain): Marcela González-Gross, Jara Valtueña, David Jiménez-Pavón, Ulrike Albers, Raquel Pedrero, Agustín Meléndez, Pedro J. Benito, Juan José Gómez Lorente, David Cañada, Alejandro Urzanqui, Juan Carlos Ortiz, Francisco Fuentes, Rosa María Torres, Paloma Navarro.
Rights and permissions
About this article
Cite this article
Ferrari, M., Cuenca-García, M., Valtueña, J. et al. Inflammation profile in overweight/obese adolescents in Europe: an analysis in relation to iron status. Eur J Clin Nutr 69, 247–255 (2015). https://doi.org/10.1038/ejcn.2014.154
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2014.154
This article is cited by
-
Novel insights into the consequences of obesity: a phenotype-wide Mendelian randomization study
European Journal of Human Genetics (2022)
-
Roux-en-Y Gastric Bypass as a Treatment for Hepatic Iron Overload: An Exploratory Study
Obesity Surgery (2022)
-
Prevalence of iron deficiency and related factors in Spanish adolescents
European Journal of Pediatrics (2020)
-
Diet as moderator in the association of adiposity with inflammatory biomarkers among adolescents in the HELENA study
European Journal of Nutrition (2019)
-
Dietary iron intake and availability are related to maternal education level in overweight/obese adolescents
European Journal of Nutrition (2018)