Abstract
In the 1970s, with the advent of biochemical multichannel screening in the United States and other western countries, the clinical presentation of primary hyperparathyroidism (PHPT) changed from a symptomatic to an asymptomatic disorder. However, in Asian countries, like China, PHPT did not show this evolution, but rather continued to be a symptomatic disease with target organ involvement. In this paper, we revisit the clinical features of PHPT in New York and Shanghai, representative United States and Chinese cites, over the past decade. The questions we address are whether the disease evolved in China to a more asymptomatic one and, whether in the United States further changes are evident. The results indicate that while PHPT continues to present primarily as an asymptomatic disease in the United States, a new phenotype characterized by normal serum calcium and high parathyroid hormone levels, normocalcemic PHPT, has emerged. Data from Shanghai demonstrates a trend for PHPT to present more commonly as an asymptomatic disorder in China. However, most patients with PHPT in China still manifest classical symptoms, i.e. nephrolithiasis and fractures. A comparison of the two cohorts shows that Chinese patients with PHPT are younger, with higher serum calcium and PTH levels, and lower 25-hydroxyvitamin D levels than patients in New York. Normocalcemic PHPT has not yet been recognized in Shanghai. In summary, although the phenotypes of PHPT in both cities are evolving towards less evident disease, sharp clinical and biochemical differences are still apparent in PHPT as expressed in China and the United States.
Similar content being viewed by others
Introduction
In countries that began to utilize the multichannel biochemical screening test in the 1970s, the presentation of primary hyperparathyroidism (PHPT) changed from a disease that was classically symptomatic with “stones, bones, moans and groans” to a contemporary asymptomatic disorder (1). While this clinical evolution was apparent in the United States and other Western countries, in Asian countries, such as India and China, PHPT continued to be seen as a symptomatic disorder with severe biochemical and target organ manifestations (2). More than a decade ago, this difference between the clinical presentations of PHPT patients in western and Asian countries was confirmed by a comparison between New York City, USA and Beijing, China (3). In that “Tale of Two Cities”, patients with PHPT in Beijing were shown to have higher serum calcium (12.4±1.1 vs. 10.7±10.7 mg·dL−1), and PTH concentrations (21.4 vs. 1.86 fold above normal) as compared with their American counterparts from 1984–1999. Strikingly, 97% of the Beijing patients suffered from skeletal lesions (osteitis fibrosa cystica, osteoporosis, pathological fractures), kidney stones and other features of PHPT, while less than 20% of New York patients were symptomatically involved (3). The disease pattern in Beijing, China reflected the experience in the United States prior to the advent of the multichannel autoanalyzer.
In this paper, we review the more recent experience in two cities, Shanghai and New York, with the central question: has the clinical expression of PHPT changed in these countries over the past 10 years?
Methods
The cohort from Shanghai has recently been reported (4). These subjects form the basis for the description of the more recent experience in China. In the United States, an ongoing new cohort of subjects since 2010 form the basis of the New York experience, along with a published experience of subjects who present with normocalcemic PHPT (5,6). As opposed to asymptomatic cases, symptomatic PHPT refers to symptoms related with hypercalcemia, such as skeletal and renal diseases, neuromuscular, gastrointestinal, articular, hematologic, cardiovascular and central nervous system manifestations.
Statistical analyses
All statistical analyses were performed using SPSS (version 13.0; SPSS Inc, Chicago, Illinois). The data are expressed as means±SD, except for data that did not have a normal distribution, which are expressed as median (range). Variables were tested for normality using the Kolmogorov-Smirnov Z statistic. Between-group differences were analyzed with an independent samples t test and a 1-way ANOVA.
Results
The New York Experience, 2010–2013
In the United States, asymptomatic PHPT still predominates with over 80% in this category. However, over the past 10 years, another group of individuals with PHPT has surfaced in which the serum total and ionized calcium are normal and the PTH level is elevated (5). They have no evidence for secondary causes of hyperparathyroidism, such as vitamin D deficiency, renal, liver, or gastrointestinal disease. The New York experience was gleaned from a referral population in which subjects were evaluated for low bone density. In the course of that evaluation, the elevated PTH level was discovered, even though the serum calcium was normal. It was hypothesized that these patients represent the earliest manifestations of the disease, a “forme fruste” of PHPT (5), in keeping with the proposal of Parfitt, Kleerekoper and Rao (7). However, about 75% of these individuals with normocalcemic PHPT have low bone mass. Only 10% of subjects in the New York cohort were truly asymptomatic. It was further demonstrated that 40% of these individuals developed more clinical features and complications related with PHPT, such as hypercalcemia, marked hypercalciuria, and greater bone loss, over a median 3-year follow-up (6).
The observation that normocalcemic PHPT is being discovered in the context of a referral population and that these individuals already demonstrate clinical features of the disease raises the possibility that there is another set of individuals with normocalcemic PHPT whose skeletal involvement is much less evident. Screening a large epidemiological database of unselected individuals is likely to reveal yet another cohort of subjects with normocalcemic PHPT. They would be the counterpart of subjects with asymptomatic PHPT with hypercalcemia. This putative cohort would be described as asymptomatic normocalcemic PHPT. The Columbia group has recently shown that such individuals can be identified using data from The Osteoporotic Fractures in Men (MrOS) Study and the Dallas Heart Study (8).
In 2008, normocalcemic PHPT was formally recognized as a specific clinical form of PHPT at the Third International Workshop on the Management of Asymptomatic PHPT (9,10). It was not clear, at that time, whether the guidelines established for the management of the hypercalcemic form of PHPT would apply to the normocalcemic variant. From a diagnostic point of view, these patients are to be distinguished from hypercalcemic individuals whose serum calcium may occasionally be measured within normal limits. In normocalcemic PHPT, the serum calcium during a standard monitoring period is always normal. It is necessary to exclude secondary causes for an elevated PTH. The serum 25-hydroxyvitamin D level should be greater than 30 ng·mL−1 (75 nmmol·L−1) and renal function by estimated glomerular filtration rate should be higher than 60 mL·min−1. Other causes of secondary hyperparathyroidism should be evaluated for and excluded, such as liver disease, malabsorption, hypercalciuria, and use of thiazide diuretics or lithium (11).
Although normocalcemic PHPT represents only a small percentage of subjects (<10%) in the New York cohort, it has become evident not only in the United States, but also in Brazil and European countries (11,12). However, no data are available from China and other Asian countries.
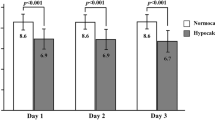
With the exception of the emergence of normocalcemic PHPT in the United States, the clinical phenotype of PHPT has not changed substantially over the past 20 years. The serum calcium and PTH levels are similar to average values 20 years ago. It is noteworthy, however, that mean 25-hydroxyvitamin D levels are much higher than they used to be. The average 25-hydroxyvitamin D level is now 36.7±16 ng·mL−1, as compared to 21±1 ng·mL−1 in the cohort described from 1984–1999. Renal stone disease is seen to the same extent. A comparison of the breakdown of subjects with PHPT in the United States from 1984–1999 to 2010–2013 is shown in Figure 1.
Symptomatic and asymptomatic primary hyperparathyroidism in New York City, from 1984–1993 and 2010–2013. Symptomatic PHPT refers to symptoms related with hypercalcemia, such as skeletal and renal diseases, neuromuscular, gastrointestinal, articular, hematologic, cardiovascular and central nervous system manifestations. With the exception of the emergence of normocalcemic PHPT in the United States, the clinical phenotype of PHPT has not changed substantially over the past 20 years. Since the normocalcemic individuals have only recently been systemically identified, the percentage noted in this figure is likely to be an underestimate of its true prevalence.
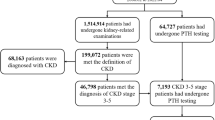
The Chinese Experience, 2000–2010 and Evolution of PHPT in China
In Shanghai, 249 subjects with PHPT representing a majority of provinces (17 of 31) were diagnosed and treated from 2000 to 2010 in a single clinical center. A clear increase in numbers of subjects diagnosed with PHPT became apparent during this period (Figure 2). Their characteristics were recently described (4) and are summarized in Table 1. When PHPT patients are grouped into quartiles based on their serum PTH concentrations, calcium, alkaline phosphatase and creatinine increase with higher PTH levels, while the serum concentrations of albumin and hemoglobin, and bone mineral density at the lumbar spine, femoral neck and total hip decrease with higher PTH levels.
The presentation of PHPT in China appears to have changed markedly over the past 10 years. In Beijing, virtually all subjects were symptomatic. In Shanghai, 10 years later, there are many more patients with asymptomatic disease (Figure 3). In contrast to the earlier experience in China, when virtually the entire population was symptomatic, only 60% of this more recent cohort manifests classical symptoms such as polydipsia, polyuria, urolithiasis, bone pain, and fragility fracture. The average serum calcium has fallen from 12.4±1.1 to 11.72±1.4 mg·dL−1 (nl: 8.4-10.2) and the mean PTH has fallen from 1391 pg·mL−1 to 402 pg·mL−1 (nl: 10–65). Even within the Shanghai experience, the percentage of asymptomatic subjects rose from < 20% in the first half of the decade reviewed to approximately 40% in the latest 4-year period. Moreover, individuals who were symptomatic between 2000–2010 demonstrated a more mild presentation (Figures 2 and 3). The shift in this clinical phenotype can be explained by more routine measurement of serum calcium as well as widespread use of neck ultrasonography during routine examinations.
In the Shanghai cohort of confirmed PHPT, there were no cases of normocalcemic disease. In the only 2 patients with normal calcium levels, their circulating 25-hydroxyvitamin D concentrations were below 30 ng·mL−1, thus not fulfilling the criteria for normocalcemic PHPT.
Comparison of the American and Chinese Subjects with PHPT based upon the recent cohorts
As shown in Table 2, Chinese patients are significantly younger and the population does not show the female predominance noted in the American experience. Moreover, the Chinese subjects with PHPT experienced a shorter disease course and displayed more severe biochemical abnormalities, including significantly higher serum calcium, PTH and alkaline phosphatase concentrations and lower serum albumin and 25-hydroxyvitamin D concentrations.
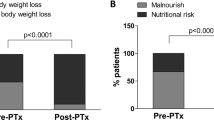
The two main target organs, namely kidney and bone, also display differences between the two cohorts. In Shanghai, there is a much higher prevalence of kidney stones (48 vs. 14%) with a significantly higher serum creatinine level (1.03 vs. 0.79 mg/dL). BMD at the lumbar spine is significantly lower in the Shanghai cohort but there is no significant difference in the hip region. There is no difference in fracture rates. Malignancy was seen in 14/249 (about 6%), which is substantially higher than most published reports. No cases of parathyroid cancer were diagnosed in the American cohort. A comparison of these features between the recent American and Chinese experiences is shown in Figure 4.
Comparison of the differences in current presentation of primary hyperparathyroidism in New York City and Shanghai. Note the continued higher prevalence of symptomatic disease in the Chinese cohort, as well as relatively high occurrence of parathyroid cancer. Normocalcemic primary hyperparathyroidism is noted in the American cohort but not in the Chinese population.
Discussion
The current data from New York and Shanghai demonstrate that PHPT continues to evolve in both the United States and China. A new phenotype of PHPT, normocalcemic PHPT, has emerged (13). Normocalcemic PHPT requires careful definition because many patients with hypercalcemia will show normal calcium values from time to time. This occasional excursion of the serum calcium down into the normal range among those who have hypercalcemia is to be contrasted with normocalcemic PHPT in which the serum calcium is always normal. The surprising observation with the cohorts reported so far is that they tend to have more symptomatic disease than subjects with the common hypercalcemic variant of PHPT. This can be explained by the fact the normocalcemic PHPT is being described in subjects referred because of a possible underlying metabolic bone disease. They would not, therefore, appear to be the forerunner of asymptomatic hypercalcemic PHPT. Asymptomatic normocalcemic subjects are likely to be discovered only through non-selected epidemiological cohorts in which there is no selection bias (8,9). Among those individuals described so far, nevertheless, progression to hypercalcemia has been described (1,5,6). Recently, even a case of parathyroid carcinoma presenting as normocalcemic PHPT was reported (14).
More information is clearly needed with regard to both the symptomatic subjects with normocalcemic PHPT as well as the individuals who are more likely to represent the asymptomatic variant of normocalcemic PHPT. Only then will it be possible to suggest guidelines for the surgical or medical management of this form of PHPT.
In Asian countries, like China, normocalcemic PHPT has not yet been recognized. The reasons for this are several-fold. First, there is a high prevalence of vitamin D deficiency among individuals who present with normal serum calcium and high PTH levels. This form of secondary hyperparathyroidism is thus the most likely explanation for their elevated PTH levels. As these subjects are repleted with vitamin D one of 3 clinical sequellae are possible: the PTH will be become normal; the serum calcium will become elevated, indicating traditional hypercalcemic PHPT; or the diagnosis of normocalcemic PHPT will be made. Further studies are ongoing to determine what percentage of Chinese individuals who present with high PTH and low serum 25(OH)D levels will fall into which category. A second reason why normocalcemic PHPT is not being described in China relates to the limited access to PTH and DXA measurements in the country. Even if a DXA unit is available and the finding of low bone mass is made, practitioners will often treat the individual without a search for an underlying cause for the bone loss syndrome.
The big change in China is the clear evolution of PHPT from a symptomatic to an asymptomatic disease. The pattern appears to be duplicating the experience of the United States and other Western countries 40 years ago when PHPT became recognized commonly as an asymptomatic disease. The increasing use of biochemical screening in China is likely to be one explanation for this change in clinical phenotype. Another explanation resides in the widespread use of ultrasound examination of the neck. This is akin to another kind of screening test. If the current trend continues in China, the asymptomatic form of PHPT may well become the predominant one in the next 10–15 years.
Several other comparative features are noteworthy between the New York and the Shanghai experiences. The length of known disease was much shorter in Chinese subjects than those in the United States. While this might argue that delayed recognition is not a factor, it still could be. In China, it is likely the disease duration is not documented accurately since routine testing is not widely available. In the United States, however, hypercalcemia is more likely to have been documented for a longer period of time. The more severe presentation of disease in China argues for this interpretation. On the other hand, the younger age at diagnosis could argue that the disease is truly more severe in China. The markedly lower serum 25(OH)D levels in the Chinese subjects, in the range where PHPT has been shown to be much more severe (15), argues for this point. Although it is noteworthy that serum 25(OH)D levels are higher now in the Shanghai PHPT population than the cohort described from Beijing (13 vs. 8.8 ng·mL−1), the levels are still very low. The larger parathyroid tumor size in the Chinese subjects is also compatible with their vitamin D deficient state. This finding is similar to other reports describing an inverse association between serum 25(OH)D and parathyroid adenoma weight (16). The larger tumor size in Chinese patients with PHPT also may make the lesion more readily detected by ultrasound. As a consequence, a larger amount of PTH is needed to reach the new set-point (16). These pathophysiological changes may partly explain the higher PTH serum concentrations and larger tumor size observed in Chinese population.
Another interesting comparative note is that the there is not the overwhelming female preponderance in China as compared to the United States and many other western countries. This difference in female predominance was appreciated in the original study (3) and has also been seen in India (2).
It is clear that in both cities, PHPT has changed substantially over the past decade. In China, the evolution from a predominantly symptomatic disorder to one that is increasingly being seen as an asymptomatic one is mirroring the experience in the United States and elsewhere 40 years ago. In the United States, the emergence of a normocalcemic variant is bringing new concepts to how this disease develops clinically as well as the possibility that one can show progressive disease even before hypercalcemia ensues.
References
Silverberg SJ, Walker MD, Bilezikian JP . Asymptomatic primary hyperparathyroidism. J Clin Densitom. 2013;16:14–21.
Pradeep PV, Jayashree B, Mishra A, Mishra SK . Systematic review of primary hyperparathyroidism in India: the past, present, and the future trends. Int J Endocrinol. 2011;2011:921814.
Bilezikian JP, Meng X, Shi Y, Silverberg SJ . Primary hyperparathyroidism in women: a tale of two cities—New York and Beijing. Int J Fertil Womens Med. 2000;45:158–165.
Zhao L, Liu JM, He XY, Zhao HY, Sun LH, Tao B, Zhang MJ, Chen X, Wang WQ, Ning G . The changing clinical patterns of primary hyperparathyroidism in Chinese patients: data from 2000 to 2010 in a single clinical center. J Clin Endocrinol Metab. 2013;98:721–728.
Silverberg SJ, Bilezikian JP . “Incipient” primary hyperparathyroidism: a “forme fruste” of an old disease. J Clin Endocrinol Metab. 2003;88:5348–5352.
Lowe H, McMahon DJ, Rubin MR, Bilezikian JP, Silverberg SJ . Normocalcemic primary hyperparathyroidism: further characterization of a new clinical phenotype. J Clin Endocrinol Metab. 2007;92:3001–3005.
Rao DS, Wilson RJ, Kleerekoper M, Parfitt AM . Lack of biochemical progression or continuation of accelerated bone loss in mild asymptomatic primary hyperparathyroidism: evidence for biphasic disease course. J Clin Endocrinol Metab. 1988;67:1294–1298.
Cusano NE, Maalouf NM, Wang PY, Zhang C, Cremers SC, Haney EM, Bauer DC, Orwoll ES, Bilezikian JP . Normocalcemic hyperparathyroidism and hypoparathyroidism in two community-based non-referral populations. J Clin Endocrinol Metab. 2013 May 20. [Epub ahead of print]
Eastell R, Arnold A, Brandi ML, Brown EM, D'Amour P, Hanley DA, Rao DS, Rubin MR, Goltzman D, Silverberg SJ, Marx SJ, Peacock M, Mosekilde L, Bouillon R, Lewiecki EM . Diagnosis of asymptomatic primary hyperparathyroidism: proceedings of the third international workshop. J Clin Endocrinol Metab. 2009;94:340–350.
Silverberg SJ, Lewiecki EM, Mosekilde L, Peacock M, Rubin MR . Presentation of asymptomatic primary hyperparathyroidism: proceedings of the third international workshop. J Clin Endocrinol Metab. 2009;94:351–365.
Cusano NE, Silverberg SJ, Bilezikian JP . Normocalcemic primary hyperparathyroidism. J Clin Densitom. 2013;16:33–39.
A Amaral LM, Queiroz DC, Marques TF, Mendes M, Bandeira F . Normocalcemic versus Hypercalcemic Primary Hyperparathyroidism: More Stone than Bone? J Osteoporos. 2012;2012:128352.
Bilezikian JP . Primary hyperparathyroidism. Endocr Pract. 2012;18:781–790.
Campennì A, Ruggeri RM, Sindoni A, Giovinazzo S, Calbo E, Ieni A, Calbo L, Tuccari G, Baldari S, Benvenga S . Parathyroid carcinoma presenting as normocalcemic hyperparathyroidism. J Bone Miner Metab. 2012;30:367–372.
Stein EM, Dempster DW, Udesky J, Zhou H, Bilezikian JP, Shane E, Silverberg SJ . Vitamin D deficiency influences histomorphometric features of bone in primary hyperparathyroidism. Bone. 2011;48:557–561.
Rao DS, Honasoge M, Divine GW, Phillips ER, Lee MW, Ansari MR, Talpos GB, Parfitt AM . Effect of vitamin D nutrition on parathyroid adenoma weight: pathogenetic and clinical implications. J Clin Endocrinol Metab. 2000;85:1054–1058.
Acknowledgements
Some of this work as it pertains to the presentation of Primary Hyperparathyroidism in the United States was supported by a grant from the NIH: DK32333. This study was also supported by the National Natural Science Foundation of China (81070693 and 81200647). We acknowledge the vision of Dr. Clyde Wu who has been the inspiration for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liu, Jm., Cusano, N., Silva, B. et al. Primary Hyperparathyroidism: A Tale of Two Cities Revisited — New York and Shanghai. Bone Res 1, 162–169 (2013). https://doi.org/10.4248/BR201302005
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.4248/BR201302005
This article is cited by
-
Widespread presentation of brown tumors mimicking multiple myeloma
European Journal of Hybrid Imaging (2023)
-
Minimally Invasive Parathyroidectomy as the Surgical Management of Single Parathyroid Adenomas: A Tertiary Care Experience
Indian Journal of Otolaryngology and Head & Neck Surgery (2023)
-
Multidisciplinary team efforts to improve the pregnancy outcome of pregnancy complicated with primary hyperparathyroidism: case series from a single hospital
BMC Pregnancy and Childbirth (2021)
-
Effectiveness of anti-osteoporotic treatment after successful parathyroidectomy for primary hyperparathyroidism: a randomized, double-blind, placebo-controlled trial
Langenbeck's Archives of Surgery (2019)
-
Primary hyperparathyroidism
Nature Reviews Endocrinology (2018)