Key Points
-
An update for practising dentists regarding the indications, applications and use of contemporary crown and bridge systems.
-
Informs the reader about CAD/CAM production methods.
-
Provides revision of 'ideal' tooth preparation guidelines for all-ceramic crown/bridge systems and new specifically formulated luting cements.
-
Concludes that all-ceramic bridgework can be routinely used in all clinical settings.
Abstract
This paper reports the utility of an all-ceramic crown and bridge system, Lava™ from 3M/ESPE™. The background of the case is discussed and the clinical findings and treatment of a patient are outlined. This case illustrates that state of the art zirconium oxide CAD/CAM manufactured frameworks with the latest ceramic systems are a user friendly, highly aesthetic alternative to metal-ceramic restorations.
Similar content being viewed by others
Introduction
For aesthetic crown and bridgework, metal-ceramic is still the most widely prescribed material among dental surgeons both in general practice and most likely in hospital environments as well.1 Metal-ceramic restorative methods have been reliably used since their inception in the 1950s when Brecker described the baking of porcelain onto gold.2 Over half a century of refinements have led to reliable, strong crowns/bridges with satisfactory aesthetics. Recently, metal substructures have been minimised and gold rich alloys used to maximise the natural hue, value and chroma of artificial units. While metal-ceramic systems still represent a high strength mode of treatment associated with a good long term success rate, there are a number of disadvantages, mainly, the extent of tooth preparation (which is common to all crown and bridge systems that use metal or ceramic substructures and which may compromise pulpal health), aesthetics and allergy (specifically to nickel). The past decade has seen the emergence of a number of novel all-ceramic crown and bridge systems, capable of restoring anterior, posterior and multiple units. The search for new methods has been driven, in part, by patients who have increasingly high expectations in the arena of aesthetic dentistry and may also have concerns about the biocompatibility of metals intra-orally. Improvements in high strength all-ceramic technology were noted by the profession with the advent of computer-aided design/milling (CAD/CAM) systems. Procera (Nobel Biocare, Sweden) is one such example, first described in 1993,3 employing, as the title of the paper states: 'A dense-sintered, high purity alumina coping with porcelain'. Research has shown that this type of all-ceramic crown is able to resist fracture during function/parafunction, both at anterior and posterior sites, notably under higher stresses.4 Other new systems include the high precision multi-unit contact scanning Procera Forte (Nobel Biocare) and both Cercon (Degudent) and DC-Zirkon (DCS) use similar CAD/CAM manufacturing methods.
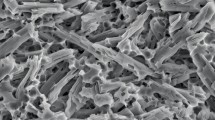
Recently, 3M ESPE (Seefeld, Germany) launched the LAVA crown and bridge system. LAVA is one of the first all-ceramic systems to use CAD/CAM technology with optical scanner devices to create an infrastructure in zirconia, subsequently finished with veneering ceramic. During the manufacturing process, a stabilising agent, yttrium oxide (Y2O3) is added to zirconium oxide and the resultant material used to fabricate the infrastructure is termed yttrium tetragonal zirconia (ZrO2) polycristals (Y-TZP). The Y-TZP exhibits excellent material properties for clinical application by, resisting fracture by a process termed 'transformation toughening', whereby any stress fractures created within the material cause a transformation of configuration of the zirconia to another one of its three forms, thereby minimising crack propagation.5 Sorenson et al. (2000) also demonstrated that the polycrystalline microstructure of the zirconia ceramic resists hydro-fatigue (degradation of the material by water in saliva).6
The design and manufacturing process firstly involves optical scanning and digitising of the dies (created from the master impression of the prepared teeth/cores), bite registration, and where applicable the bridge pontic region (from the master model), in order to duplicate the dimensions of the margin/s with precision. The scanned 3D images of the dies are then used to design the substructure, prompted by computer software (CAD) which has a database of pontic designs and critical, minimum dimensions of connectors set at 9 mm2. The CAD unit is linked to a robotic CAM centre that machines a partially sintered Y-TZP block to the design specifications (Fig. 1). The marginal adaptation of LAVA substructures has been investigated by Hertlein et al. who reported a range of between 40 to 70 microns,7 although recent correspondence from 3M ESPE has confirmed that with optical scanning, a marginal fit of 25 microns and final fit of 25 microns plus/minus 12 microns is reliably achievable. Hauptman et al. undertook investigations to ascertain the mechanical properties of the Y-TZP ZrO2 substructures with respect to strength, toughness, optical properties and subcritical crack propagation (ie longevity). They concluded that the material exhibited outstanding mechanical and optical properties showing a failure rate of just 2% after five years at a constant load of 450 Mpa, suggesting the utility of Y-TZP ZnO2 for posterior bridges is possible.9
Edelhoff and Sorensen (2002) evaluated light transmission through ceramic infrastructures and found that Y-TZP offers less light transmission than the most transluscent ceramic, Inceram Spinell (MgAl2O4), but was better than Inceram zirconia and far superior to any metal ceramic system.10 One advantage is the shade of the ceramic infrastructure, which can be selected in one of seven Vita shades. This eliminates a white collar (of pure unstained zirconia) at the cervical region of the restoration, which is important as the veneering ceramic is thinnest in cross-section at this point. Furthermore, with a metal-free, colour-matched base, without the need for bulky opaque layering, the resultant restoration exhibits an ideal balance between strength and aesthetics (with enhanced translucency) (Fig. 2).
Long term clinical data relating to the longevity and performance of LAVA restorations intra-orally are not yet available. However, there are a number of well reported ongoing trials, the longest of which has been at The University of Zurich, whose research unit has completed a three-year recall for all study patients, with no instances of bulk fracture reported.11
Tooth preparation guidelines for all-ceramic systems
The general preparation design principles are similar to conventional metal or metal-ceramic systems. However, due to the unique nature of the material and CAD/CAM production of the all-ceramic restorations, certain specific criteria must be met. These include:
-
For anterior teeth: 1.5-2 mm incisal reduction, 1.0-1.5 mm lingual reduction, 1.0-1.5 mm labial reduction
-
For posterior teeth: 1.5-2 mm occlusal reduction and 1-2 mm axial reduction
-
A 4 degree minimal taper is required to allow the scanner to make an accurate reading for single unit preparations, while for bridge abutments a 6 degree taper is recommended.
-
Rounded internal line angles, no sharp edges or undercuts
-
Deep chamfer or 'shoulder with rounded internal angle' are the finishing margins of choice
-
Maintenance of a straight line axial wall at the cervical third of the palatal surface of anterior preparations to maximise retention and resistance form
-
Feather edge, gutter margins (lipping) and 90 degree shoulder must be avoided.12,13
In general, preparation margins should be placed supragingivally. This applies to all indirect restorative treatment, aids impression taking and preserves periodontal health. However, the advent of all-ceramic restorations has been driven by aesthetics, thus when restoring the aesthetic zone, finishing margins may be placed approximately 0.5 to 1 mm subgingivally in order to mask the union between margin and dentine.
Preparation is undertaken with high speed diamond burs, a selection of which is listed in Table 1. This essentially comprises round-ended tapered diamonds (1 mm tip) of varying length and diameter and a rugby-ball diamond to facilitate adequate lingual reduction at the cingulum area of anterior teeth.
Due to the complexity of bridgework, a number of additional considerations must be considered, including: abutment height, sufficient interocclusal clearance for the substructure (plus veneering ceramic), sufficient height and width for the connectors (3 mm by 3 mm minimum), 0.5 mm wall thickness for posterior copings (0.3 mm for single unit anterior crown), lingually positioned connectors for anterior bridgework to achieve an aesthetic veneering with more refined labial contours. Furthermore, all-ceramic bridgework is contra-indicated if there is differential bone support between abutment teeth (ie one tooth exhibits mobility), as the lack of stability and leverage caused by the mobile tooth may produce additional stress on the connectors during mastication. All-ceramic bridgework in the chronic bruxist should also be considered with great care. Finally, unlike metal-ceramic bridgework, if a Y-TZP substructure exhibits poor marginal adaptation on the abutments at try-in, an impression must be retaken and a new framework fabricated as it is not possible to modify the substructure (in the way that metal-work may be cut, indexed and soldered).14
Laboratory considerations
After a high wear resistance model/die has been cast and the bite registration trimmed, both are digitised by the LAVA scanner and may be viewed three-dimensionally on screen at the milling centre. The design of the crown or bridge substructure is computer aided to ensure high efficiency and where appropriate, computer-guided, to ensure optimal dimensions of the connector. The resultant image can be customised to create an ideal simulated prosthesis, prior to machining. The substructure is milled from a pre-sintered blank of Y-TZP based ceramic (Fig. 3). Additionally, the shade of the core substructure can be selected from one of seven Vita shades, to further enhance the aesthetic result of the prosthesis. At present there are approximately 100 laboratories that handle the Lava system in the UK and four recognised milling centres, thus specialist laboratories would provide the substructure, before returning it to a regional laboratory for the addition of veneering ceramic (in this case, Lava Ceram 3M ESPE) (Fig. 4).15The skill of the ceramist is critical to the aesthetic outcome.
Immediately after tooth preparation, all vital dentine surfaces were sealed with dentine bonding resin to seal dentinal tubules, offering protection and increasing final bond strength. At the fit stage, after the provisional restorations were removed, bonding resin was re-applied.
Cementation
Due to the precise nature of CAD/CAM fabrication, crown and bridgework formed using this method has a consistent and excellent accuracy of fit, with tolerances reported as low as 50 to 100 μm. Furthermore, some milling centres are adding a gap to the restoration to better accommodate the cement lute (the resultant fit is still less than 100 μm).16 Although there are a wide range of cements currently available, including zinc phosphate, carboxylate, glass ionomer, hybrids (resin modified GIC/compomers), it is the composite resin type, in particular a self-adhesive, dual cure universal resin cement, called Rely X™ Unicem (3M™ ESPE™) that is the luting cement of choice. The advantages of using this type of adhesive luting material include: ease of handling, high bond strength, high aesthetics (shade A1, A2, A3, opaque/translucent), suitable for ceramic and composite resin restorations and all shades are radiopaque. Sorenson et al. undertook a study to evaluate the bond strengths of eight cements (including Panavia) and found that Rely X Unicem™ exhibited the maximum adhesion values when used to cement zirconia-based ceramics.17 Unlike other systems, no pre-treatment steps are required; etching or the use of primer or bond resins are not necessary. The preparation must be free from any residue or temporary cement and gently dried (not desiccated). Appropriate shade selection is followed by automated mixing of the applicap, administration into the pre-sandblasted, fitting surface of the prosthesis and seating onto the prepared site. As the Unicem is dual cured, the chemical curing may be supplemented by light activation if deemed clinically necessary.
Clinical studies to date
At present there are very few data relating to the clinical outcomes and long term service of Lava crown and bridgework. This seems to be related to its recent emergence onto the market and the lack of laboratory provision. However, at IADR 2004/5, 12 abstracts were published reporting different positive outcomes of the Lava system from laboratory testing and three clinical case reports were presented from 2003 to 2005. The case reports are summarised in Table 2.
Case report
A 78-year-old lady was referred to our department to manage failing bridgework, failed endodontic treatment for the enucleation of a radicular cyst associated with the mesial surface of the upper right first molar, caries and chronic plaque-induced periodontitis. For the purpose of this report, the case study will focus solely on the restoration of the upper arch with the Lava system.
At presentation the upper quadrant exhibited a fixed metal-ceramic bridge (double abutment UR1/UR2), with fractured ceramic at the UR3 pontic and secondary caries at all margins. At the upper left quadrant, UL1 to UL6 had been restored with a fixed (double abutted) acrylic bridge, again, with associated caries and periodontal disease (Fig. 5).
At the completion of the provisional treatment stage, periodontal therapy had been undertaken, all carious lesions managed, diet analysis, oral hygiene therapy and periodontal review appointments were undertaken and both upper bridges were replaced with provisionals (without double abutment), exhibiting excellent marginal fit. Oral health was established in the lower arch. The occlusion was analysed pre-operatively, both clinically and with the aid of mounted study models on a semi adjustable articulator. The patient was asked to provide a photograph to show the morphology of her own natural teeth, prior to crown/bridgework. A diagnostic wax-up was carried out and modified at the chair-side with the patient, until the final outline form of the new restorations were deemed to be aesthetically satisfactory. At the tooth preparation/registration stage, the form of the abutment teeth were refined using a Shofu 835-1 round ended tapered diamond (coarse and superfine) before impression taking and laboratory manufacture at Techceram (Shipley, UK) (Figs 6, 7).
At the fit stage, all abutment teeth were cleaned of temporary cement and all restorations cemented with Rely X Unicem at one visit. To avoid double abutment, the occlusion (which exhibited an incisor relationship of Class 2 division 1 with 3 mm overjet) and the integrity, bulk and alveolar bone support of the upper laterals were critically evaluated. It was deemed that a clinical gain would be made by restoring the upper arch with single unit crowns on upper central incisors, with short span three and four unit bridges posteriorly, due to the pronounced mesial drift of both upper first molars (Figs 8, 9).
Discussion and conclusion
It would seem that feedback from laboratory based studies and the very few reported clinical trials show great promise for the use of the Lava all-ceramic crown and bridge system. The Lava system provides high strength copings with veneering ceramics of excellent aesthetic value and due to the metal-free nature of the prosthesis the incidence of allergenic reactions among atopic patients is likely to be less. Due to recent advancements in CAD/CAM technology and the nature of the Y-TZP ceramic, the Lava system offers a wider range of restorative options, including, for the first time, all-ceramic posterior bridgework. As with all indirect restorative procedures, case selection, pre-operative management and highest levels of accuracy are mandatory during tooth preparation and registration. From the preliminary findings of this report, it appears that further long term clinical data are required to support the wealth of laboratory studies. However for the purpose of this case report, it may be concluded that the Lava system provided seamless restorations, exhibiting excellent marginal fit, occlusal form and aesthetics (Fig. 10). It is therefore possible that Lava may represent the next generation of first line all-ceramic systems for full mouth restoration.
References
GDS Treatment Items Year Ending March 2003. Dental Practice Board, Eastbourne, UK.
Brecker S C . Porcelain baked to gold: a new medium in prosthodontics. J Prosth Dent 1956; 6: 801–810.
Andersson M, Oden A . A new all-ceramic crown. A dense-sintered, high purity alumina coping with porcelain. Acta Odontol Scand 1993; 51: 59–64.
Wagner W C, Chu T M . Biaxial flexural strength and indentation fracture toughness of three new dental core ceramics. J Prosth Dent 1996; 76: 140–144.
Sorenson J A . The LAVA system for CAD/CAM production of high-strength precision fixed prosthodontics. Quint Dent Technology 2003; 26: 57–67.
Sorenson J A, Berge H X, Edelhoff D . Effect of storage media and fatigue loading on ceramic strength. J Dent Res 2000; 79: 271.
Hertlein G, Hoscheler S, Frank S et al. Marginal fit of CAD/CAM manufactured all-ceramic zirconia prosthesis. J Dent Res 2001; 80: 492.
Rafelt J . Personal communication. August 2006.
Hauptmann H, Suttor D, Frank H et al. Material properties of all ceramic zirconia prostheses. J Dent Res 2000; 79: 271.
Edelhoff D, Sorensen J . Light transmission through all ceramic framework and cement combinations. J Dent Res 2002; 81.
Robert Kelly J . Dental ceramics: current thinking and trends. Dent Clin N Am 2004; 513–530.
Raigrodski AJ . Clinical and laboratory considerations for the use of CAD/CAM Y-TZP-based restorations. Pract Proced Aest Dent 2003; 15: 469–476.
LAVA, 3M ESPE Clinical Preparation guidelines 2006: www.3MESPE.com.
Boudrias P . The yttrium tetragonal zirconia polycristals (Y-TZP) infrastructure: The new chapter in the search for a metal framework replacement. J Dent Quebec 2005; 42: 172–176.
Burke F J T, Palin W . Trends in indirect dentistry: CAD/CAM technology. Dental Update 2005; 32: 566–572.
Sorenson J A . The LAVA system for CAD/CAM production of high-strength precision fixed prosthodontics. pp 57–66. Chicago: Quintessence Publishing Co, 2003; 26.
Sorenson JA . Shear bond strength to zirconium oxide ceramic. J Dent Res 2002; 81: 413.
Raigrodski A J, Chiche G J, Potiket N et al. Clinical efficacy of Y-TZP based posterior fixed partial dentures. J Dent Res 2005; 226.
Pospiech P R, Rountree P R, Northdurft F P . Clinical evaluation of zirconia-based all ceramic posterior bridges: 2 year results. J Dent Res 2003; 817.
Pospiech P R, Northdurft F P . Long-term behaviour of zirconia-based bridges (Lava): Results after three years in service. Continuing Education in Dentistry 2004; 230.
Acknowledgements
The authors would like to thank Dr John Rafelt Senior Scientific Affairs Executive (3M ESPE Dental Products 3M Health Care Limited, UK) and Techceram (1 Acorn Park, Charlestown, Shipley, UK) who undertook all laboratory work.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Barnfather, K., Brunton, P. Restoration of the upper dental arch using Lava™ all-ceramic crown and bridgework. Br Dent J 202, 731–735 (2007). https://doi.org/10.1038/BDJ.2007.534
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/BDJ.2007.534
This article is cited by
-
Comparison of implant versus tooth-supported zirconia-based single crowns in a split-mouth design: a 4-year clinical follow-up study
Clinical Oral Investigations (2016)
-
Beyond the pale
British Dental Journal (2009)
-
Three-year clinical prospective evaluation of zirconia-based posterior fixed dental prostheses (FDPs)
Clinical Oral Investigations (2009)
-
Source of concern
British Dental Journal (2007)