Key Points
-
Compared to the general population, a higher proportion of people with multiple sclerosis report being registered at a dental practice.
-
People with multiple sclerosis experience difficulties in attending a dental practice and in maintaining oral health.
-
Initiatives are required in order to increase awareness of the importance of oral health to the quality of life of people with multiple sclerosis and ensure access to dental services for individuals with physical disabilities.
Abstract
Objective To determine the impact of multiple sclerosis (MS) on patient attendance at dental practices and maintenance of oral health.
Design A cross-sectional postal questionnaire-based study.
Setting Leicestershire, United Kingdom.
Subjects and methods People with MS in Leicestershire identified from local health authority records (n = 476).
Main outcome measures Number registered at dental practice, frequency of attendance, issues and perspectives relating to attendance and maintenance of oral health.
Results A response rate of 61% (n = 289) was obtained. When compared to the general population, a higher number of people with MS were registered with a dentist (49%:88%) and displayed more frequent practice attendance (71%:81%) in the past year. People with MS reported difficulties in attending a dentist and maintaining oral health, which were exacerbated by deterioration in general health. Problems relating to reduced personal mobility had the greatest impact on attendance.
Conclusions MS has a negative impact on perceived patient attendance and maintenance of oral health. Patients with a progressive disability could benefit greatly from the provision of preventive oral health care. The importance of seeking care earlier rather than later needs to be emphasised to both professionals and patients alike. Further efforts are required to increase awareness of the importance of oral health to the quality of life of people with MS and ensure that individuals with physical disabilities receive the same access to dental services as the able-bodied.
Similar content being viewed by others
Introduction
There are an estimated 85,000 people living with multiple sclerosis (MS) in the UK, with the highest prevalence occurring in Scotland.1 The cause of MS is unknown, but it is believed to be an inflammatory condition in which autoimmune attack is associated with a breakdown of the normal barrier separating blood from the brain.2 People living with MS exhibit a wide spectrum of physical signs and symptoms, which are often related to the severity and form of their disorder.1 These can include loss of vision from optic neuritis, isolated numbness, leg weakness and urinary sphincter disturbance from spinal cord disease, or disturbance of coordination and eye movements due to brain-stem inflammation.3 Due to the complex nature of this disease, it is impossible to predict the actual symptoms a patient may experience or to what extent their health will deteriorate over time.4 People with MS were found to have a lower quality of life when compared both to other disabled groups5 and the general population.6 Yet there still appears to be a strong need for health care providers and carers to understand the difficulty people with MS can experience in performing routine activities of life.
When the association between oral health and quality of life has been reported with the needs and priorities for oral health care, these have been shown to vary significantly for people with a disability compared to the general population.7,8,9 It has been reported that individuals with MS have special needs in relation to dental care,10 and often face difficulties in maintaining oral hygiene and accessing care, placing them at increased risk of developing oral health problems.9,11 Dental care for people with MS has been poorly co-ordinated, which may be a result of their dental needs being perceived as of low priority by carers and the wider NHS. The physical inability of an individual with MS to clean their teeth without assistance and the effects of medication on the oral environment9 can create oral health problems, the impact of which can be significantly deleterious to quality of life. There are increasing demands to facilitate access to dental health services for physically disabled patients and to reinforce the role of health professionals in supporting and improving the oral health of people with MS.10
A study that compared the oral health of people with MS to a comparison group of individuals of a similar age and sex12 found that people with MS had a nine percent excess risk of decayed, missing or filled teeth (OR 1.09; 95% CI 1.00, 1.18; P = 0.049). It is particularly important for people with MS to avoid dental infection and trauma, as these may cause a relapse of the condition.13,14 Patients with MS have made calls for the provision of non-amalgam fillings, due to concerns regarding the mercury content of amalgam,15 despite the lack of evidence to support any aetiological association between mercury exposure and MS.12,16,17 Progression of the disease with involvement of the facial muscles further complicates treatment if dentures are required.18 It may be assumed that patients with MS could be at risk of experiencing inequalities in dental care and that the oral health needs of this subgroup must not be overlooked.
The aims of this study were to explore the impact of MS on patient attendance and maintenance of oral health, and to identify factors that may act as potential barriers to attendance.
Methods
The findings of a literature review, a general dental practitioner survey in Leicestershire,19 focus group discussions and informal discussions with key stakeholders were used to develop a questionnaire. The questionnaire was piloted by people with MS who had previously been involved in informal and focus group discussions to ensure that the questions were appropriate, clear, understandable and had both face and content validity.20 Full ethical approval was granted from the Leicestershire Research Ethics Committee.
The questionnaire, accompanied by an information sheet providing details of the study, was posted to people with MS identified using the in-patient records held by Leicestershire Health Authority, based on a diagnosis code for MS. Subjects were excluded from the study if they indicated they did not have MS or did not live in Leicestershire. A follow-up mailing was sent after eight weeks. A total of 289 completed questionnaires were received from the 476 subjects eligible to take part, a response of 61%.
The primary outcome measure was frequency of attendance at the dental practice by people who have MS. Secondary outcome measures included the impact of MS on attendance, reasons for attendance and barriers to receiving dental care. The ability to walk was used as a marker for disability, as the postal questionnaire was not deemed as being a suitable instrument by which to measure disability.
In order to increase the accuracy of data input, a form identical to the questionnaire was designed and the data were double-entered into Access software and were then transferred to SPSS. Differences between groups of individuals in terms of continuous variables were assessed using a two-sample t-test. Association between categorical variables was assessed by calculating an odds ratio (OR) and 95% CI and by using a chi-square test.
Results
Responders compared to non-responders
There was no difference between the gender and age distribution of responders and non-responders. Of the responders, 25% were male and 75% female, compared to 28% male and 72% female in the non-responding group (P = 0.407). The mean age of the responders was 51.5 years (SD = 12.7), compared to 52.5 years (SD = 14.2) for the non-responders (P = 0.387).
Attendance pattern
A large number of respondents (88%) were currently registered with a dentist. Seventy-four percent of respondents reported attending on a regular basis, with 68% having attended in the past 6 months. No differences in attendance pattern or reason for their last visit were observed between males and females (P = 0.527) with the most common reason for the last visit being a regular check up (70%) (Table 1). People who thought that they were regular attendees reported that they were 32 times more likely to be a regular attendee (OR = 32.0; 95% CI 14.8, 69.0; p < 0.001).
Oral hygiene practices
The vast majority of respondents (97%) reported cleaning their teeth regularly, performing this activity once (34%), or twice or more (66%) times per day. Women were three times more likely to clean their teeth frequently than men (OR = 3.20; 95% CI 1.74, 5.90; p < 0.001).
Impact of MS on dental attendance
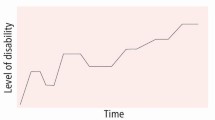
Participants rated their general health as excellent (1%), very good (6.5%), good (44%), poor (37%) and very poor (11.5%). Self-reported general health and practice attendance pattern were associated, with 76% of respondents who rated their health as good to excellent having made their most recent visit to a dentist within the last 6 months, in comparison with only 56% of individuals who reported poorer general health (Fig. 1). The effects of general health and mobility on oral health needs and behaviours of people with MS are summarised in Table 2.
Potential barriers to receiving dental services
Some respondents considered it difficult to get access to the building (21%), waiting room (11%) and surgery (16%) at the dental practice they attend. When asked to consider the facilities at their surgery, 38% rated the practice as having suitable parking spaces, 63% suitable access and 48% suitable toilet facilities. However, only 4% attended a practice because it had special facilities and only 5% had ever received a domiciliary visit. Fewer had been referred to the community dental service (CDS) (3%), with only 17% being aware that these services were available. A small proportion of people (10%) were referred by their dentist to specialised clinics at the Leicester Royal Infirmary, the most common being for neuralgic pain in the face and jaw.
Suggestions to improve dental services for MS patients
The majority of individuals were happy with the care that they received from their dentist (95%) because the practice staff were understanding of the difficulties encountered when attending the dentist. Changes participants would like to see made to dental services included improved provision of information on services (56%), increased accessibility of practices for those with personal mobility problems (11%), including the availability of disabled parking (6%). It was suggested that the availability of hoists to aid transfer from the wheelchair to the dental chair would also reduce barriers to attendance. Improvements in the availability and frequency of transport suitable for wheelchair users (4%) would also facilitate attendance at a surgery. A small proportion (2%) of respondents suggested that domiciliary visits should be available to the housebound.
Discussion
The aim of the study was to identify whether having MS had an impact on the ability of patients to attend the dentist, and the maintenance of oral health. It also aimed to identify reasons for and possible barriers to attendance at the dentist.
It is unlikely that the subjects participating in this survey are a representative sample of all MS patients, because they were selected from inpatient records. However, it is this subgroup of MS patients, in active receipt of treatment, which may be likely to experience the greatest difficulty accessing services as their condition deteriorates. Thus, this group is likely to be representative of those who have an unmet need for services such as dental treatment.
Just over 60% of questionnaires were returned, a rate which is comparable to the response obtained from other disabled groups.21,22,23 The non-respondents may potentially produce bias in the results, but the current study found that there was no difference in the age or sex of non-respondents compared to respondents.
The sample composition was three quarters female and a quarter male, suggesting that the sample was biased towards females. However, this distribution is in keeping with the general prevalence of MS, which occurs up to three times more frequently in females.24,25
People with MS are frequently proactive, with many seeking alternative treatments, dietary regimes and exercise to maintain and improve their general health.4 Therefore, it was not surprising that nearly 90% of participants were currently registered with a dentist. This was much higher than the proportion in the general population in England and Wales, where less than 50% reported being registered with a dentist.26 As expected, women reported cleaning their teeth more frequently than men; a finding which is comparable to the general population.27
It is clear that people with MS exhibit many similar characteristics to the general population in relation to dental health, such as attendance pattern and receiving treatment under the NHS. Comparisons with the general population are summarised in Table 1. Although people with MS were more likely to attend the dentist for a check up and receive treatment either privately or in a combination of privately/under the NHS, they reported cleaning their teeth less frequently than the general population.27 It would also appear that people with MS were less likely to be edentate, but more likely to have a denture in addition to natural teeth than the general population.28 This supports the findings of earlier work,12 which found that people with MS had a higher number of decayed, missing and filled teeth when compared to age-matched controls. Although this study demonstrates that oral health is important to people with MS, such patients appear to have difficulty in maintaining their oral health and report the need for assistance in their dental care as their condition deteriorates. Therefore, poorer oral health may be experienced due to the complexity of symptoms and access to appropriate care rather than a lack of personal interest in oral health.
The ability to walk has been shown in this study to have a significant association with many aspects of dental attendance and maintaining oral health. The ability to walk was used as a measure of disability, as it is not possible to use a measure such as the Expanded Disability Status Scale (EDSS)29 to determine the level of disability with a postal questionnaire. As the ability to walk decreased, individuals were less likely to either attend the dentist or consider themselves to be regular attendees. They also cleaned their teeth less frequently, were less interested in receiving information about caring for their teeth and had increased problems accessing the building, waiting room and surgery.
Self-reported poor general health was shown to have an association with attendance at the dentist and maintaining oral health. People who reported that they had poor general health were more likely to need help caring for their teeth, and be either edentate or have a partial denture, than people with MS who reported good general health, or those in the general population.27This group also had problems accessing surgery buildings and were more likely to be unaware of services such as the CDS or domiciliary services.
A large percentage of participants reported that the dental practice they attended lacked facilities such as suitable parking, access and toilets. However, less than 5% of participants attended dental practices because they offered special facilities. It would appear that patients with MS prefer to attend a dentist because it is the family dentist or it is near their home or place of work rather than find a new practice, which would be more accessible. This may be related to the difficulty of finding an NHS practice accepting new patients, as a high percentage of participants reported receiving NHS treatment. However, it may also be related to the fact that patients have built up a relationship with the entire dental team, who over the years have developed an understanding of MS in terms of symptoms and treatment provision.
The main barriers to dental care for the general population were reported as being financial cost, fear and anxiety.30,31 For this group, structural barriers such as a lack of suitable parking, access and toilet facilities, became more apparent as level of disability increased. As found in earlier studies, the attitude of staff, lack of information on facilities available and high financial cost also prohibited people from attending the dentist.32,33,34,35,36,37,38 This study also highlights the general lack of knowledge as to the availability of and entitlements to services for people with special needs. Part III of the Disability and Discrimination Act (1995)39 makes it unlawful for a service provider to treat a disabled person less favourably for a reason related to their disability. From October 2004, where services are inaccessible to the physically disabled, practices are legally required to make reasonable adjustments in order to comply with the Act.40,41
At the time of study, dentists were paid per item of treatment. Thus, providing care to individuals with a disability, who may take more time to treat than the average member of the public, might have presented a financial disincentive to GDPs and may have posed a further barrier to care for the physically disabled patient. This should no longer be an issue under the new dental contract, and may serve to improve access to care for physically disabled people in the GDS.
Respondents were unaware of the availability of services such as the CDS, which provides dental treatment to special needs patients who cannot obtain treatment in a practice setting. Individuals did not appear to consider the possibility that their dentist may offer domiciliary care or would refer them to a practice with the necessary facilities, or to the CDS. Furthermore, it would appear that dentists may not be providing sufficient information to people with MS about the availability of these services. There is a possibility that patients may suffer unnecessary pain and discomfort because of a perceived lack of need both in the case of the individual and in those responsible for planning their pathway of care, or as a result of an acceptance that poor oral health is an inevitable part of disease progression or growing old, as found by a study of older adults.42 Raising the awareness of these issues may serve to facilitate the provision of a service that takes account of the variation in symptoms and needs of a patient with MS. The importance of oral health to the quality of life of individuals with a physical disability should be reinforced and recognised as being of high priority when commissioning patient centred dental services.43
Conclusion
This study has shown that people with MS consider their oral health to be important, with a large percentage attending the dentist frequently. Findings confirm that information on oral health specific to the symptoms of MS would increase awareness of the problems patients face maintaining their oral health from the onset of their condition.
References
Branas P, Jordan R, Fry-Smith A, Burls A, Hyde C. Treatments for fatigue in multiple sclerosis: a rapid and systematic review. Health Technol Assess 2000; 4: 1–61.
Raine C S, McFarland H F, Tourtellotte W W (eds). Multiple sclerosis: clinical and pathogenic basis. London, New York: Chapman & Hall Medical, 1997
Miller A. Diagnosis of multiple sclerosis. Semin Neurol 1998; 98: 309–316.
Halper J. Advanced concepts in multiple sclerosis nursing care. New York: Demos Medical Publishing, 2001.
Aronson K J. Quality of life among persons with multiple sclerosis and their caregivers. Neurology 1997; 48: 74–80.
Parkin D, Jacoby A, McNamee P et al. Treatment of multiple sclerosis with interferon beta: an appraisal of cost-effectiveness and quality of life. J Neurol Neurosurg Psychiatry 2000; 68: 144–149.
Gift H C, Redford M. Oral health and the quality of life. Clin Geriatr Med 1992; 8: 673–683.
Freeman J, Johnson J, Rollinson S, Thompson A, Hatch J. Standards of healthcare for people with multiple sclerosis. London: Multiple Sclerosis Society, 1997.
Cnossen M W. Considerations in the dental treatment of patients with multiple sclerosis. J Oral Med 1982; 37: 62–64.
Fiske J, Griffiths J, Thompson S. Multiple sclerosis and oral care. Dent Update 2002; 29: 273–283.
Griffiths J E, Trimlett H J. Dental status and barriers to care for adults with multiple sclerosis. Int Dent J 1996; 46 (4 Suppl 2): 445.
McGrother C W, Dugmore C, Phillips M J et al. Multiple sclerosis, dental caries and fillings: a case-control study. Br Dent J 1999; 187: 261–264.
Rapp N S, Gilroy J, Lerner A M. Role of bacterial infection in exacerbation of multiple sclerosis. Am J Phys Med Rehabil 1995; 74: 415–418.
Bamford C R, Sibley W A, Thies C et al. Trauma as an etiologic and aggravating factor in multiple sclerosis. Neurology 1981; 31: 1229–1234.
Siblerud R L, Kienholz E. Evidence that mercury from silver dental fillings may be an etiological factor in multiple sclerosis. Sci Total Environ 1994; 142: 191–205.
deShazer D O. The mercury-multiple sclerosis connection. J Colo Dent Assoc 1985; 63: 4.
Thompson C C. Dentistry and the multiple sclerosis patient. J Oral Med 1986; 41: 102–104.
Barker T. Role of health beliefs in patient compliance with preventive dental advice. Community Dent Oral Epidemiol 1994; 22: 327–330.
Baird W O, McGrother C, Abrams K R, Dugmore C, Jackson R J. Access to dental services for people with a physical disability: a survey of General Dental Practitioners in Leicestershire. Community Dent Health; In press.
Fink A. The Survey Kit. How to measure survey reliability and validity. Thousand Oaks: Sage, 1995.
Melton L J 3rd, Dyck P J, Karnes J L, O'Brien P C, Service F J. Non-response bias in studies of diabetic complications: the Rochester Diabetic Neuropathy Study. J Clin Epidemiol 1993; 46: 341–348.
Caradoc-Davies T, Hawker A. Rehabilitation services in the health sector: the perspectives of providers and consumers. Part 2. New Zeal Med J 1995; 108: 32–34.
Knight M, Stewart-Brown S, Fletcher L. Estimating health needs: the impact of a checklist of conditions and quality of life measurement on health information derived from community surveys. J Public Health Med 2001; 23: 179–186.
Sadovnick A D, Dyment D, Ebers G C. Genetic epidemiology of multiple sclerosis. Epidemiol Rev 1997; 19: 99–106.
McLeod J G, Hammond S R, Hallpike J F. Epidemiology of multiple sclerosis in Australia; with NSW and SA survey results. Med J Australia 1994; 160: 117–122.
Dental Practice Board. GDS Statistics section of the Dental Practice Board website [Web Page]. March 2005; Available at http://www.dpb.nhs.uk/gds/reg_index.shtml. (Accessed August 2005).
Kelly M. Adult dental health survey: oral health in the United Kingdom 1998. London: The Stationery Office 2000.
Nuttall N M, Bradnock G, White D, Morris J, Nunn J. Dental attendance in 1998 and implications for the future. Br Dent J 2001; 190: 177–182.
Kurtzke J F. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology 1983; 33: 1444–1452.
Nuttall N M, Steele J G, Pine C M, White D, Pitts N B. The impact of oral health on people in the UK in 1998. Br Dent J 2001; 190: 121–126.
Freeman R. Barriers to accessing and accepting dental care. Br Dent J 1999; 187: 81–84.
Land T. What patients think of dental services. Br Dent J 2000; 189: 21–24.
Wilson K I. Treatment accessibility for physically and mentally handicapped people – a review of the literature. Community Dent Health 1992; 9: 187–192.
Sjogren R, Nordstrom G. Oral health status of psychiatric patients. J Clin Nurs 2000; 9: 632–638.
O'Donnell D, Cooper J R. A pattern for the establishment of a unit for the dental treatment of the handicapped patient in the community based on such a unit in Hertfordshire. J Royal Soc Health 1984; 104: 125.
Storhaug K. Barriers to utilization of dental health services in a group of disabled Norwegian adults. Acta Odontol Scand 1988; 46: 246.
Nunn J H, Murray J J. Social and medical influences on dental care provision for handicapped children. Public Health 1987; 101: 391.
Russell G M, Kinirons M J. A study of the barriers to dental care in a sample of patients with cerebral palsy. Community Dent Health 1992; 10: 57–64.
The Disability and Discrimination Act 1995. London: HMSO, 1995, publication no. DL 160.
2004 – what it means to you. A guide for service providers. Stratford-upon-Avon: Disability Rights Commission, 2003.
You can make a difference: improving primary care services for disabled people. A good practice guide for primary care service providers. London: Disability Rights Commission & NHS, 2004.
Lester V, Ashley F P, Gibbons D E. The relationship between socio-dental indices of handicap, felt need for dental treatment and dental state in a group of frail and functionally dependent older adults. Community Dent Oral Epidemiol 1998; 26: 155–159.
Department of Health. Choosing better oral health: an oral health plan for England. London: Department of Health, 2005.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Baird, W., McGrother, C., Abrams, K. et al. Factors that influence the dental attendance pattern and maintenance of oral health for people with multiple sclerosis. Br Dent J 202, E4 (2007). https://doi.org/10.1038/bdj.2006.125
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bdj.2006.125
This article is cited by
-
Multiple sclerosis and its impact on dental care
BDJ Team (2022)
-
Multiple sclerosis and its impact on dental care
British Dental Journal (2021)
-
Investigating the relationship between multimorbidity and dental attendance: a cross-sectional study of UK adults
British Dental Journal (2019)
-
Factors influencing patients' continuing attendance at a given dentist
British Dental Journal (2015)
-
Access to special care dentistry, part 1. Access
British Dental Journal (2008)