Key Points
-
Describes a rare case that can occur in the practice setting.
-
Outlines management guidelines.
-
An anatomical/physiological explanation is proposed.
Abstract
A case of transient left lateral rectus nerve palsy, following an inferior alveolar nerve block to enable the surgical removal of a permanent mandibular left third molar tooth, is reported. The anatomy related to this case is considered together with suggestions for management of such patients.
Similar content being viewed by others
Introduction
Local anaesthetic is an integral part of every practising dentist's daily work. The complications of local anaesthetic are well known. This article documents the occurrence of a less common effect of an inferior alveolar nerve block that could easily occur in the practice environment. We look at the presenting factors, the anatomical considerations and the management of the patient.
Case report
A healthy 28-year-old female attended the oral and maxillofacial surgery department at Salisbury District Hospital as an outpatient for removal of the permanent mandibular left third molar tooth. 4.0 ml of 2% lidocaine with 1:80000 epinephrine was administered as a left inferior alveolar nerve block and long buccal nerve block using an aspirating syringe and a long needle. The thumb was placed on the anterior border of the ramus and the second finger on the posterior border. The needle entered the mucosa at the middle point of the thumb, slightly above the occlusal plane and lateral to the pterygomandibular raphe. The needle was advanced until it contacted the lingual and then withdrawn slightly before the solution was deposited. The long buccal block was performed by injecting 1.0 ml of local anaesthetic buccally and posteriorly to the second molar. No blood was noted in the LA cartridge upon aspiration. A few seconds after the nerve block the patient complained of feeling 'odd' and of double vision.
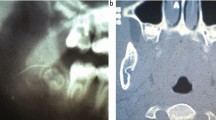
On examination, a palsy of the left abducent (VI cranial nerve) nerve was observed. The patient was unable to abduct the left eye. All other eye movements were normal (Figs 1 and 2). An area of skin blanching was also noted in a discreet area of skin of the upper left lip. Its inferior border was the left upper lip, its superior border the nose; laterally it extended just beyond the nasolabial groove and medially, the blanching did not cross the midline.
It was noted that profound analgesia of the mandibular teeth and of the lower lip had been achieved. The permanent mandibular left third molar tooth was surgically removed without event. The blanching resolved and the diplopia had improved markedly prior to the patient leaving the department. She was escorted home by a relative with instructions not to drive/operate machinery until her eyesight had returned to normal. Advice was given to contact the hospital by telephone if the diplopia had not resolved within a few hours.
The patient was contacted by telephone (with her consent) later that day and she reported that her diplopia had ceased and that her vision was normal.
Anatomical considerations/discussion
Several similar cases of palsy of the lateral rectus have been reported, although this has been more commonly related to superior alveolar nerve blockade.1The authors report 31 cases of ophthalmic complications after dental anaesthesia. These comprise a series of 14 of their own patients and 17 cases reported in previous literature. Only 35% of these cases resulted in diplopia secondary to inferior dental nerve blockade.
In this case, it is not possible to give a precise anatomical explanation, although the following suggestions can be offered.
Firstly, it is conceivable that the palsy resulted from diffusion of the local anaesthetic solution through tissue planes and into the orbit for direct action on the lateral rectus and/or the abducent nerve at the point that it innervates the muscle. This would require the solution to spread from a site near the mandibular foramen in the infratemporal fossa where the inferior alveolar nerve is located and thence anteriorly to the pterygomaxillary fissure and the pterygopalatine fossa, and then through the inferior orbital fissure into the orbital cavity. Even within the orbit, the solution would have to pass through orbital fat and fascia and around densely packed structures to end at the medial surface of the lateral rectus muscle where the abducent nerve is located. Although it is worth noting that, with the increased use of articaine, there is likely to be an increased incidence of ophthalmologic complications owing to its increased diffusion properties,2 the suggestion that diffusion caused the palsy seems to us to be unlikely and, should it have occurred, we might expect that the local anaesthetic solution would have affected the other nerves in the region (for example, the infra-orbital and zygomatic branches of the maxillary division of the trigeminal nerve as they travel through the inferior orbital fissure or other motor branches supplying the extra-ocular musculature).
Secondly, there could have been diffusion of the local anaesthetic solution from the infratemporal fossa and into the middle cranial cavity where the abducent nerve runs (ie in the medial wall of the cavernous sinus). This would require the solution to pass through the foramen ovale, foramen spinosum and/or sphenoidal emissary foramen in the roof of the infratemporal fossa and then to diffuse within or around the dura mater. This also seems to us to be improbable, especially since the solution would have to pass to the roof of the infratemporal fossa around/beneath the mass of the lateral pterygoid muscle and the deep head of the medial pterygoid muscle.
Thirdly, there might be an aberrant innervation to the lateral rectus muscle. However there is nothing in the literature to support this notion.
Fourthly, and most probably, the local anaesthetic solution could have affected the arterial supply in the region of the orbit and the infratemporal fossa. This view is supported by the blanching seen in the region of the upper left lip. This involved a discreet area of skin; its inferior border was the left upper lip, its superior border the nose and laterally it extended just beyond the nasolabial groove. Medially, the blanching did not cross the midline. The upper lip usually receives its blood supply from two major sources: the superior labial branches of the facial artery and from the infra-orbital artery as it passes from the orbit and onto the face through the infra-orbital foramen. The infra-orbital artery is a branch of the terminal part of the maxillary artery that has passed from the infratemporal fossa and into the pterygopalatine fossa. Another possibility is that there is an 'aberrant' origin and/or course for a meningeal branch of the maxillary artery that comes off the main trunk close to the mandibular foramen and that will affect the abducent nerve as it travels within the middle cranial cavity. Indeed, although it is generally accepted that the meningeal branches from the maxillary artery (usually a middle meningeal and an accessory meningeal artery) arise from the second part as the maxillary artery runs across the lateral pterygoid muscle in the roof of the infratemporal fossa, our experience in the dissection room has shown that the meningeal branches can arise from the first part of the maxillary artery as it enters the infratemporal fossa and runs close to the ramus of the mandible and the course of the inferior alveolar nerve. Although we have no direct evidence, this would be our preferred option to explain the lateral rectus palsy.
Conclusions
Previous articles have advised always aspirating prior to depositing the local anaesthetic solution. However, this case shows that even when aspirating such complications are still possible.
If a patient reports diplopia treatment should be stopped and the patient examined. The eye movements should be assessed and notes made. Reassure the patient this is a transient event which should resolve as the action of the local anaesthetic ceases. If diplopia persists at the end of the treatment the patient should be escorted home and advised against driving and operating machinery until normal sight returns. It is reasonable and sensible to telephone the patient later in the day to check it has resolved.
References
References
Marinho R O M. Abducent nerve palsy following dental local analgesia. Br Dent J 1995; 179: 69–70.
Penarrocha-Diago M, Sanchis-Bielsa J M. Ophthalmological complications after intraoral local anesthesia with articaine. Oral Surg Oral Med Oral Pathol Radiol Endod 2000; 90: 21–24.
Further reading
Berkovitz B K B, Holland G R, Moxham B J. Oral anatomy, histology and embryology (3rd edn). UK: Mosby, 2002.
Moore K L, Dalley A F. Clincially oriented anatomy (4th edn). UK: Lippincott, Williams & Wilkins, 2005.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Scott, J., Moxham, B. & Downie, I. Upper lip blanching and diplopia associated with local anaesthesia of the inferior alveolar nerve. Br Dent J 202, 32–33 (2007). https://doi.org/10.1038/bdj.2006.114
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bdj.2006.114
This article is cited by
-
Etiology and Pathophysiological Pathways of Ocular Complications Associated with Local Dental Anesthesia and Odontogenic Infections: A Systematic Review
Journal of Maxillofacial and Oral Surgery (2022)
-
A Randomized Controlled Study Comparing Efficacy of Classical and Gow-Gates Technique for Providing Anesthesia During Surgical Removal of Impacted Mandibular Third Molar: A Split Mouth Design
Journal of Maxillofacial and Oral Surgery (2017)
-
Latrogenic diplopia
International Ophthalmology (2014)
-
Amaurosis, ophthalmoplegia, ptosis, mydriasis and periorbital blanching following inferior alveolar nerve anaesthesia
Oral and Maxillofacial Surgery (2011)
-
Visual phenomena
British Dental Journal (2010)