Abstract
Aim:
To characterize pharmacokinetic-pharmacodynamic modeling of diclofenac in Freund's complete adjuvant (FCA)-induced arthritic rats using prostaglandin E2 (PGE2) as a biomarker.
Methods:
The pharmacokinetics of diclofenac was investigated using 20-day-old arthritic rats. PGE2 level in the rats was measured using an enzyme immunoassay. A pharmacokinetic-pharmacodynamic (PK-PD) model was developed to illustrate the relationship between the plasma concentration of diclofenac and the inhibition of PGE2 production. The inhibition of diclofenac on lipopolysaccharide (LPS)-induced PGE2 production in blood cells was investigated in vitro.
Results:
Similar pharmacokinetic behavior of diclofenac was found both in normal and FCA-induced arthritic rats. Diclofenac significantly decreased the plasma levels of PGE2 in both normal and arthritic rats. The inhibitory effect on PGE2 levels in the plasma was in proportion to the plasma concentration of diclofenac. No delay in the onset of inhibition was observed, suggesting that the effect compartment was located in the central compartment. An inhibitory effect sigmoid Imax model was selected to characterize the relationship between the plasma concentration of diclofenac and the inhibition of PGE2 production in vivo. The Imax model was also used to illustrate the inhibition of diclofenac on LPS-induced PGE2 production in blood cells in vitro.
Conclusion:
Arthritis induced by FCA does not alter the pharmacokinetic behaviors of diclofenac in rats, but the pharmacodynamics of diclofenac is slightly affected. A PK-PD model characterizing an inhibitory effect sigmoid Imax can be used to fit the relationship between the plasma PGE2 and diclofenac levels in both normal rats and FCA-induced arthritic rats.
Similar content being viewed by others
Introduction
Diclofenac sodium is a non-steroidal anti-inflammatory drug (NSAID) that is widely prescribed and used for relieving the pain and edema associated with inflammatory conditions, such as osteoarthritis and rheumatoid arthritis1,2,3. It is commonly known that diclofenac acts by potent cyclo-oxygenase (COX) inhibition, which decreases the formation of proinflammatory mediators, such as prostaglandins (PGs)4. The prediction of safety and long-term efficacy has become the main challenge in the evaluation of NSAIDs for the treatment of pain in chronic inflammatory conditions. Pharmacokinetic-pharmacodynamic (PK-PD) modeling represents a powerful tool to quantitatively describe the pharmacokinetic, pharmacodynamic and system-related processes5. Several attempts have been made to illustrate the relationship between the plasma concentration-time profiles of NSAIDs and the pharmacological activity of these drugs using two types of traditional pharmacological endpoints: (i) those exploring the inflammatory response and having a mechanistic interest, such as central and local hyperthermia (body and skin temperature), hyperalgesia (pain score) and edema (paw volume) and (ii) the hybrid endpoints that have direct clinical relevance and reflect both the pain and functional impairments2,6,7,8,9,10,11. However, these studies have disregarded the direct relationship between the drug concentration and the pharmacological response to COX inhibition. In addition, the lack of direct correlation between the plasma drug concentrations and the analgesic or adverse effects in chronic inflammatory conditions has made it difficult to predict the appropriate dosing regimen for the treatment of chronic inflammatory pain12.
Prostaglandin E2 (PGE2) is associated with acute and chronic inflammatory pain, and NSAIDs exert analgesic effects via the inhibition of COX-2 activity. As a biomarker of COX activity, it is well known that PGE2 can reflect a downstream process on the causal pathway between target occupancy and analgesic response. This indicates that PGE2 can be used as a specific biomarker to explain and understand the variability in the therapeutic of these drugs12. Recently, efforts have been made to establish the relationship between biomarkers, pain measurement and safety13,14,15,16. However, information on the integrated pharmacokinetic-pharmacodynamic profiles of these drugs under normal and chronic inflammatory conditions is still limited.
The aim of this study was to characterize the PK-PD profiles of diclofenac in normal and Freund's complete adjuvant (FCA)-induced arthritic rats using PGE2 as a biomarker. The inhibitory effect of diclofenac on PGE2 release induced by lipopolysaccharide (LPS) was also measured in vitro in the blood cells of normal and FCA-induced arthritic rats.
Materials and methods
Chemicals
Diclofenac sodium and Bacillus Calmette Guerin (BCG) were purchased from the National Institute for the Control of Pharmaceutical and Biological Products (Beijing, China), pentobarbital and lipopolysaccharide (LPS) were purchased from Sigma Chemical Co (St Louis, MO, USA), and the ELISA kits for PGE2 were from Cayman Chemical Co (Ann Arbor, MI, USA). All other reagents were of analytical grade and were commercially available.
Animals
Male Sprague Dawley rats (110–120 g) were purchased from B&K Universal Group Ltd (Shanghai, China). The rats were maintained in air-conditioned animal quarters at a temperature of 22±2 °C with a relative humidity of 50%±10% and a 12-h light/dark cycle. The rats received a standard diet (laboratory rodent chow; Nanjing, China) and water ad libitum. The studies were approved by the Animal Ethics Committee of China Pharmaceutical University.
Induction of Freund's complete adjuvant (FCA)-induced arthritic rats
FCA-induced arthritic rats were developed according to a previously described method17. Rats were acclimated for 1 week before the experiments and randomly divided into two groups. Freund's complete adjuvant (FCA) was prepared by grinding 60 mg of heat-killed BCG in a mortar and adding a mixture of liquid paraffin and lanolin (2:1, v/v) so that the final concentration of BCG was 10 mg/mL. Rats received a single intradermal injection of 0.1 mL of FCA in the right hindpaw by inserting a 25-gauge, 0.5-inch needle between the second and third digits into the dorsum of the hind paw on d 018. For clinical evaluation of FCA-induced arthritis, the polyarthritis severity was graded on a scale of 0–419: 0, no swelling; 1, isolated phalanx joint involvement; 2, involvement of the phalanx joint and digits; 3, involvement of the entire region to the ankle; and 4, involvement of the entire paw including the ankle. Scores were given for the left hindpaw and both forepaws for each rat, yielding a maximum possible score of 12 on d 20 after treatment with adjuvant. The total score was defined as the secondary inflammation index (arthritic index). Body weight and food intake were monitored every day. A sensitized animal was considered to have arthritis when at least one non-injected paw was inflamed, and these rats were then used for the following experiments.
In vivo experiments
On d 20, after FCA injection, the FCA-induced arthritic rats and age-matched normal rats were fasted overnight and given a dose of diclofenac sodium intravenously (10 mg/kg) in the tail vein. Blood samples (approximately 200 μL) were collected under light ether anesthesia via the oculi chorioideae vein before dosing, as well as at 5, 15, 30, 60, 120, 180, 240, and 360 min after dosing. The blood sample taken prior to dosing was used for measuring the basal levels of PGE2. The plasma samples were obtained by centrifugation at 5000 rounds per minute for 10 min and stored at -80 °C for assaying diclofenac and PGE2 levels.
In vitro experiments in whole blood
For the in vitro experiments, the blood samples of FCA-induced arthritic rats and normal rats were collected under anesthesia via the abdominal aorta with intraperitoneal administration of pentobarbital (60 mg/kg). The PGE2 released by LPS in the blood samples was documented according to a previously described method20. A 200-μL blood sample was added to a tube containing different levels of diclofenac sodium, heparin (0.3%) and aspirin (10 μg/mL). After adding LPS (final levels 10 μg/mL), the blood samples were incubated for 24 h at 37 °C in a gently stirring water bath. The plasma was separated by centrifugation at 5000 rounds per minute for 10 min and was stored at -80 °C for assessing PGE2 levels.
HPLC analysis of diclofenac
The concentration of diclofenac in the plasma was analyzed by a validated HPLC procedure using ultraviolet (UV) detection that has been previously described21. Briefly, plasma samples were spiked with 10 μL of internal standard (50 μg/mL naproxen in methanol). Then, 200 μL acetonitrile was added, and the samples were vortex-mixed. After centrifugation at 15 000 rounds per minute for 10 min, the organic layer was transferred to a clean tube and evaporated to dryness under a stream of nitrogen gas in a water bath at 45 °C. The residue was reconstituted in 100 μL of mobile phase and centrifuged (1000 rounds per minute, 10 min). Next, 20 μL of the supernatant was injected into an HPLC system equipped with an LC-10AD pump, a CTO-10ASvp column oven, and a SPD-10A UV absorbance detector (Shimadzu, Kyoto, Japan) set to a wavelength at 276 nm. Chromatography was performed on a Diamonsil C18 5-μm column (150 mm×4.6 mm, Dikma, Technologies, Beijing, China). The mobile phase consisted of 0.03% phosphoric acid and acetonitrile (45:55, v/v) with a flow rate of 1.0 mL/min. The linear range of diclofenac in plasma was 0.078–10 μg/mL, and the limit of quantification for diclofenac was 0.078 μg/mL.
Analysis of PGE2
The PGE2 levels were measured with an enzyme immunoassay (EIA) using the Cayman EIA kits according to the manufacturer's protocol. Briefly, samples were diluted in EIA buffer, and a 50-μL aliquot was transferred into a coated well plate. After the addition of 50 μL of the corresponding antibody and 50 μL of acetylcholinesterase conjugate, samples were incubated at 4 °C for 18 h, washed five times and incubated for 60 min in an orbital shaker after 200 μL substrate was added. The absorbance was measured in a plate reader at 412 nm.
Pharmacokinetic-pharmacodynamic modeling
A combined pharmacokinetic and pharmacodynamic (PK-PD) model was used to describe the intensity of the effect as a function of time. This model was made on a computer running Windows XP with WinNonlin Professional software (Version 6.1, Pharsight Corporation, Mountain View, CA, USA).
The diclofenac concentration-time data for plasma were individually fitted using one-, two-, and three-compartment models. Goodness-of-fit was assessed by the objective functions and visual inspection of various diagnostic plots. Based on model selection criteria such as parameter correlations and Akaike Information Criterion (AIC), good fittings were observed using a two-compartmental model.
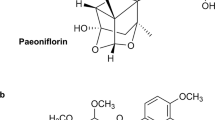
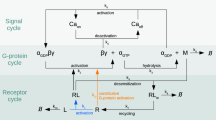
The obtained pharmacokinetic parameters were then used to characterize the relationship between diclofenac concentrations and PGE2 levels. Several models, including Imax and indirect response models, were tried to fit pharmacodynamic data (PGE2 levels), and the results showed that the sigmoid Imax model yielded the best fit. Therefore, a PK-PD model characterizing an inhibitory effect sigmoid Imax was introduced to illustrate the relationship between diclofenac concentrations and PGE2 levels in plasma, which is described in Figure 1.
The relationship between diclofenac concentrations (C) and the PGE2 levels (E) was expressed as follows.

where E0 is the basal level of PGE2, Imax represents the maximum inhibitory fraction to diclofenac, IC50 is the drug concentration required to produce 50% of the maximum inhibition and γ is a slope factor, which determines the steepness of the curve. The IC80 value was also estimated according to the equation described by Huntjens et al16.

Statistical analysis
The data were expressed as the mean±standard error (SEM) (CV%). The statistical analysis was performed using a t-test. Differences were considered significant when P<0.05.
Results
Development of FCA-induced arthritic rats
The development of the FCA-induced arthritic rats (Figure 2) was observed. The rats that were treated with FCA showed a decreased rate in body weight gain. The body weight of the arthritic rats (219.5±7.5 g) was significantly lower than that of normal rats (263.4±5.5 g, P<0.01) on d 20. The incidence of the arthritis was approximately 28%, which is agreement with a previous study22. The FCA-induced arthritic rats showed typical arthritic symptoms, including involvement of the phalanx joint and digits, involvement of the entire region to the ankle, or involvement of entire paw including the ankle. The arthritic index of the non-injected paws of the FCA-induced arthritic rats gradually rose with time. The arthritic index was 6.5±0.7 on d 20 after the FCA injection. Only FCA-induced arthritic rats were chosen for following experiments.
Pharmacokinetics of diclofenac in normal and FCA-induced arthritic rats
The plasma concentrations of diclofenac in normal and FCA-induced arthritic rats were measured following an iv (intravenously) injection of 10 mg/kg diclofenac (Figure 3). The plasma concentration-time data were fitted by a two-compartment model, and the corresponding pharmacokinetic parameters were estimated (Table 1). The results showed that arthritis induced by FCA did not alter the pharmacokinetic behaviors of diclofenac.
Pharmacodynamics of diclofenac in normal and FCA-induced arthritic rats
PGE2 served as a biomarker to represent the pharmacodynamic index of diclofenac in rats. The results showed that FCA-induced arthritic rats had higher basal levels of plasma PGE2 compared with those of normal rats, although no significance was found (Figure 4). The PGE2 level-time data were assayed (Figure 4A) following an iv injection of 10 mg/kg diclofenac. As expected, the administration of diclofenac significantly decreased the levels of PGE2 in the plasma of both normal and FCA-induced arthritic rats, although a large degree of variability was observed. The maximum inhibition occurred 5 min after dosing. No delay in the onset of inhibition was observed, revealing that the effect compartment was located in the central compartment. This result agrees with a previous report that described the use of naproxen14,23.
The relationship between PGE2 levels and diclofenac levels in the plasma were fitted by an inhibitory effect sigmoid Imax model, and the pharmacodynamic parameters were estimated (Table 2). The potency of diclofenac was expressed as IC50 and IC80 values. Compared with normal rats, higher IC50 and IC80 values for PGE2 production in FCA-induced arthritic rats suggested that the inhibitory effects of diclofenac on PGE2 production in FCA-induced arthritic rats were less profound than that in normal rats, although a higher Imax value was found. The observed and fitted data for PGE2 concentration (ng/mL) vs time (h) in vivo after iv (10 mg/kg) for normal (A) and FCA-induced rats (B) are shown in Figure 5.
Inhibition of PGE2 production by diclofenac in whole blood
The effect of diclofenac on PGE2 production induced by LPS in vitro in whole blood was also investigated (Figure 6). The basal levels of PGE2 induced by LPS in vitro in whole blood from normal and FCA-induced arthritic rats were measured to be 63.9±17.6 and 54.5±12.5 ng/mL, respectively. Diclofenac decreased PGE2 levels in a concentration-dependent manner. The data from PGE2-diclofenac levels in vitro in whole blood were also fitted using the inhibitory effect sigmoid Imax model (Table 2). The percent of maximum inhibition (Imax· 100%) by diclofenac in vitro in whole blood (85.8% in normal rats and 74.6% in FCA-induced arthritic rats) was less than the maximum inhibition (98%) found in vivo. The estimated IC50 value in vitro in the whole blood of normal rats was higher than that in vivo (1.3±0.7 μg/mL in vitro whole blood vs 0.5±0.2 μg/mL in vivo), but the estimated IC50 value in vitro in the whole blood of FCA-induced arthritic rats was less than that in vivo (0.4±0.2 μg/mL in vitro whole blood vs 0.7±0.3 μg/mL in vivo). The IC50 and IC80 values in vitro in the whole blood of FCA-induced arthritic rats were less than those in normal rats. The observed and fitted data for PGE2 concentration (μg/mL) vs diclofenac concentration (μg/mL) in vitro in the whole blood in normal (A) and FCA-induced rats (B) are shown in Figure 7.
Discussion
It has been established that PGE2 is released after inflammatory stimuli and the inhibition of PGE2 can largely account for the therapeutic effects of NSAIDs4. PGE2 levels are highly correlated with pain and inflammation, which indicates that PGE2 can serve as a biomarker to bridge an intermediate step between drug exposure and response. Due to the possibility of repeated measurements and increased reproducibility and sensitivity, PGE2 could be a suitable alternative endpoint for investigations and comparisons of the time-course and potency of various drug candidates23. Several reports have shown the integrated PK-PD modeling of NSAIDs using hyperthermia, hyperalgesia, edema or PGE2 as pharmacological endpoints5,11,23, but little attention has been paid to the impact of the disease status on drug effects16. The aim of this study was to characterize the PK-PD modeling of diclofenac in normal and FCA-induced arthritic rats using PGE2 as a pharmacological endpoint. Our results clearly demonstrate that arthritis induced by FCA does not alter the pharmacokinetic behaviors of diclofenac in rats. However, some reports have shown that acute inflammation may alter the pharmacokinetics of NSAIDs24,25. This discrepancy may come from the oscillations of activities of CYP enzymes over period of inflammation and drugs25. The levels of diclofenac and the corresponding biomarker PGE2 were measured after the administration of diclofenac. It was found that FCA-induced arthritic rats had higher basal levels of PGE2 in the plasma, although no significance was found because of large inter-individual variability. A large degree of inter-individual variability for PGE2 has also been shown in other reports16,26. Similarly, such variability is often observed in levels of other endogenous compounds27,28. It is generally accepted that cyclo-oxygenase-2 (COX-2) is responsible for PGE2 production, which indicates that the increased biomarker levels are due to COX-2 activity during inflammation12. Diclofenac significantly inhibited PGE2 production, and the maximum inhibition occurred 5 min after dosing. Then, the inhibitory effects gradually fell with the decline in diclofenac levels, which indicates that the inhibition of PGE2 by diclofenac is reversible. The relationship between PGE2 levels and diclofenac levels in plasma was successfully illustrated using an inhibitory effect sigmoid Imax model. Estimated IC50 and IC80 values for PGE2 production in FCA-induced arthritic rats were higher than those in normal rats.
The effect of diclofenac on PGE2 production induced by LPS in vitro in whole blood was investigated. In contrast to the in vivo results, the basal PGE2 levels induced by LPS in vitro in the whole blood of FCA-induced arthritic rats was lower than that in normal rats, which indicates that the sensitivity of the whole blood of the FCA-induced arthritic rats to LPS was less than that of the whole blood of the normal rats. In addition, the percent of maximum inhibition (Imax·100%) by diclofenac in vitro in whole blood was less than that in vivo. This discrepancy might have resulted from COX-1 inhibition. The in vitro whole blood experiment was performed in the presence of aspirin (10 μg/mL), which irreversibly inactivates platelet COX-1. It has been reported that rat blood might also produce copious amounts of PGE2 via the actions of the COX-1 enzyme that is constitutively present in platelets29. The inhibition of COX-1 by aspirin might explain the discrepancies between the in vivo studies and the in vitro whole blood studies for PGE2 inhibition.
In summary, these results support the conclusion that arthritis induced by FCA did not alter the pharmacokinetic behaviors of diclofenac in rats, but the pharmacodynamics of diclofenac were slightly affected. A pharmacokinetic-pharmacodynamic model characterizing an inhibitory effect sigmoid Imax was developed to illustrate the relationship between the plasma concentration of diclofenac and the inhibition of PGE2 production both in normal and FCA-induced arthritic rats.
Author contribution
Jing ZHANG and Xiao-dong LIU designed the experiments and analyzed the data; Jing ZHANG wrote the paper; Xiao-dong LIU and Li LIU revised the paper; Jing ZHANG, Pei LI, and Hai-fang GUO performed the research.
References
Burian M, Geisslinger G . COX-dependent mechanisms involved in the antinociceptive action of NSAIDs at central and peripheral sites. Pharmacol Ther 2005; 107: 139–54.
Vásquez-Bahena DA, Salazar-Morales UE, Ortiz MI, Castañeda-Hernández G, Trocóniz IF . Pharmacokinetic-pharmacodynamic modelling of the analgesic effects of lumiracoxib, a selective inhibitor of cyclooxygenase-2, in rats. Br J Pharmacol 2010; 159: 176–87.
Menasse R, Hedwell P, Kraetz J, Pericin C, Riesterer L, Sallman A, et al. Pharmacological properties of diclofenac sodium and its metabolites. Scand J Rheumatol 1978; 22: 5–16.
Vane JR . Inhibition of prostaglandin synthesis as a mechanism of action for aspirin-like drugs. Nat New Biol 1971; 231: 232–5.
Giraudel JM, Diquelou A, Laroute V, Lees P, Toutain PL . Pharmacokinetic pharmacodynamic modelling of NSAIDs in a model of reversible inflammation in the cat. Br J Pharmacol 2005; 146: 642–53.
Torres-Lopez JE, Lopez-Munoz FJ, Castaneda-Hernandez G, Flores-Murrieta FJ, Granados-Soto V . Pharmacokinetic-pharmacodynamic modelling of the antinociceptive effect of diclofenac in the rat. J Pharmacol Exp Ther 1997; 282: 685–90.
Granados-Soto V, Lopez-Munoz FJ, Hong E, Flores-Murrieta FJ . Relationship between pharmacokinetics and the analgesic effect of ketorolac in the rat. J Pharmacol Exp Ther 1995; 272: 352–6.
Josa M, Urizar JP, Rapado J, Dios-Vieitez C, Castaneda-Hernandez G, Flores-Murrieta F, et al. Pharmacokinetic pharmacodynamic modelling of antipyretic and anti-inflammatory effects of naproxen in the rat. J Pharmacol Exp Ther 2001; 297: 198–205.
Jeunesse EC, Bargues IA, Toutain CE, Lacroix MZ, Letellier IM, Giraudel JM, et al. Paw inflammation model in dogs for preclinical pharmacokinetic pharmacodynamic investigations of nonsteroidal anti-inflammatory drugs. J Pharmacol Exp Ther 2011; 338: 548–58.
Toutain PL, Cester CC, Haak T, Laroute V . A pharmacokinetic- pharmacodynamic approach vs a dose titration for the determination of a dosage regimen: the case of nimesulide, a COX-2 selective nonsteroidal anti-inflammatory drug in the dog. J Vet Pharmacol Ther 2001; 24: 43–55.
Flores-Murrieta FJ, Ko HC, Flores-Acevedo DM, López-Muñoz FJ, Jusko WJ, Sale ME, et al. Pharmacokinetic-pharmacodynamic modeling of tolmetin antinociceptive effect in the rat using an indirect response model: a population approach. J Pharmacokinet Biopharm 1998; 26: 547–57.
Huntjens DR, Danhof M, Della Pasqua OE . Pharmacokinetic-pharmacodynamic correlations and biomarkers in the development of COX-2 inhibitors. Rheumatology (Oxford) 2005; 44: 846–59.
Lepist EI, Jusko WJ . Modeling and allometric scaling of s(+)-ketoprofen pharmacokinetics and pharmacodynamics: a retrospective analysis. J Vet Pharmacol Ther 2004; 27: 211–8.
Huntjens DR, Spalding DJ, Danhof M, Della Pasqua OE . Correlation between in vitro and in vivo concentration effect relationships of naproxen in rats and healthy volunteers. Br J Pharmacol 2006; 148: 396–404.
Huntjens DR, Strougo A, Chain A, Metcalf A, Summerfield S, Spalding DJ, et al. Population pharmacokinetic modelling of the enterohepatic recirculation of diclofenac and rofecoxib in rats. Br J Pharmacol 2008; 153: 1072–84.
Huntjens DR, Spalding DJ, Danhof M, Della Pasqua OE . Impact of chronic inflammation on the pharmacokinetic pharmacodynamic relationship of naproxen. Eur J Pain 2010; 14: 227.e1–10.
Wei W, Chen MZ, Xu SY . Pharmacological effects of isoxicam. Chin Pharmacol Bull 1986; 2: 29–34.
Fletcher DS, Widmer WR, Luell S, Christen A, Orevillo C, Shah S, et al. Therapeutic administration of a selective inhibitor of nitric oxide synthase does not ameliorate the chronic inflammation and tissue damage associated with adjuvant-induced arthritis in rats. J Pharmacol Exp Ther 1998; 284: 714–21.
Gu WZ, Brandwein SR . Inhibition of type II collagen-induced arthritis in rats by triptolide. Int J Immunopharmacol 1998; 20: 389–400.
Blain H, Boileau C, Lapicque F, Nédélec E, Loeuille D, Guillaume C, et al. Limitation of the in vitro whole blood assay for predicting the COX selectivity of NSAIDs in clinical use. Br J Clin Pharmacol 2002; 53: 255–65.
Wang DL, Liu L, Deng YX, Liu HY, Xie L, Liu XD, et al. Effects of ginkgolide B on the pharmacokinetics and pharmacodynamics of diclofenac, a substrate of cytochrome P450 2C9, in rats. Chin New Drug J 2008; 17: 919–26.
Banik RK, Kasai M, Mizumura K . Reexamination of the difference in susceptibility to adjuvant-induced arthritis among LEW/Crj, Slc/Wistar/ST and Slc/SD rats. Exp Anim 2002; 51: 197–201.
Krekels EH, Angesjö M, Sjögren I, Möller KA, Berge OG, Visser SA . Pharmacokinetic-pharmacodynamic modeling of the inhibitory effects of naproxen on the time-courses of inflammatory pain, fever, and the ex vivo synthesis of TXB2 and PGE2 in rats. Pharm Res 2011; 28: 1561–76.
Projean D, Dautrey S, Vu HK, Groblewski T, Brazier JL, Ducharme J . Selective downregulation of hepatic cytochrome P450 expression and activity in a rat model of inflammatory pain. Pharm Res 2005; 22: 62–70.
Uno S, Fujii A, Komura H, Kawase A, Iwaki M . Prediction of metabolic clearance of diclofenac in adjuvant-induced arthritis rats using a substrate depletion assay. Xenobiotica 2008; 38: 482–95.
Patrignani P, Panara MR, Sciulli MG, Santini G, Renda G, Patrono C . Differential inhibition of human prostaglandin endoperoxide synthase-1 and -2 by nonsteroidal anti-inflammatory drugs. J Physiol Pharmacol 1997; 48: 623–31.
Gozzi P, Påhlman, I, Palmér, L, Grönberg A, Persson S . Pharmacokinetic-pharmacodynamic modeling of the immunomodulating agent susalimod and experimentally induced tumor necrosis factor-α levels in the mouse. J Pharmacol Exp Ther 1999; 291: 199–203.
Geldof M, Freijer JI, Peletier LA, van Beijsterveldt L, Danhof M . Mechanistic model for the acute effect of fluvoxamine on 5-HT and 5-HIAA concentrations in rat frontal cortex. Eur J Pharm Sci 2008; 33: 217–29.
Giuliano F, Warner TD . Origins of prostaglandin E2: involvements of cyclooxygenase (COX)-1 and COX-2 in human and rat systems. J Pharmacol Exp Ther 2002; 303: 1001–6.
Acknowledgements
This work was supported by funds from the Graduate Student Research and Innovation Program of Jiangsu Province (Grants No CX10B-383Z, 2010) and by funding for innovative research team in institution of Jiangsu higher education.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, J., Li, P., Guo, Hf. et al. Pharmacokinetic-pharmacodynamic modeling of diclofenac in normal and Freund's complete adjuvant-induced arthritic rats. Acta Pharmacol Sin 33, 1372–1378 (2012). https://doi.org/10.1038/aps.2012.67
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2012.67
Keywords
This article is cited by
-
Ciprofloxacin blocked enterohepatic circulation of diclofenac and alleviated NSAID-induced enteropathy in rats partly by inhibiting intestinal β-glucuronidase activity
Acta Pharmacologica Sinica (2016)
-
Pharmacometrics: a quantitative tool of pharmacological research
Acta Pharmacologica Sinica (2012)