Abstract
Aim:
To evaluate the pharmacokinetics of tacrolimus in Chinese stable liver transplant recipients converted from immediate release (IR) tacrolimus-based immunosuppression to modified release (MR) tacrolimus-based immunosuppression.
Methods:
Open-label, multi-center study with a one-way conversion design was conducted. Eighty-three stable liver recipients (6–24 months post-transplant) with normal renal and stable hepatic function were converted from IR tacrolimus twice-daily treatment to MR tacrolimus once-daily treatment on a 1:1 (mg: mg) total daily dose basis. Twenty-four hour pharmacokinetic studies were carried out on d 0 (pre-conversion), d 1, and d 84 (post-conversion).
Results:
The area under the blood concentration–time curve of MR tacrolimus from 0 to 24 h (AUC0–24) on d 1 was comparable to that of IR tacrolimus on d 0, with a 90% confidence interval (CI) for MR/IR tacrolimus of 92%–97%. The AUC0–24 value for MR tacrolimus on d 84 with the daily dose increased by 14% was approximately 17% lower than that for IR tacrolimus. The 90% CI was 77%–90%, outside the bioequivalence range of 80%–125%. There was a good correlation between AUC0–24 and concentration at 24 h (C24) for IR tacrolimus (d 0, r=0.930) and MR tacrolimus (d 1, r=0.936; d 84, r=0.903).
Conclusion:
The exposure to tacrolimus when administered MR tacrolimus once daily is not equivalent to that for IR tacrolimus twice daily after an 84-day conversion in Chinese stable liver transplant recipients. The dose should be adjusted on the basis of trough levels. The therapeutic drug monitoring for patients treated with IR tacrolimus is considered to be applicable to MR tacrolimus.
Similar content being viewed by others
Introduction
Tacrolimus is an immunosuppressive agent that inhibits cellular and T-cell-dependent humoral responses via the inactivation of the intracellular calcineurin complex. It has been marketed mainly for preventing or treating graft rejection in solid organ transplantation1, 2. Tacrolimus has a narrow therapeutic window, and its bioavailability shows high inter- and intra-individual variability1, 3, 4. The systemic exposure AUC is a significant efficacy variable; therefore, therapy is optimized on an individual patient basis by monitoring trough levels as surrogate markers of exposure. In clinical practice, the current immediate release (IR) tacrolimus is administered twice a day, once in the morning and once in the evening, to maintain whole blood trough concentrations generally within the range of 5–15 μg/L to prevent rejection. Tacrolimus should be taken 1 h before or at least 2 to 3 h after a meal to prevent a food effect. This schedule may be an additional burden for the patient, especially for the evening dose, because it may interfere with daily activities. Transplant recipients often receive an immunosuppressive regimen consisting of multiple medications; thus, a formulation that can be taken once daily is considered to be beneficial to patients. A new oral modified release (MR) formulation of tacrolimus has been developed to allow a once-daily dosing regimen. Clinical studies demonstrate that MR tacrolimus is as efficient and safe as IR tacrolimus5, 6, 7, 8. This formulation, known commercially as Advagraf, has been approved in more than 30 countries and regions as of 2010. The pharmacokinetics (PK) of tacrolimus have been compared between MR and IR formulations in stable kidney, liver, and heart transplant patients, and in de novo kidney and liver transplant recipients9, 10, 11, 12, 13. However, there is few clinical data on Chinese patients. The present study was designed to evaluate the PK profiles of tacrolimus in Chinese stable liver transplant recipients converted from a twice-daily IR tacrolimus-based immunosuppression regimen to a once-daily MR tacrolimus-based immunosuppression regimen.
Materials and methods
Patients
Eligible patients were stable liver transplant recipients who had undergone a transplant operation between 6 and 24 months prior to the start of the study. They were on a stable dose of IR tacrolimus (with or without mycophenolate mofetil) that remained unchanged for two weeks before baseline and a stable blood trough level concentration of tacrolimus (2–10 μg/L) which was measured before enrollment. Additional inclusion criteria were age (18–67 years), normal renal function (serum creatinine in the normal range), and stable liver function (aspartate aminotransferase or alanine aminotransferase less than twice the normal value). Patients who had received other organ transplantation, experienced any rejection episode within 90 days of enrollment, received antibody therapy within 6 months of enrollment, or were currently receiving other immunosuppression therapy such as sirolimus were not enrolled. Patients who had taken any drug that may interact with tacrolimus within 28 days of the study or during the study were also excluded.
Ethics
The clinical study was conducted at six study sites, with the leadership of Peking University People's Hospital, following approval of the protocol by the Independent Ethics Committee of the leadership hospital. The study was in full compliance with the principles of the “Declaration of Helsinki” (current revision) and the “Good Clinical Practice” guidelines issued by the State of Food and Drug Administration in China. Written informed consent was obtained from each patient before enrollment.
Study design
The research was an open-label, multi-center, one-way conversion study in stable liver transplant recipients being treated with IR tacrolimus-based [Prograf®, Astellas Pharmaceutical (China), Inc] immunosuppression. On d 0, patients continued to receive a stable twice-daily dose of IR tacrolimus. On d 1, patients were converted to MR tacrolimus [Astellas Pharmaceutical (China), Inc] on a 1:1 (mg:mg) basis for their total daily dose. The administration time was similar to that of those who were administered IR tacrolimus for the first time. Succeeding doses were adjusted based on whole blood trough levels, which were expected to be 2–10 μg/L and were monitored using the microparticle enzyme immunosorbent assay (MEIA) or enzyme linked immunosorbant assay (ELISA) method.
PK studies
PK study 1 (PK1), PK study 2 (PK2), and PK study 3 (PK3), were carried out three times in 24 h on d 0, d 1, and d 84 (time window ±5 d).
Sample collection for the PK studies
In PK1, blood samples (2 mL) were collected from the forearm vein and placed into EDTA plastic tubes prepared in the morning at pre-dose and at 0.5 h, 1 h, 2 h, 3 h, 4 h, 6 h, 8 h, 12 h, 12.5 h, 13 h, 14 h, 15 h, 16 h, 18 h, 20 h, and 24 h after oral administration. In PK2 and PK3, blood samples were collected in the morning at pre-dose and at 0.5 h, 1 h, 2 h, 3 h, 4 h, 6 h, 8 h, 12 h, 14 h, 16 h, 20 h, and 24 h after oral administration. Blood samples were frozen at −20 °C within 20 min of collection. The frozen samples were then sent to the analytical laboratory and stored at −70 °C until analysis.
Determination of tacrolimus in human blood samples
The quantification of tacrolimus was performed using a validated liquid chromatography-tandem mass spectrometry (LC/MS/MS) method14. In brief, the blood samples were prepared using liquid-liquid extraction with ethyl ether. Chromatography was carried out on a Capcell-Pak CN column (particle size 5 μm, 100 mm×4.6 mm, Shiseido, Tokyo, Japan) using a mobile phase of acetonitrile-0.002% ammonia water (75:25, v/v) at a flow rate of 0.5 mL/min. Column temperature was maintained at 30 °C. An API 4000 triple quadrupole mass spectrometer equipped with a TurboIonSpray (ESI) source (Applied Biosystems, Concord, Ontario, Canada) was used for mass analysis and detection. Quantification was performed using multiple reaction monitoring (MRM) of the transitions m/z 802.7 → m/z 560.5 for tacrolimus and m/z 790.9 → m/z 548.5 for the internal standard ascomycin.
Tacrolimus response was found to be linear (r>0.998) over the concentration range of 0.200–30.0 μg/L. Intra- and inter-run precision values for the concentrations of 0.500, 4.00, and 24.0 μg/L were all less than 14.0%, and the accuracy ranged from 96.2% to 102.5% of the nominal value.
Data analysis
PK parameters were calculated using standard non-compartmental methods. Maximum concentration (Cmax) and time to reach Cmax (tmax) were determined by inspecting blood concentration–time curves. Concentration at trough level was determined using the concentration at 24 h (C24) on days when PK profiles were obtained. The area under the blood concentration–time curve from 0 to 24 (AUC0–24) at steady state was calculated using the linear trapezoidal method.
Statistical analysis
The correlation between AUC0–24 and C24 was analyzed for both MR and IR tacrolimus. As this was not a standard bioequivalence study, the comparisons of PK parameters between the two formulations were conducted with an analogous bioequivalence procedure based on a 90% CI for the ratio of geometric means and acceptance intervals of 80% to 125% for AUC0–24, Cmax, C24, and dose-adjusted AUC0–24. The parameters were ln-transformed before statistical analysis.
The software WinNonlin 5.2.1 (Pharsight, Mountain View, CA, USA) was used in PK analysis, and SAS 9.1.3 (SAS Institute Inc, Cary, NC, USA) was used for statistical analysis.
Results
Patients and dose levels
A total of 85 Chinese patients were enrolled in this PK study. Eighty-three patients (70 males and 13 females) completed PK1 and PK2 profiles; among them, 81 patients (68 males and 13 females) completed all three PK profiles. The mean age for the 83 patients was 46±10 years (from 19 to 67 years), and the mean weight was 66.1±11.4 kg (from 43 to 90 kg).
The mean daily dose of tacrolimus for IR tacrolimus on d 0 and MR tacrolimus on d 1 was 0.063±0.030 mg/kg (from 0.011 to 0.147 mg/kg), whereas the mean daily dose for MR tacrolimus on d 84 was 0.072±0.035 mg/kg (from 0.014 to 0.196 mg/kg). After conversion, 29 patients did not require any dose adjustment; 39 patients had an increase in daily doses; and 15 patients had a decrease.
Pharmacokinetics
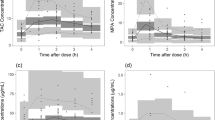
The mean whole blood concentration–time curves of tacrolimus for IR tacrolimus on d 0, MR tacrolimus on d 1, and MR tacrolimus on d 84 are shown in Figure 1. The calculated PK parameters are listed in Table 1, and the statistical results are summarized in Table 2.
The whole blood tacrolimus concentrations for IR tacrolimus reflected the twice-daily dose regimen, with a smaller secondary peak exhibited on d 0. There was another trough concentration at 12 h in addition to C24. The mean values of C12 and C24 were 4.15 and 4.26 μg/L, respectively. The mean Cmax was 11.3 μg/L at 1 h, with a secondary Cmax of 8.0 μg/L at 14 h.
The whole blood tacrolimus concentrations for MR tacrolimus reflected the profile of the MR formulation. The mean values of C24 for MR tacrolimus were considerably lower than that for IR tacrolimus, with 3.72 μg/L on d 1 and 3.31 μg/L on d 84. The mean Cmax was 10.4 μg/L at 2 h on d 1 and 9.0 μg/L at 2 h on d 84, which were also lower than those of IR tacrolimus.
The AUC0–24 for MR tacrolimus on d 1 was comparable to that for IR tacrolimus. The 90% CI for the ratio of geometric mean was 92%–97%, which was contained entirely in the 80%–125% limits of equivalence. However, the same parameter for MR tacrolimus on d 84 was approximately 17% lower than that for IR tacrolimus, with a 90% CI of 77%–90%. The 90% CI for dose-adjusted AUC0–24 was 66%–79%, which was also not within the equivalence limits of 80%–125%.
Correlation between AUC0–24 and C24
The correlation between AUC0–24 and C24 for IR tacrolimus and MR tacrolimus is shown in Figure 2. There was a good correlation between AUC0–24 and C24, with a coefficient r of 0.930 for IR tacrolimus on d 0, 0.936 for MR tacrolimus on d 1, and 0.903 for MR tacrolimus on d 84. The correlation between AUC0–24 and C24 for MR tacrolimus was similar to that for IR tacrolimus.
Discussion
Before our study, a set of clinical trials had been conducted to compare the PK profiles of tacrolimus between IR and MR formulations9, 10, 11, 12, 13. The clinical trial in de novo liver transplant patients showed that the systemic exposure AUC0-24 on d 1 was approximately 50% lower for MR tacrolimus than for IR tacrolimus at equivalent doses, whereas values at steady state (d 14 and w 6) were similar for both formulations13. The conversion study in stable liver transplant patients showed that the AUC0-24 at steady state for MR tacrolimus once daily was equivalent to taking IR tacrolimus twice a day, but on average an 11% lower AUC0-24 was found after a mg-for-mg dose conversion9. In order to better understand the PK profiles of MR tacrolimus, we performed a conversion study with a long period follow up in Chinese stable liver transplant recipients. In this study, the systemic exposure to MR tacrolimus on the first conversion day was found to be equivalent to that for IR tacrolimus. This is not surprising because the exposure on d 1 reflects mostly the steady state exposure for the IR formulation. However, the steady state exposure of MR tacrolimus was found to decrease significantly when compared with that of IR tacrolimus. The AUC0-24 value on d 84 decreased by 17% when the daily dose increased by 14%. The 90% CI for the ratio of MR/IR tacrolimus was 77%–90%, and the 90% CI for the ratio in dose-adjusted AUC0-24 was only 66%–79%. These statistics are not in agreement with the previous report9, which showed that most patients did not require a dose adjustment when they were converted from IR to MR tacrolimus, and the 90% CI for the ratio in AUC0–24 was within the equivalence range of 80%–125%. The discrepancy between these results and our findings may be due to the difference in study design. The reported study9 was a four-period replicate (IR tacrolimus-MR tacrolimus-IR tacrolimus-MR tacrolimus) design study in which treatment with tacrolimus was converted on three occasions, and each treatment period was only 14 d. However, the present study was a one-way conversion from twice-daily IR tacrolimus to once-daily MR tacrolimus, and it had a longer period at nearly three months of treatment. In another one-way conversion study with a six months follow up, 68% of patients who converted to MR tacrolimus had doses adjusted and nearly two-thirds required an increase, which is similar to our findings15. Dose increases were also found in kidney and heart transplant recipients16, 17. The reason for the lower exposure for MR tacrolimus on d 84 is still unclear. It is well known that many factors influence the PK profiles of tacrolimus1. In this study, the patients were all in stable condition, and any drug known to alter the CYP450 enzyme system was prohibited before and during the study period to avoid drug-drug interaction. Because the treatment period was relatively long, some other factors that we did not find or record may have led to the decrease in exposure. Nevertheless, our findings, together with the latest reports15, 16, 17, indicate that for MR tacrolimus, exposure to tacrolimus will decrease somewhat, and patients may require a mild dose increase when they are converted from IR to MR tacrolimus.
Despite the lower exposure to tacrolimus for MR tacrolimus, the efficacy and safety of MR tacrolimus did not appear to be different from IR tacrolimus. Simultaneous clinical trials showed that there was no increase in incidences of acute rejection, graft loss, and effects on patient survival rates in patients converted to MR tacrolimus when compared with patients treated with IR tacrolimus18. The incidences of adverse events were also comparable in both treatment groups18. These observations indicate that MR and IR tacrolimus are therapeutically equivalent in stable liver transplant recipients.
Similar to other reports9, 10, 11, 12, 13, the present study also showed that there was a good correlation between AUC0–24 and C24 for both IR and MR tacrolimus. The fact that the slope of the line best fit was similar for both formulations indicates that the same therapeutic drug monitoring for IR tacrolimus could be applied to MR tacrolimus.
In conclusion, this study indicates that exposure to tacrolimus for MR tacrolimus once daily is not equivalent to that for IR tacrolimus twice daily in Chinese stable liver transplant recipients after an 84-day conversion, and the dose should be adjusted on the basis of trough levels. The therapeutic drug monitoring carried out for patients receiving IR tacrolimus is considered to be applicable to those receiving MR tacrolimus.
Author contribution
Da-fang ZHONG and Yi-fan ZHANG designed research; Xiaoyan CHEN, Xiao-jian DAI, and Xi-sheng LENG performed research; Yi-fan ZHANG analyzed data; Yi-fan ZHANG wrote the paper.
References
Staatz CE, Tett SE . Clinical pharmacokinetics and pharmacodynamics of tacrolimus in solid organ transplantation. Clin Pharmacokinet 2004; 43: 623–53.
Gewirtz AT, Sitaraman SV . Tacrolimus Fujisawa. Curr Opin Investig Drugs 2002; 3: 1307–11.
Scott L, McKeage K, Keam SJ, Plosker GL . Tacrolimus: a further update of its use in the management of organ transplantation. Drugs 2003; 63: 1247–97.
Wallemacq P, Armstrong VW, Brunet M, Haufroid V, Holt DW, Johnston A, et al. Opportunities to optimize tacrolimus therapy in solid organ transplantation: report of the European consensus conference. Ther Drug Monit 2009; 31: 139–52.
First MR, Fitzsimmons WE . Modified release tacrolimus. Yonsei Med J 2004; 45: 1127–31.
Wente MN, Sauer P, Mehrabi A, Weitz J, Büchler MW, Schmidt J, et al. Review of the clinical experience with a modified release form of tacrolimus [FK506E (MR4)] in transplantation. Clin Transplant 2006; 20 Suppl 17: 80–4.
Chisholm MA, Middleton MD . Modified-release tacrolimus. Ann Pharmacother 2006; 40: 270–5.
First MR . First clinical experience with the new once-daily formulation of tacrolimus. Ther Drug Monit 2008; 30: 159–66.
Florman S, Alloway R, Kalayoglu M, Lake K, Bak T, Klain A, et al. Conversion of stable liver transplant recipients from a twice-daily Prograf-based regimen to a once-daily modified release tacrolimus-based regimen. Transplant Proc 2005; 37: 1211–3.
Alloway R, Steinberg S, Khalil K, Gourishankar S, Miller J, Norman D, et al. Conversion of stable kidney transplant recipients from a twice-daily Prograf-based regimen to a once-daily modified release tacrolimus-based regimen. Transplant Proc 2005; 37: 867–70.
Alloway R, Vanhaecke J, Yonan N, White M, Haddad H, Rábago G et al. Pharmacokinetics in stable heart transplant recipients after conversion from twice-daily to once-daily tacrolimus formulations. J Heart Lung Transplant Epub 2011; 30: 1003–10.
Wlodarczyk Z, Squifflet JP, Ostrowski M, Rigotti P, Stefoni S, Citterio F, et al. Pharmacokinetics for once- versus twice-daily tacrolimus formulations in de novo kidney transplantation: a randomized, open-label trial. Am J Transplant 2009; 9: 2505–13.
Fischer L, Trunecka P, Gridelli B, Roy A, Vitale A, Vajdivieso A, et al. Pharmacokinetics for once-daily versus twice-daily tacrolimus formulations in de novo liver transplantation: a randomized, open label trial. Liver Transplantation 2011; 17: 167–77.
Zhang YF, Chen XY, Dai XJ, Ao JH, Zhong DF . Comparison of pharmacokinetics of tacrolimus in Chinese de novo kidney transplant patients after repeated-dose of modified release tacrolimus and immediate release tacrolimus. Chin J Clin Pharmacol 2011; 27: In press. Chinese.
Merli M, Di Menna S, Giusto M, Giannelli V, Lucidi C, Loria S, et al. Conversion from twice-daily to once-daily tacrolimus administration in liver transplant patient. Transplant Proc 2010; 42: 1322–4.
Hougardy JM, Broeders N, Kianda M, Massart A, Madhoun P, Le Moine A, et al. Conversion from Prograf to Advagraf among kidney transplant recipients results in sustained decrease in tacrolimus exposure. Transplantation 2011; 91: 566–9.
Marzoa-Rivas R, Paniagua-Martín MJ, Barge-Caballero E, Pedrosa del Moral V, Barge-Caballero G, Grille-Cancela Z, et al. Conversion of heart transplant patients from standard to sustained-release tacrolimus requires a dosage increase. Transplant Proc 2010; 42: 2994–6.
Li GM, Zheng SS, Liu YF, Zhu ZJ, Xia Q, Zhou J, et al. A randomized trial on the efficacy and safety of Advagraf vs tacrolimus in prevention of acute liver allograft rejection. Chin J Organ Transplant 2011; 32: 217–20.
Acknowledgements
We would like to acknowledge Prof Shu-sen ZHENG of the First Affiliated Hospital, Zhejiang University; Prof Yong-feng LIU of the First Hospital of China Medical University; Prof Zhi-jun ZHU of Tianjin First Center Hospital; Prof Qiang XIA of Renji Hospital affiliated to Shanghai Jiao Tong University; Prof Jia FAN of Zhongshan Hospital Fudan University; and Prof Zhi-ren FU of Shanghai Changzheng Hospital for their assistance in performing the clinical studies.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, Yf., Chen, Xy., Dai, Xj. et al. Pharmacokinetics of tacrolimus converted from twice-daily formulation to once-daily formulation in Chinese stable liver transplant recipients. Acta Pharmacol Sin 32, 1419–1423 (2011). https://doi.org/10.1038/aps.2011.125
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2011.125
Keywords
This article is cited by
-
Clinical Pharmacokinetics of Once-Daily Tacrolimus in Solid-Organ Transplant Patients
Clinical Pharmacokinetics (2015)