Abstract
Aim:
To investigate whether a combination of conventional and metronomic scheduling of chemotherapy could enhance and extend the effectiveness of chemotherapy against osteosarcoma.
Methods:
A total of 110 osteosarcoma-bearing SD rats were randomly divided into four groups, three of which were given conventional, metronomic or combination scheduling of chemotherapy, and the remaining one served as a control. Tumor volumes were measured every week during the treatment period of 8 weeks. At the end of treatment, tumors were removed from the rats and weighed. Expression of VEGFA in tumors was determined using Western blot assays.
Results:
As indicated by the tumor volume, conventional and metronomic schedules showed similar trends in tumor growth curves, and both of them lost their inhibitory effect in the sixth week, whereas the combination schedule maintained effectiveness until the end of treatment. Statistical significance with tumor volumes and weights was found among the groups (P<0.001), with combination scheduling being the most effective (P<0.001). Western blot indicated that all the therapy groups had significantly decreased expression of VEGFA (P<0.01), and the combination scheduling group had the lowest VEGFA expression.
Conclusion:
Combination of conventional and metronomic scheduling of chemotherapy could be a promising treatment for osteosarcoma. Antiangiogenesis contributed to the effect of combination scheduling.
Similar content being viewed by others
Introduction
Osteosarcoma, the most common malignant bone tumor in childhood and adolescence, is found predominantly found in males (male: female=1.6:1)1, 2. Despite its relatively low incidence rate among overall cancers, osteosarcoma is the second only less than leukemia causing cancer-related deaths in teenagers and children younger than ten years old3. Additionally, osteosarcoma progresses aggressively and usually develops a lung metastasis even after surgery. In spite of the continuous development of adjuvant therapies and increasing 5-year disease-free survival rate4, 5, 6, amputation is the primary treatment in most cases. Osteosarcoma results in lifelong physical disability and psychological trauma for patients and their families.
Until the late 1970s, limb amputation was the conventional treatment for osteosarcoma, associated with an extremely low 5-year disease-free survival rate of 10%–20%1. Subsequently, with the aim of eliminating primary tumor cells and micrometastases, neoadjuvant chemotherapy was introduced7. Doxorubicin (DOX), methotrexate (MTX), cisplatin (CDP) and ifosfamide (IFO) given in succession were proven effective for the treatment of osteosarcoma8, 9, 10, which made it possible to develop a systemic multi-agent chemotherapy. It was later proven to dramatically increase the overall or 5-year disease-free survival rate to 70% in the patients without metastasis6, 11. However, it still troubled researchers that standard neoadjuvant chemotherapy affected few patients with metastasis or who had had no response to prior chemotherapy. Despite the application of high-dose ifosfamide, novel problems arose as a result of the toxicity of the chemotherapy agents, such as bone marrow suppression, heart failure and serious liver and kidney damage6.
Studies in the past decade have indicated that several traditional chemotherapy agents have remarkable antiangiogenesis and inhibitory effects on tumor cell growth when administered with a higher frequency and at a lower dose12, 13, 14. This strategy was named the antiangiogenic schedule, also known as the metronomic schedule12, 15. As a nutrient transport channel, microvasculature provides a material basis for tumor growth and metastasis. However, in osteosarcoma, a hypervascular tumor, metronomic therapy is rarely used, despite evidence that it delays tumor recurrence in dogs with soft tissue sarcoma16 and has been proven effective in other cancers. In the current study, we hypothesized that the combination of conventional and metronomic scheduling of neoadjuvant chemotherapy would enhance inhibition of osteosarcoma cell growth. For this investigation, osteosarcoma-bearing SD rats were separated into four groups and received different schedules of chemotherapy treatment, including conventional, metronomic and combination chemotherapy, together with a null control group. The volume and weight of tumors were measured after the termination of treatment. Western blot assay was used to measure the expression level of VEGFA in tumor tissues, which is a signal that promotes the growth of new blood vessels.
Materials and methods
Cell culture and reagents
The osteosarcoma cell line UMR 106 was purchased from the Fourth Military Medical University in Xi'an, China and cultured in RPMI-1640 medium (Gibco, Grandland, NY) supplemented with 10% fetal bovine serum (FBS, Gibco). Lentiviral vectors with GFP-gene were transferred into UMR106 cells to establish a stable fluorescent cell line, UMR 106-GFP. The 293FT cell line (Invitrogen, Carlsbad, CA) was cultured in Dulbecco's modified Eagle medium (DMEM, Gibco) supplemented with 10% FBS. All the cell cultures were maintained in an incubator with 5% CO2 at 37 °C. Methotrexate (MTX), adriamycin (ADM), and Cilatinum (CDP) were commercially obtained.
Osteosarcoma-bearing SD rat modeling
Both 4- to 6-week-old Balb/c nude mice and 5-week-old SD rats were obtained from the Animal Center of Shanghai Public Health Center. Before UMR 106-GFP was injected into SD rats, it was cultured in Balb/c nude mice for several generations to enhance its tumorigenicity. Initially, 5×106 cells were inoculated under the right forelimb axillary of three Balb/c nude mice. Once at a volume of 0.8 cm3, the tumors were peeled off, their capsules and external blood vessels were cleaned, and they were shredded into 0.2 mm3 tumor tissue grains. Twenty to thirty pieces of the grains were inoculated again in the subcutaneous tissue of three more nude mice to culture the next generation. Seven in vivo periods were carried out before the last generation of tumor grains was inoculated subcutaneously to the forelimb axillary of SD rats. In each period, one of the three nude mice was kept alive until 21 d after incubation to observe the tumorigenicity by measuring the volume of the tumor.
Forty to sixty pieces of 0.2 mm3 tumor grains were used for each SD rat.
Chemotherapy of the osteosarcoma-bearing SD rats
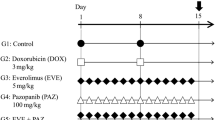
A total of 110 osteosarcoma-bearing SD rats were divided into four groups.
The 10 rats in the control group received no chemotherapy. However, the volumes of control rat tumors were measured every three days and then calculated using the formula (width×length2)/2.
Thirty rats received conventional neoadjuvant chemotherapy; the medication process is described in Table 1. Intravenous drip MTX was used with a high dosage of 1.35 g/kg for 6 h, followed by detoxification with folinic acid (CF).
Another thirty rats received tail vein injections of MTX on a metronomic schedule of twice a week with a lower dosage of 1.2 mg/kg.
Forty rats received combination chemotherapy with conventional and metronomic scheduling of chemotherapy. For these animals, MTX was used twice a week in the third, fourth, eighth weeks of conventional scheduling with a lower dosage of 1.2 mg/kg (Table 1).
At the termination of the treatment, all the SD rats were killed and the tumors were removed to be measured and weighed.
Western blot assay
Tumor tissues were frozen and sliced into 10-μm sections and lysed in PBS at 4 °C for 30 min, with 1% NP-40 and protease inhibitor cocktail tablets (Roche, Mannheim, Germany). BCA assay (Pierce, Rockford, IL) was used to determine the concentration of protein. After being separated by electrophoresis, proteins were transferred from the gel to a polyvinylidene difluoride (PVDF) membrane and then stained with ponceau S for 2 min. After being washed with TBST three times, the membrane was incubated with rabbit polyclonal antibody against rat VEGF-A (Abcam, Cambridge, UK) at 4 °C for 4 h, followed by another three washes of TBST. Next, membrane was incubated with peroxidase-conjugated goat anti-rabbit immunoglobulin G (Pierce) for 1 h at room temperature. After another wash with TBST, the membrane was visualized with enhanced DAB (Biyuntian, Shanghai, China) staining. β-actin in the same individual samples was analyzed with rat anti-β-actin mAb (Zhongshan Goldenbridge Biotechnology Co Ltd, Beijing, China) to calibrate the volume of the samples. Western blot lanes were analyzed by Gel-Pro analyzer.
Statistical analysis
Statistical evaluation of differences in the tumor volume and weight among groups was determined by Dunnett's T3 test after the homogeneity of variance was assessed by Levene's test. Ratios between each treated group and control group were calculated to evaluate the efficacy of each treatment. All of the data analysis was performed using SPSS 13.0
Results
Tumor growth in Bal b/c nude mice
In the first period of UMR 106-GFP culture in each nude mouse, a vacuole caused by the cell suspension could be seen at the inoculation site on the day of inoculation. One day later, the suspension disappeared, and the skin recovered its smoothness. A lump could be observed at the inoculation site a week after inoculation. Fourteen days after inoculation, there was a grain-sized tumor at the site that kept growing until four weeks after inoculation. Afterward, each mouse lost weight, and the growth rate of the tumors slowed. As the in vivo culture periods continued, the growth of the tumors accelerated.
Enhancement of tumorigenicity after several culture generations in nude mice
UMR 106-GFP cells were generated in Bal b/c nude mice for several cycles. At the end of each generation, one nude mouse was kept alive until 21 d after inoculation. Afterward, tumor tissues were removed from the dead mice to measure the volume and weight. After comparison of the seven mice from the seven different generations, we found that along with the process of generation, UMR 106-GFP accelerated proliferation and tumorigenicity was enhanced (Figure 1).
Tumorigenicity enhancement by repeated in vivo generation in Balb/c nude mice. (A) Twenty-one days after UMR 106 cells incubation, the volume of tumor was about 0.5 cm3 after 2 in vivo culture periods; (B) The volume of tumor was about 2 cm3 after 4 in vivo periods; (C) The volume of tumor was about 4.5 cm3 after 7 in vivo periods.
Inhibitory effect of the chemotherapy on tumor growth of SD rats
In all the treatment groups as well as the control group, the tumor volume increased continuously throughout the experiment (Figure 2). Statistical analysis indicated that growth rate of tumor in all four groups was significantly different. Further multiple comparisons were performed.
Mean tumor volumes and tumor inhibition rate. (A) The volumes were calculated by: Volume (mm3)=0.5*a*b2 (a and b are the longest and shortest diameters of the tumor, respectively). Pairwised tumor volumes were significantly different (P<0.001) since the third week, although it hadn't been significant before the third week as the treatments to all the test groups were similar. (B) Tumor inhibition rate in each group changed as the treatments carried on.
Measurement of tumor volume started during the second week of the experiment. In the second week, the mean tumor volumes of each group were 0.26±0.03 cm3 in the control group, 0.21±0.03 cm3 in the conventional group, 0.23±0.03 cm3 in the metronomic group and 0.22±0.03 cm3 in the combination group. Dunnett's T3 test showed that there was no statistical significance among pairwise comparisons except for the conventional group vs the control group and the combination group vs the control group. It seemed that both conventional and combination chemotherapy schedules were effective from the very beginning of treatment, whereas metronomic scheduling was not. The result for the initial time of treatment made sense because the medicine dosage was much higher in conventional and combination chemotherapy than in metronomic therapy, indicating a much greater cytotoxic effect on tumor cells.
In the third week of chemotherapy, not only a significant difference was observed between the control and treated groups, but also the effects of the three treated groups were distinct from each other. All three treated groups showed a significant inhibitory effect on tumor growth (P<0.001) (Figure 2A). However, as indicated by the trends of the growth curve, the trends with the conventional therapy and the metronomic therapy were similar to each other and differed from that with the combination therapy. Moreover, the tumor inhabitation rates were calculated in order to investigate the inhibitory effects on tumor growth (Figure 2B). All three therapies showed continuously increasing tumor inhibition until the sixth week. In the sixth week, knee points appeared on the curves of both the conventional and the metronomic therapy groups, followed by a continuous decrease in tumor inhabitation rate, indicating a failure of inhibition of tumor growth. In other words, after several weeks of treatment, both the conventional and the metronomic scheduling of chemotherapy lost their inhibitory effect on the tumor. In contrast, combination therapy produced a sustained positive treatment response to tumors.
After the 8th week of chemotherapy, all the rats were killed, and the tumors were removed from the bodies. The volume and weight of the tumors were determined. The mean weights of the tumors were 4.14±0.28 g, 3.64±0.28 g, 3.15±0.22 g and 0.86±0.10 g in the control, conventional, metronomic and combination groups, respectively. The mean volumes of the tumors were 4.15±0.30 cm3, 3.45±0.19 cm3, 2.89±0.27 cm3, 0.81±0.10 cm3 in the control, conventional, metronomic and combination groups, respectively. The overall difference among the groups and pairwise difference between each treatment group and the control group were statistically confirmed by Dunnett's test (P<0.001). Additionally, combination therapy was distinct from the other two therapies (P<0.001, Figure 3). All three schedules of chemotherapy showed effective tumor inhibition, with the combination scheduling showing the strongest effect.
VEGFA expression was affected by different chemotherapy scheduling
Western blot assays revealed that, compared to the control group, expression of VEGFA in all three treatment groups decreased. Statistical significance was observed in all three groups (P<0.01). The expression of VEGFA in the metronomic schedule group and in the combination group was much lower than in the conventional schedule group (Figure 4).
Relative expression of VEGFA in four groups. (A) Relative expression of VEGFA in four groups, β-actin was used as an internal control to normalize the loading capacity while expression of VEGFA in control group was used as an external control. (B) Western blot analysis for the expression of VEGFA in four therapy groups. cP<0.01 compared to the mean ratio of VEGFA/β-actin in control.
Discussion
Despite being one of the most popular chemotherapy options for osteosarcoma at present and having a significant tumor cell necrosis effect, neoadjuvant chemotherapy has little significant effect on prognosis17, 18. The growth and metastasis of osteosarcoma, a highly malignant tumor rich in blood vessels, are related to its angiogenesis19. Some agents used in conventional chemotherapies show a strong antiangiogenic and inhibitory effect on tumors at low doses of almost 1/3 to 1/20 of the maximum tolerated dose when administered at a higher frequency. The administration of low-dose, high-frequency chemotherapy was named metronomic scheduling in 200020, 21. It has been proven to be a more efficient method than the combination of different schedules of chemotherapy in previous studies on many other tumors22, 23, 24. However, for the treatment of osteosarcoma, there is little evidence to elucidate the effect of combination scheduling. The shortcomings of current conventional chemotherapy and the misery associated with the possibility of amputation made it urgent to investigate the effectiveness of combination chemotherapy scheduling in the treatment of osteosarcoma. Our study is to prove the effectiveness of combination chemotherapy scheduling in osteosarcoma tumor suppression.
The goal of combination scheduling is to integrate the superiority of the two kinds of chemotherapy scheduling: the maximum tolerated dose of conventional scheduling to kill tumor cells and the higher frequency of metronomic scheduling to inhibit angiogenesis.
The UMR 106 cell line is a transplantable rat osteosarcoma model with stable growth and high lung metastatic potential25, which makes it an appropriate cell line for our animal modeling. Osteosarcoma is the most common malignant bone tumor in childhood and adolescence, and the thymus gland plays an important role in producing T cells to bolster the immune system during this period of development. Given their deteriorated or absent thymus, nude mice are a less effective model for osteosarcoma than SD rats. Additionally, in our experiment, to amplify the tumorigenicity of UMR 106 in SD rats, which have a stronger immunity than nude mice, the cells were generated in nude mice for several cycles. The repeated generations resulted in enhanced tumorigenicity of the cell line.
According to some clinical data, the tumors of a considerable number of patients stop activating, neither growing nor shrinking after conventional chemotherapy26. On the other hand, in some recent research, it was reported that a single cycle of continuous low-dose antiangiogenic chemotherapy could accelerate metastasis after short-term treatment27. This result may be due to the tolerance of tumor cells to medicines—in other words, a loss of sensitivity to chemotherapy. However, the antiangiogenic effect of chemotherapy keeps tumor from growing. In our in vivo experiments, all three chemotherapies showed antiangiogenic effects. As shown by the tumor growth curves and the tumor inhibition rates (Figure 2), conventional and metronomic scheduling shared similar curve trends even though conventional scheduling showed an effect much earlier, which could be explained by the much higher dose used in conventional scheduling. After the sixth week of observation, knee points appeared on the growth curves of both the conventional and the metronomic scheduled treatments. Metronomic chemotherapy had a better effect over the last few weeks. The negative change in tumor growth indicated that both of the schedules inhibited tumor cells. Further studies will be carried out to identifythe mechanism and whether tolerance developed, the tumor progressed or the immune system collapsed. However, our results confirm the previous finding that tolerance to medicines could arise not only in conventional scheduling but also in metronomic scheduling.
In the first few weeks of the study, the tumor growth curve of the combination schedule had almost the same trend as the other two schedules. However, after the sixth week of observation, unlike the other two therapies, the combination schedule's inhibitory effect on tumor cells persisted.
The antiangiogenic and apoptotic activity of metronomic scheduling of chemotherapeutic agents has been demonstrated for 4-hydroperoxycyclophosphamide, taxanes, epothilones and vinblastine in several studies28, 29. VEGFA is a member of the VEGF family and encodes a protein that has an important effect on angiogenesis. VEGFA was proven to increase in expression level and contribute to angiogenesis in cancer30, 31, 32 . In our study, the results of western blot assays indicated statistically decreased expression of VEGFA in all therapy groups. Additionally, the metronomic and the combination schedule groups showed a much lower VEGFA expression than the conventional group, which indicated that therapy on the metronomic and combination schedules may have a superior antiangiogenic effect.
In conclusion, in osteosarcoma-bearing SD rats models, we have found that the combination of conventional and metronomic scheduling of chemotherapy was a better strategy than either schedule alone. By combining the administration of conventional and metronomic scheduling, with the intermittent high dose of conventional therapy and the continuous low dose of metronomic chemotherapy, the combination scheduling might not only promote tumor necrosis but also inhibit angiogenesis of tumor.
To obtain more evidence of the clinical value of combination chemotherapy scheduling, further in vitro studies on tumor lung metastasis, real-time PCR of related genes, immunohistochemistry and northern blot assays should be carried out.
Author contribution
Dr Jiong MEI designed the research. Dr Hong-mei Yin contributed new reagents or analytic tools. Dr Xiao-zhong Zhu performed the experiments and wrote the paper.
References
Longhi A, Errani C, De Paolis M, Mercuri M, Bacci G . Primary bone osteosarcoma in the pediatric age: state of the art. Cancer Treat Rev 2006; 32: 423–36.
Quan GM, Ojaimi J, Nadesapillai AP, Zhou H, Choong PF . Resistance of epiphyseal cartilage to invasion by osteosarcoma is likely to be due to expression of antiangiogenic factors. Pathobiology 2002; 70: 361–7.
Dass CR, Ek ET, Contreras KG, Choong PF . A novel orthotopic murine model provides insights into cellular and molecular characteristics contributing to human osteosarcoma. Clin Exp Metastasis 2006; 23: 367–80.
Wittig JC, Bickels J, Priebat D, Jelinek J, Kellar-Graney K, Shmookler B, et al. Osteosarcoma: a multidisciplinary approach to diagnosis and treatment. Am Fam Physician 2002; 65: 1123–32.
Ferguson WS, Goorin AM . Current treatment of osteosarcoma. Cancer Invest 2001; 19: 292–315.
Ferrari S, Smeland S, Mercuri M, Bertoni F, Longhi A, Ruggieri P, et al. Neoadjuvant chemotherapy with high-dose Ifosfamide, high-dose methotrexate, cisplatin, and doxorubicin for patients with localized osteosarcoma of the extremity: a joint study by the Italian and Scandinavian Sarcoma Groups. J Clin Oncol 2005; 23: 8845–52.
Rosen G, Caparros B, Huvos AG, Kosloff C, Nirenberg A, Cacavio A, et al. Preoperative chemotherapy for osteogenic sarcoma: selection of postoperative adjuvant chemotherapy based on the response of the primary tumor to preoperative chemotherapy. Cancer 1982; 49: 1221–30.
Enneking WF . Advances and treatment of primary bone tumors. J Fla Med Assoc 1979; 66: 28–30.
Rosenburg SA, Chabner BA, Young RC, Seipp CA, Levine AS, Costa J, et al. Treatment of osteogenic sarcoma. I. Effect of adjuvant high-dose methotrexate after amputation. Cancer Treat Rep 1979; 63: 739–51.
Campanacci M, Bacci G, Bertoni F, Picci P, Minutillo A, Franceschi C . The treatment of osteosarcoma of the extremities: twenty year's experience at the Istituto Ortopedico Rizzoli. Cancer 1981; 48: 1569–81.
Chou AJ, Gorlick R . Chemotherapy resistance in osteosarcoma: current challenges and future directions. Expert Rev Anticancer Ther 2006; 6: 1075–85.
Browder T, Butterfield CE, Kraling BM, Shi B, Marshall B, O'Reilly MS, et al. Antiangiogenic scheduling of chemotherapy improves efficacy against experimental drug-resistant cancer. Cancer Res 2000; 60: 1878–86.
Isobe K, Shimizu T, Nikaido T, Takaoka K . Low-voltage electrochemotherapy with low-dose methotrexate enhances survival in mice with osteosarcoma. Clin Orthop Relat Res 2004; 426: 226–31.
Lau DH, Xue L, Young LJ, Burke PA, Cheung AT . Paclitaxel (Taxol): an inhibitor of angiogenesis in a highly vascularized transgenic breast cancer. Cancer Biother Radiopharm 1999; 14: 31–6.
Hanahan D, Bergers G, Bergsland E . Less is more, regularly: metronomic dosing of cytotoxic drugs can target tumor angiogenesis in mice. J Clin Invest 2000; 105: 1045–7.
Elmslie RE, Glawe P, Dow SW . Metronomic therapy with cyclophosphamide and piroxicam effectively delays tumor recurrence in dogs with incompletely resected soft tissue sarcomas. J Vet Intern Med 2008; 22: 1373–9.
Bacci G, Forni C, Ferrari S, Longhi A, Bertoni F, Mercuri M, et al. Neoadjuvant chemotherapy for osteosarcoma of the extremity: intensification of preoperative treatment does not increase the rate of good histologic response to the primary tumor or improve the final outcome. J Pediatr Hematol Oncol 2003; 25: 845–53.
Goorin AM, Schwartzentruber DJ, Devidas M, Gebhardt MC, Ayala AG, Harris MB, et al. Presurgical chemotherapy compared with immediate surgery and adjuvant chemotherapy for nonmetastatic osteosarcoma: Pediatric Oncology Group Study POG-8651. J Clin Oncol 2003; 21: 1574–80.
Patel SJ, Lynch JW Jr, Johnson T, Carroll RR, Schumacher C, Spanier S, et al. Dose-intense ifosfamide/doxorubicin/cisplatin based chemotherapy for osteosarcoma in adults. Am J Clin Oncol 2002; 25: 489–95.
Browder T, Butterfield CE, Kraling BM, Shi B, Marshall B, O'Reilly MS, et al. Antiangiogenic scheduling of chemotherapy improves efficacy against experimental drug-resistant cancer. Cancer Res 2000; 60: 1878–86.
Hanahan D, Bergers G, Bergsland E . Less is more, regularly: metronomic dosing of cytotoxic drugs can target tumor angiogenesis in mice. J Clin Invest 2000; 105: 1045–7.
Cham KK, Baker JH, Takhar KS, Flexman JA, Wong MQ, Owen DA, et al. Metronomic gemcitabine suppresses tumour growth, improves perfusion, and reduces hypoxia in human pancreatic ductal adenocarcinoma. Br J Cancer 2010; 103: 52–60.
Tang TC, Man S, Lee CR, Xu P, Kerbel RS . Impact of metronomic UFT/cyclophosphamide chemotherapy and antiangiogenic drug assessed in a new preclinical model of locally advanced orthotopic hepatocellular carcinoma. Neoplasia 2010; 12: 264–74.
Italiano A, Toulmonde M, Lortal B, Stoeckle E, Garbay D, Kantor G, et al. “Metronomic” chemotherapy in advanced soft tissue sarcomas. Cancer Chemother Pharmacol 2010; 66: 197–202.
Quan GM, Choong PF . Anti-angiogenic therapy for osteosarcoma. Cancer Metastasis Rev 2006; 25: 707–13.
Chou AJ, Gorlick R . Chemotherapy resistance in osteosarcoma: current challenges and future. Expert Rev Anticancer Ther 2006; 6: 1075–85.
Ebos JM, Lee CR, Cruz-Munoz W, Bjarnason GA, Christensen JG, Kerbel RS . Accelerated metastasis after short-term treatment with a potent inhibitor of tumor angiogenesis. Cancer Cell 2009; 15: 232–9.
Bacci G, Ferrari S, Longhi A, Picci P, Mercuri M, Alvegard TA, et al. High dose ifosfamide in combination with high dose methotrexate, adriamycin and cisplatin in the neoadjuvant treatment of extremity osteosarcoma: preliminary results of an Italian Sarcoma Group/Scandinavian Sarcoma Group pilot study. J Chemother 2002; 14: 198–206.
Klement G, Huang P, Mayer B, Green SK, Man S, Bohlen P, et al. Differences in therapeutic indexes of combination metronomic chemotherapy and an anti-VEGFR-2 antibody in multidrug-resistant human breast cancer xenografts. Clin Cancer Res 2002; 8: 221–32.
Dai H, Zhao S, Xu L, Chen A, Dai S . Expression of Efp, VEGF and bFGF in normal, hyperplastic and malignant endometrial tissue. Oncol Rep 2010; 23: 795–9.
Xie TX, Xia Z, Zhang N, Gong W, Huang S . Constitutive NF-kappaB activity regulates the expression of VEGF and IL-8 and tumor angiogenesis of human glioblastoma. Oncol Rep 2010; 23: 725–32.
Hall K, Ran S . Regulation of tumor angiogenesis by the local environment. Front Biosci 2010; 15: 195–212.
Acknowledgements
This work was supported in part by the National Natural Science Foundation of China (No 30471760). We thank Dr Gai-ling LI (H&H Life Science Research Center) for her direction to our data analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhu, Xz., Yin, Hm. & Mei, J. Inhibition of tumors cell growth in osteosarcoma-bearing SD rats through a combination of conventional and metronomic scheduling of neoadjuvant chemotherapy. Acta Pharmacol Sin 31, 970–976 (2010). https://doi.org/10.1038/aps.2010.97
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2010.97