Abstract
Aim:
The cytotoxicity of marcaine was estimated in combination with a calcium channel blocker. In addition, the influence of marcaine and marcaine plus lekoptin on a model system using the H9C2 cardiac cell line was investigated.
Methods:
Cells were incubated for five hours with marcaine, lekoptin, or with both drugs simultaneously. Apoptotic cells were detected using the TUNEL assay and the alkaline comet assay. Mitochondrial cell function after drug uptake was examined using the MTT assay. The concentration of MDA (malondialdehyde) — the final product of fatty-acid peroxidation, was quantified spectrophotometrically. The expression of glutathione S-transferase π (GST-π) was detected by immunofluorescence (IF) and Western blotting (WB) and inducible nitric oxide synthase (iNOS) was assessed by immunocytochemical staining (ABC).
Results:
Incubation with marcaine resulted in the highest number of apoptotic cells. After incubation with both marcaine and lekoptin, moderate damage to cells (54.2%±1.775% of DNA destruction) was observed. The highest levels of iNOS and GST-π expression were observed in cells treated with marcaine and marcaine plus lekoptin. The characteristic nuclear GST-π expression was observed in cells treated with both drugs.
Conclusion:
Lekoptin stimulated cells to proliferate. Marcaine caused membrane damage and ultimately cell death.
Similar content being viewed by others
Introduction
Calcium acts as an intracellular messenger to modulate many aspects of cell physiology. Intracellular calcium signaling plays an essential role in cardiac physiology and modulates cardiac gene expression. However, the role of intracellular calcium signaling during cardiac development and the ability of calcium to modulate the differentiation of striated muscle cells are poorly understood1, 2, 3, 4.
The primary target for marcaine's cardiotoxic action is generally considered to be voltage-gated sodium channels. Results from isolated heart studies as well as other studies suggest that the actions of bupivacaine (marcaine) on sodium channels probably contribute to the cardiotoxic effects5, 6, 7. Some authors have noted that nitric oxide (NO) acts in calcium signaling as an inter- and intracellular messenger in various types of cells. Pathogenic stimulation, such as inflammatory response, may induce the production of NO, which is mediated mainly by inducible nitric oxide synthase (iNOS). The role of NO generation by cardiomyocytes and the expression of NOS isoforms is still unclear. Cardiomyocytes have been reported to express two NOS isoforms , endothelial and inducible, in disease states8, 9, 10. It was also reported that cardiac cells express neither iNOS nor eNOS immunoreactivity in both infracted and normal myocardium11, 12, 13.
The crucial antioxidant enzymes that protect cells from oxidative stress are SOD, glutathione S-transferase, catalase, and glutathione peroxidase14. Glutathione-S-transferase π (GST-π) is involved in a variety of cell detoxification processes. We investigated the level of expression of GST-π in cells treated with commonly used medicines. Increased expression of GST-π in different normal and tumor cells is associated with reduced sensitivity to cytostatics. Oxidative stress is an important component of cytostatic-induced apoptosis. GSTs are believed to detoxify endogenous substances that are formed as a consequence of oxidative stress, including lipid hydroperoxides and hydroxyalkenals. Therefore, increased GST-π expression in cells may protect them against drug-induced oxidative stress and, thus, apoptosis5. Isomoto et al hypothesized that some antiarrhythmic drugs might cause cardiotoxicity through the induction of apoptosis15.
There is little known about drug oxidation and toxicity in the heart. Cardiotoxicity occurs during therapy with several cytotoxic drugs and may be the dose-limiting factor in treatment and cell response16. Lekoptin is often used for the treatment of ventricular arrhythmia and is a potent blocker of calcium channels. Walles et al showed that heart tissue successfully metabolized verapamil17. Other authors have demonstrated an increase in cardiotoxicity when doxorubicin was given in combination with verapamil and several different mechanisms have been proposed for this effect. One mechanism is based on the capacity of verapamil to inhibit the function of P-glycoprotein and therefore increase intracellular cytotoxic drug concentrations. This effect may be useful for cancer chemotherapy, but it could also lead to toxic effects in normal cells, such as cardiac cells16. However, some studies show increased doxorubicin accumulation in rat cardiomyocytes incubated in doxorubicin in combination with verapamil18, 19. In another study, inhibition of L-type Ca2+ channels was implicated in the cardiac depression induced by bupivacaine (marcaine), which causes a stronger arrhythmogenic effect and is probably related to enantiomer-specific binding to Na+ or K+ channels20. The authors found an increased cardiotoxic (arrhythmias) effect caused by R(+)bupivacaine, compared with S(−)bupivacaine20. Marcaine is one of the most commonly used anesthetics in contemporary medicine, especially in obstetrics. It blocks sodium channels, with consequent retardation of stimulus production and conduction, and also causes oxidative stress, leading to cell death21, 22. Cesselli et al concluded that this might constitute the most proximal event in heart failure23. However, Lenfant et al indicated that bupivacaine was effective in protecting erythrocytes against oxidative stress24, 25.
We performed studies on H9C2 cells, which are a rat myoblast cell line that differentiates in vitro. We examined the influence of the L-type calcium channel blocker lekoptin (verapamil), the local anesthetic marcaine, and a combination of these two agents. Both drugs are used in common medical practice; thus, it is important to analyze their actions in the human body. One of the first events that can be studied is oxidative stress, a disturbance of the pro- and antioxidative balance. The aim of this study included determination of the relative toxicities of marcaine and lekoptin, factors predisposing cells to toxicity, the mechanisms of these toxic effects, and the actions of these drugs.
Materials and methods
Cell culture
H9C2 rat heart myocardium cells (a gift from Prof Fluvio URSINI of University of Padova) were grown in DMEM medium (Sigma) with the addition of 10% fetal bovine serum (FBS), 2 mmol/L glutamine, 104×diluted 10 000 U/mL penicillin, 10 mg/mL streptomycin (Sigma), and 0.05 mmol/L selenite (Sigma). For experiments, cells were removed by trypsinization and washed with PBS. The cells were maintained in a humidified atmosphere at 37 °C in 5% CO2.
Culturing with marcaine and lekoptin
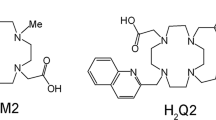
Marcaine and lekoptin (Polfa, Poland) were obtained from Dr Z SACZKO of the A. Falkiewicz Specialists' Hospital of Wroclaw, Poland. Cells were incubated for five hours in three combinations of clinically used concentrations: with marcaine (CM=6 μg/mL), with lekoptin (verpamili hydrochloridum) (CL=952 μg/mL), and both drugs simultaneously. The five hour incubation time was established from previous experiments. This time was optimal for observing the interaction between drugs and cells.
Lipid peroxidation
After in vitro treatment with the drugs , the cells were removed by trypsinization and resuspended in PBS. The final product of fatty-acid peroxidation, malondialdehyde (MDA), reacts with TBA to form a colored complex. The level of TBARS was measured by the absorbance at a wavelength of 535 nm. The concentration of MDA was quantified spectrophotometrically based on a set of MDA standards of known concentration.
Alkaline comet assay (ACA)
For the detection of DNA fragmentation associated with apoptosis, the alkaline comet assay method was used26. Cells at a concentration of 1×105/mL were mixed with low-melting-point agarose (Sigma) at a ratio of 1:10 (v/v) and spread on a slide. The slides were submerged in precooled lysis solution (2.5 mol/L NaCl, 100 mmol/L EDTA, pH 10, 10 mmol/L Tris base, and 1% Triton X-100) at 4 °C for 60 min. After being lysed and rinsed, the slides were equilibrated in TBE solution (40 mmol/L Tris/boric acid, 2 mmol/L EDTA, pH 8.3), electrophoresed at 1.0 V/cm2 for 20 min, and stained using the silver staining method27. To score the comet pattern, 100–200 nuclei from each slide were counted by two independent investigators.
Apoptosis - TUNEL assay
DNA fragmentation was visualized using an ApopTag® (Qbiogene) kit. In the TUNEL assay the enzyme terminal deoxynucleotidyl transferase labels the 3′-OH ends of DNA generated during apoptosis with biotinylated nucleotides. These fragments are detected by immunoperoxidase staining. The apoptosis detection kit distinguishes apoptosis from necrosis by specifically detecting the DNA cleavage and chromatin condensation associated with apoptosis. Experiments were performed on 8-well slides. Cells with stained nuclei were determined by counting 100 cells in 3 randomly selected fields. The counting was performed by two independent investigators. Samples were examined with an upright microscope (Olympus BX51).
Cell proliferation
Cytotoxicity was determined by the MTT assay (Sigma, In Vitro Toxicology Assay). Cells were seeded onto 96-well plates at a concentration of 5×103 cells/well. For the viability assay the cells were exposed to a combined-drug therapy. Following incubation for 5 and 24 h at 37 °C, the medium was removed and 100 μL 0.04 mol/L HCl in 2-propanol (Sigma) was added. The absorbance at 570 nm was measured spectrophotometrically (Multiscan MS microplate reader) and results were expressed as a percentage of the untreated control (% of control).
Immunocytochemistry
Immunocytochemistry was performed using the ABC method. Briefly, cultures were fixed and dehydrated using 4% paraformaldehyde and an ethanol gradient, respectively. The samples were then permeabilized and blocked by incubation with 0.1% Triton X-100 in PBS. Inducible nitric oxide synthase was visualized with mouse monoclonal antibody (1:100, NOS2 and Ki-67, Santa Cruz). For conventional bright-field microscopy (peroxidase-ABC labeling), the samples were incubated with a diaminobenzidine-H2O2 mixture to visualize the peroxidase label and counterstained with hematoxylin for 30 s. The samples were examined using an upright microscope (Olympus BX51). Stained cell numbers were determined by counting 100 cells in 3 randomly selected fields. The counting was performed by two independent investigators. The result was judged to be positive if staining was observed in more than 5% of cells. The intensity of immunohistochemical staining was evaluated as (−) negative (no reaction), (+) weak, (++) moderate, and (+++) strong. All experiments were repeated three times.
Immunofluorescence
To visualize the expression of glutathione S-transferase π after marcaine and lekoptin treatment, H9C2 cells were plated in 600 μL of growth medium into an eight-chambered coverglass (Nunc) and grown for two days. The cells were then incubated for five hours with both drugs. After incubation, the cells were fixed with 99.9% methanol. The intracellular localization of GST-π (rabbit polyclonal antibody, 1:100, Novoacstra) labeled with TRITC (tetramethylrhodamine isothiocyanate, excitation wavelength of 541 nm and emission wavelength of 572 nm) was monitored using a confocal laser scanning microscope (Olympus FluoView FV1000).
Subcellular fractionation
Cells were harvested in 700 μL of lysis buffer (50 mmol/L Tris-HCl, 150 mmol/L NaCl, 1 mmol/L EDTA, 1% Triton X-100, pH 8.0) containing a cocktail of protease inhibitors (Roche) and sonicated with a Vibra-Cell YC-130PB (Labo-Plus) at level 60 for 40 s. Cell lysates were centrifuged for 20 min at 600×g in a Sigma 3K18 centrifuge using the 12154-H rotor to pellet nuclei. The supernatant was further centrifuged at 100 000×g for 60 min in a UP-65 centrifuge. The final supernatant was designated the cytosolic fraction. The proteins contained in the supernatant and pellet were subjected to SDS-PAGE/Western blot.
SDS-PAGE and immunoblotting
Whole-cell lysates were characterized by SDS-PAGE, according to the methods of Laemmli, using 10% mini gels (Bio-Rad). A dual Color molecular weight marker (Bio-Rad) was used as a size standard. For immunoblotting, after SDS-PAGE, the gel was electrophoretically transferred to an Immobillon P (Millipore) membrane with transfer buffer (10 mmol/L Tris, 150 mmol/L glycine, 20% methanol) at 4 °C for 1.5 h and at 1.2 mA/1 cm2 of membrane. The transfer and immunoblotting were performed according to the procedure described in the Millipore manual. Briefly, the membrane with transferred proteins was incubated at 37 °C for 1 h with a rabbit antibody against GST (Santa Cruz Biotechnology) diluted at 1:200 in 1% BSA in Tris-HCl buffer saline containing 0.05% Tween-20 (TBS-T, 20 mmol/L Tris-HCl, pH 7.0, 50 mmol/L NaCl, 0.05% Tween-20). The membrane was then incubated at 37 °C for 1 h with goat anti-rabbit IgG conjugated with horseradish peroxidase (Sigma) diluted 1:1000 in TBS-T. The membrane was washed four times in TBS for 10–15 s after each incubation with antibodies. Immunoblots were developed with a 4-chloro-1-α-naphtol substrate solution in the presence of H2O2.
Statistical analysis
The normality of the continuous variables was checked by the Saphiro-Wilk test. The significance of the difference between mean values of different groups of cells compared with the control group (untreated cells) was assessed by Student's t-test with values of P≤0.05 taken as statistically significant. Statistical analysis was performed using Statistica 6 software.
Results
Lipid peroxidation
Rat myoblasts were incubated for five hours with marcaine or lekoptin (as a calcium channel blocker) and simultaneously with both drugs. The high level of MDA (Figure 1) shows that marcaine increases MDA concentration in H9C2 cells to 0.726±0.45μmol/L . However, we also observed an increase in cells treated with lekoptin (0.565±0.369 μmol/L). Incubation with both drugs resulted in a lower level of MDA than in the control cells (Figure 1). No statistically significant differences were seen between the groups.
Alkaline comet assay (ACA)
The results of ACA are shown in Figure 2. The highest number of apoptotic cells was seen in cells treated with marcaine only (65%±5.7% of cells). Results obtained for marcaine were statistically significant. Cells treated with lekoptin and treated simultaneously with both drugs showed the same level of apoptosis (54.2%±1.775% of cells). Surprisingly, some necrotic cells (5.25%±6.625%) were observed among the cells treated with lekoptin. The same level (13.95%±1.6% of cells) of intermediate damage was seen for the drug combination and control cells (14.4%±4.825%).
MTT assay
The oxidoreductive mitochondrial function is shown in Figure 3. The 24-h incubation with marcaine resulted in the greatest damage to mitochondrial function (16.29%±0.075% compared with control cell level). The levels of viability after 5 and 24 h with lekoptin were comparable and exceeded 100% of the control cells. In the cells treated with both drugs, we observed a statistically significant decrease in viability after 24 h, to 17.57%±0.086% of that of control cells. The 5-h incubation post therapy was the first stage in which changes in cells were observed. The 24 hour period after therapy was established for the cytotoxicity assay. After that period, no significant changes were detected.
TUNEL assay
Figure 4 shows the H9C2 TUNEL assay. Cells incubated with marcaine and with both drugs showed the strongest TUNEL positivity (as assayed by stained cell nuclei) (Figure 4A, 4B). Single apoptotic cells were observed (not present) in the cells treated with lekoptin or in the control cells (Figure 4C, 4D, Table 1).
iNOS expression
The highest expression of inducible nitric oxide synthase was also observed for cells treated with marcaine and both marcaine and lekoptin (Figure 5A, 5B). In cells incubated only with lekoptin, no significant iNOS expression was observed (figures not included); the results were comparable to that of control cells (Table 2).
Ki67 expression
The expression of a marker for cell proliferation (Ki-67) is presented in Figure 6A–6D). In the cells treated with marcaine the reaction was about 5%, comparable with that of control cells (Figures 6A, 6D). The strongest nuclear staining was seen in cells treated with lekoptin (Figure 6C) and both drugs (Figure 6B, Table 3).
GST-π expression and immunoblotting
The expression of S-glutathione transferase π demonstrated a specific nuclear localization in cells treated with both drugs (Figure 7B). In the cells treated with only marcaine, GST-π expression was observed in the cytoplasm and the nuclear envelope (Figure 7A). The control cells and cells treated with lekoptin demonstrated very weak enzyme expression (data not shown). To complement the immunofluorescence results, immunoblotting of cytosolic and nuclear fractions was performed and presented in Figure 8. This permitted us to demonstrate a characteristic immunoreactive protein band at 26 and 50 kDa, particularly in the nuclear fraction of H9C2. In the cytosolic fraction we observed split bands of NFκB p50-GST protein (50 kDa) for samples treated with marcaine and for control cells. The same probes also indicated no significant expression of GST fusion proteins (26 kDa). The staining was detectable in the nuclear fraction of all samples (it was the weakest band in the control probe). The strongest band appeared for cells treated with lekoptin, followed by marcaine and both drugs. This is partially a confirmation of fluorescent immunolabeling in confocal microscopy, but this strong immunoblotting result is unexpected for lekoptin treatment.
Discussion
The present study showed the cytotoxic effect of marcaine on rat myoblasts in vitro. Five hours of incubation with marcaine led to higher levels of lipid peroxidation, higher expression levels of iNOS and GST-π, and damaging action on mitochondrial function. In addition, marcaine caused membrane damage and, finally, cell death. Mitochondria have recently been shown to be involved in apoptosis and have been implicated in the generation of reactive oxygen species (ROS). Singh et al suggest that mitochondrial DNA determines the cellular response to cancer therapeutics and some drugs can induce mutations in the mitochondrial genome28. There is a question of whether similar mutations could occur in normal cardiac cells . Our results show that marcaine mainly induces the late phase of apoptosis (comet assay) and causes irreparable changes in cells. Contrary to the therapeutic effect of marcaine, lekoptin application indicated a protective role for the H9C2 cell line and stimulation of further cell proliferation. These results were confirmed by the MTT assay and Ki67 labeling. In cells incubated with only lekoptin we observed single apoptotic nuclei (TUNEL assay). Thus, we conclude that this mechanism may account for the protective effect of lekoptin against oxidative stress in this model. The action of lekoptin has membrane stabilizing properties that may induce changes in membrane polarization. It blocks calcium channels, which should cause a more intensive action of marcaine. Isomoto et al showed that selective blockers of Na+, K+, and Ca2+ channels or β-adrenergic receptor did not induce apoptosis in H9C2 cells, but the authors indicated that some antiarrhythmic drugs (eg, amiodarone) had a pro-apoptotic effect on cardiac cells15.
Similar to our study, others have shown that expression of this synthase was markedly increased in cardiomyocytes and endothelial cells in the hearts of spontaneously hypertensive rats, which indicates a pathophysiological significance of altered iNOS expression12.
Some studies have shown that bupivacaine induces apoptosis in the RT4-D6P2T cell line, which may be associated with ROS production29, 30. The ROS level was elevated in Schwann cells during the early period of bupivacaine-induced apoptosis. In contrast to our study, those authors did not observe a significant increase in NO level31. Feinstein et al showed that bupivacaine causes cell death in cardiac myocytes and dibucaine induces apoptosis in HL-60 cells32. In another study, verapamil and nimodipine, drugs that reduce cardiac automatism, were effective in decreasing cardiac toxicity induced by racemic bupivacaine24.
Glutathione S-transferase (GST) isoenzymes are important in the detoxification of lipid peroxidation products; they bind glutathione (GSH) to a variety of electrophiles, including carcinogens and cytotoxic drugs14. The isoenzymes of class pi are highly sensitive to ROS. In the present study we demonstrated the increased expression of the detoxification enzyme GST π, after treatment with marcaine. Vander Heide et al have shown that regulated increased expression of GST in cardiac myoblasts protected against anthracycline-induced cell death33. Our data indicate a correlation between oxidative stress and cell death after marcaine treatment, which was reduced by GST-π overexpression. This suggests that oxidative stress is important in both apoptotic and necrotic cell death. L'Ecuer et al indicated that GST overexpression eliminated the oxidative stress generated by doxorubicin in the H9C2 cell line. The authors suggested that other factors in addition to oxidative stress played a role in DOX-induced cell death14. In contrast to our study, some authors indicate only cytoplasmaic expression of GST-π in normal cells34. Our results showed an unexpected nuclear expression of this enzyme in cells incubated with marcaine and lekoptin. However, other authors have demonstrated that nuclear expression of this enzyme is characteristic of neoplastic cells35, which suggests that there are neoplastic changes in cells induced by applied drugs. However, some authors suggest that GST overexpression may be an important part of a protective strategy against drug-induced cell death14.
In conclusion, our study confirms evidence for an interaction between these two drugs, which could be of importance in clinical practice. The present in vitro study demonstrated an interaction between marcaine and lekoptin affecting the response of rat myoblasts to oxidative stress. We have shown that marcaine can induce apoptosis in cardiomyocytes, which can be mediated by the increase of intracellular levels of oxidative stress that involve the activation of inducible nitric oxide synthase. The protective action of lekoptin against marcaine and oxidative stress and the contribution of GST detoxification mechanism were verified. There is a need for further studies to explain the mechanism of this interaction.
Author contribution
Julita KULBACKA and Jolanta SACZKO designed research; Agnieszka CHWILKOWSKA, Malgorzata DUMANSKA, Malgorzata DRAG-ZALESINSKA, Teresa WYSOCKA, Kamilla STACH, Iwona BEDNARZ and Mateusz LUGOWSKI performed research; Julia BAR and Anna MARCINKOWSKA contributed new reagents or analytic tools; Julita KULBACKA, Jolanta SACZKO and Julia BAR analyzed data; Julita KULBACKA and Andrzej GAMIAN wrote the paper.
References
Berthel H, Ebel D, Mullenheim J, Obal D, Preckel B, Schlack W . Effect of lidocaine on ischaemic preconditioning in isolated rat heart. Br J Anaesth 2004; 93: 698–704.
Olschewski A, Wolff M, Brau ME, Hempelmann G, Vogel W, Safronov BV . Enhancement of delayed-rectifier potassium conductance by low concentrations of local anaesthetics in spinal neurones. Br J Pharmacol 2002; 136: 540–9.
Heavner JE . Cardiac toxicity of local anesthetics in the intact isolated heart model: a review. Reg Anesth Pain Med 2002; 27: 545–55.
Porter GA, Makuck RF, Rivkees SA . Reduction in intracellular calcium levels inhibits myoblast differentiation. J Biol Chem 2002, 277: 28942–7.
Doi K, Hasegawa K, Fujita M, Yamazato A, Yamanaka K, Watanabe M, et al. Clinical characteristics relevant to myocardial cell apoptosis: analysis of pericardial fluid. Interact Cardiovasc Throat Surg 2004; 3: 359–62.
Klopstock T . Drug-induced myopathies. Curr Opin Neurol 2008; 21: 590–5.
Royse CF, Royse AG . The myocardial and vascular effects of bupivacaine, levobupivacaine, and ropivacaine using pressure volume loops. Anesth Analg 2005; 101: 679–87.
Singh K, Balligand JL, Fischer TA, Smith TW, Kelly RA . Glucocorticoids increase osteoponin expression in cardiac myocytes and microvascular endothelial cells. Role in regulation of inducible nitric oxide synthase. J Biol Chem 1995; 270: 28471–8.
Ziolo MT, Kohr MJ, Wang H . Nitric oxide signalling and the regulation of myocardial function. J Mol Cell Cardiol 2008; doi:10.1016/j.yjmcc.2008.07.015 (article in press).
Ungureanu-Longrois D, Balligand JL, Kelly RA, Sminth TW . Myocardial contractile dysfunction in the systemic inflammatory response syndrome: role of a cytokine-inducible nitric oxide synthase in cardiac myocytes. J Mol Cell Cardiol 1995; 27: 155–67.
Turner JJO, Rice-Evans CA, Davies TMJ, Newman ESR . The formation of free radicals by cardiac myocytes under oxidative stress and the effects of electron-donating drugs. Biochem J 1991; 277: 833–7.
Buchwalow IB, Schulze W, Karczewski P, Kostic MM, Wallukat G, Morwinski R, et al. Inducible nitric oxide synthase in the myocard. Mol Cell Biochem 2001; 217: 73–82.
Wildhirt SM, Dudek RR, Suzuki H, Pito V, Narayan KS, Bing RJ . Immunocytochemistry in the identification of nitric oxide synthase isoenzymes in myocardial infarction. Cardiovasc Res 1995; 29: 526–31.
L'eEcuyer T, Allebban Z, Thomas R, Heide RV . Glutathione S-transferase overexpression protects against anthracycline-induced H9C2 cell death. Am J Physiol Heart Circ Physiol 2004; 286: 2057–64.
Isomoto S, Kawakami A, Arakaki T, Yamashita S, Yano K, Ono K . Effects of antiarrhythmic drugs on apoptotic pathways in H9C2 cardiac cells. J Pharmacol Sci 2006; 101: 318–24.
Schimmel KJ, Richel DJ, van den Brink RB, Guchelaar HJ . Cardiotoxicity of cytotoxic drugs. Cancer Treat Rev 2004; 30: 181–91.
Walles M, Thum T, Levsen K, Brolak J . Verapamil metabolism in distinct regions of the heart and in cultures of cardiomyocytes of adult rats. Drug Metab Dispos 2001; 29: 761–8.
Saji K, Fukumoto Y, Suzuki J, Fukui S, Nawata J, Shimokawa H . Colchicine, a microtubule depolymerizing agent, inhibits myocardial apoptosis in rats. Tohoku J Exp Med 2007; 213: 139–48.
Santostasi G, Kutty R, Krishna G . Increased toxicity of anthracycline antibiotics induced by calcium entry blockers in cultured cardiomyocytes. Toxicol Appl Pharmacol 1991; 108: 140–9
Zapata-Sudo G, Trachez MM, Sudo RT, Nelson TE . Is comparative cardiotoxicity of S(−) and R(+) bupivacaine related to enantiomer-selective inhibition of L-type Ca2+ channels? Anesth Analg 2001; 92: 496–501.
Zink W, Bohl JR, Sinner B, Martin E, Graf BM . The long term myotoxic effects of bupivacaine and ropivacaine after continuous peripherial nerve blocks. Anesth Analg 2005, 101: 548–54
Burmester MD, Schluter KD, Daut J, Hanley PJ . Enantioselective actions of bupivacaine and ropivacaine on coronary vascular resistance at cardiotoxic concentrations. Anesth Analg 2005; 100: 707–12.
Cesselli D, Jakoniuk I, Berlucchi, Beltrami AP, Hintze TH, Nadal-Ginard B, et al. Oxidative stress-mediated cardiac cell death is major determinant of ventricular dysfunction and failure in dog dilated cardiomyopathy. Circ Res 2001; 89: 279–86.
Lenfant F, Lahet JJ, Courderot-Masuyer C, Freysz M, Rochette L . Lidocaine has better antioxidant potential than ropivacaine and bupivacaine: in vitro comparison in a model of human erythrocytes submitted to an oxidative stress. Biomed Pharmacother 2004; 58: 248–54.
Lenfant F, Lahet JJ, Vergely C, Volot F, Freysz M, Rochette L . Lidocaine inhibits potassium efflux and hemolysis in erythrocytes during oxidative stress in vitro. Gen Pharmacol 2000; 34: 193–9.
Collins AL . Comet assay – principles, applications, and limitations. Methods Mol Biol 2002; 203: 163–77.
Olive PL, Frazer G, Banath JP . Radiation – induced apoptosis measured in TK6 human B lymphoblast cells using the comet assay. Radiat Res 1993; 136: 130–6.
Singh KK, Russel J, Sigala B, Zhang Y, Williams J, Keshav KF . Mitochondrial DNA determines the cellular response to cancer therapeutic agents. Oncogene 1999; 18: 6641–6.
Liao X, Liu JM, Du L, Tang A, Shang Y, Wang SQ, et al. Nitric oxide signalling in stretch-induced apoptosis of neonatal rat cardiomyocytes. FASEB J 2006; 20: 1883–5.
Park CJ, Park SA, Yoon TG, Lee SJ, Yum KW, Kim HJ . Bupivacaine induces apoptosis via ROS in the Schwann cell line. J Dent Res 2005; 84: 852–7.
Conti G, Scarpini E, Rostami A, Livraghi S, Clerici R, Piccio L, et al. Schwann cell apoptosis during cell-mediated demyelination, Ann NY Acad Sci 1999; 883: 518–9.
Feinstein D, Murphy P, Gator A, Ziemann-Gimmel P, Weinberg G . Metabolic rescue from local anesthetic-induced cytotoxicity. Anesth 2002; 96: A973.
Vander Heide RS, L'Ecuyer TJ . Molecular basis of anthracycline induced cardiotoxicity. Heart Metab 2007; 35: 1–4.
Bostwick DG, Meiers I, Shanks JH . Glutathione S-transferase: differential expression of alpha, mu, and pi isoenzymes in benign prostate, prostatic intraepithelial neoplasia, and prostatic adenocarcinoma. Hum Pathol 2007; 38: 1394–401.
Soh Y, Goto S, Kitajima M, Moriyama S, Kotera K, Nakayama T, et al. Nuclear localization of glutathione S-transferase pi is an evaluation factor for drug resistance in gynaecological cancers. Clin Oncol (R Coll Radiol) 2005; 17: 264–70.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kulbacka, J., Bar, J., Chwilkowska, A. et al. Oxidative modulation of marcaine and lekoptin in H9C2 rat myoblasts. Acta Pharmacol Sin 30, 184–192 (2009). https://doi.org/10.1038/aps.2008.27
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2008.27
Keywords
This article is cited by
-
Genotoxic evaluation of bupivacaine and levobupivacaine in the Drosophila wing spot test
Cytotechnology (2016)