Abstract
Purpose
The authors sought to evaluate the efficacy of recombinant tissue plasminogen activator (r-TPA) in the treatment of severe fibrinous anterior chamber reactions secondary to endophthalmitis.
Methods
Twelve patients with endophthalmitis associated with severe fibrinous anterior chamber reactions were enrolled in the study. Various degrees of posterior synechiae were noted in 10 of these patients. TPA (25 μg/0.05 cc) was injected into the anterior chamber through the limbus as an adjunctive treatment to intravitreal antibiotic injection. Efficacy of the treatment was judged by the rate of fibrinolysis, the lysis of posterior synechiae, and the size of the dilated pupil.
Results
After application of 25 μg of r-TPA, the fibrin reaction gradually resolved in 2–14 h. The median dilated pupil size in ratio 24 h after r-TPA injection was significantly larger than before r-TPA injection (0.41 vs0.60; P=0.002). The median difference in pupil size in ratio in patients with posterior synechiae larger than 180° was significantly larger than those with posterior synechiae equal or less than 180° (0.32 vs0.09; P=0.003). At 24 h after application of r-TPA, no eye had posterior synechiae.
Conclusion
Intracameral injection of r-TPA may be a safe and effective method for the treatment of significant fibrin reaction in endophthalmitis and thus facilitates vitreous and fundus examinations and vitrectomy if necessary.
Similar content being viewed by others
Introduction
The development of exuberant fibrinous exudation is a serious complication of endophthalmitis, which can obscure the fundus examination and interfere with the performance of vitrectomy. Furthermore, it may cause numerous sequelae in the anterior segment and posterior pole of the eye. These sequelae include extreme membrane formation with posterior synechiae, pupillary block, peripheral anterior synechiae, secondary angle closure glaucoma, and tractional retinal detachment.1 These fibrinous membranes are usually difficult to manage with conventional steroid therapy. Treatment of endophthalmitis with steroids should be done cautiously and with the knowledge that it takes extensive time to resolve the fibrinous membranes and that the treatment may still be unsuccessful. Recombinant tissue plasminogen activator (r-TPA) has been characterized as a relatively pure preparation of TPA, containing fewer other proteins that would induce inflammation. It is a clot-specific fibrinolytic agent. Because r-TPA activity is specific for its substance plasminogen and is greatly enhanced in the presence of fibrin, intraocular injection of r-TPA has been reported to be both effective and safe in the treatment of fibrin-related complications of ocular inflammation.2, 3, 4, 5, 6, 7, 8
In this study, we assess the efficacy and safety of intracameral r-TPA injection in the clearance of anterior chamber fibrinous membrane due to endophthalmitis, and we evaluate the difference in dilated pupil size pre- and post-r-TPA injection and the lysis of posterior synechiae.
Methods
From April 2003 to October 2005, 12 patients (12 eyes) with a severe anterior chamber fibrinous membrane-associated endophthalmitis were enrolled into this study. The inclusion criteria included anterior chamber fibrinous membrane covering the pupil or iris, invisible vitreous and fundus detail due to the fibrinous membrane, corneal oedema not too severe to interfere with anterior chamber examination by slitlamp biomicroscopy.
Detailed ophthalmological examinations were performed and recorded, including visual acuity, intraocular pressure (IOP), slitlamp biomicroscopy, dilated pupil with 10% phenylephrine and 1% tropicamide for indirect ophthalmoscopy, B scan if medium was opaque, and slitlamp photography. Our hospital Ethics Committee approved the study. Informed consent was obtained from all patients after discussion of the procedure. The procedure was performed in the operating room with the patient supine. After retrobulbar anaesthesia was induced with 2% xylocaine (lidocaine hydrochloride), the bulbar conjunctiva was prepared with 5% betadine. The eyelids were opened by lid speculum. Aqueous humor was aspirated from the anterior chamber through the limbus with an insulin syringe, and vitreous tapping was performed through the pars plana with an insulin syringe for bacteria and fungus culture. Vancomycin (1 mg/0.1 cc) and ceftazidime (2.25 mg/0.1 cc) were injected into the anterior vitreous through the pars plana. r-TPA (25 μg/0.05 cc) (actilyse 50 mg flacon; Boehringer Ingelheim, Ingelheim, Germany) was injected into the anterior chamber, having been diluted with balanced salt solution to a concentration of 50 μg/0.1 ml and stored at −70°C as described previously.9
Postoperative medications included fortified 1.3% gentamicin eye drops every 30 min, 5% cefazolin eye drops every 30 min, 1% pre-forte four times daily, and 1% atropine eye ointment once daily.
Slitlamp biomicroscopy examination was performed 2, 4, and 6 h and then daily after the administration of the r-TPA; the IOP was measured daily. The degree of posterior synechiae was evaluated using slitlamp biomicroscopy and recorded as 0°, 90° (>0° and ⩽90°), 180° (>90° and ⩽180°), 270° (>180° and ⩽270°) and 360° (>270°). Pupil size was measured as the ratio of pupil to cornea diameter in the horizontal meridian based on photographs obtained before and 1 day after the administration of the r-TPA. Difference in pupil size was defined as pupil size in ratio 1 day after the administration of the r-TPA minus pupil size in ratio before the administration of the r-TPA.
The statistical evaluation of the difference in dilated pupil size between pre- and post-r-TPA injection was performed by means of the Wilcoxon test. The statistical analysis of the difference in pupil size in ratio between with and without posterior synechiae group and posterior synechiae >180° group and ⩽180° group was carried out with the Mann–Whitney test.
Results
In this study, 12 eyes in 12 patients (eight females and four males) with endophthalmitis following cataract surgery developed a severe fibrinous membrane in the anterior chamber. The mean age of the patients was 73.8±7.9 years (range: 62–85 years). Various degrees of posterior synechiae were noted in 10 of these patients (Table 1). After application of 25 μg of r-TPA, the fibrin reaction gradually resolved in all cases. The time to complete fibrinolysis was 2–14 h (mean: 5.2±4.0 h). In only two cases, did it take more than 6 h to achieve complete fibrinolysis, 14 and 12 h, respectively. The vitreous opacity can be evaluated by slitlamp biomicroscopy after fibrinolysis.
The median pupil size in ratio at 24 h after r-TPA injection was significantly larger than before injection (0.41 vs 0.60; P=0.002; Table 1). A plot of pre- and postinjection pupil size in ratio demonstrated that all eyes experienced pupil enlargement 24 h after r-TPA injection (Figure 1). The median difference in pupil size in ratio was more remarkable in patients with posterior synechiae than in patients without posterior synechiae (0.28 vs 0.07; P=0.015). Eyes were divided into two groups according to the degree of synechiae: synechiae >180° group and synechiae ⩽180° group. The median difference in pupil size in ratio in patients with posterior synechiae >180° was significantly larger than in patients with posterior synechiae less than 180° (0.32 vs 0.09; P=0.003; Figure 2). After application of 25 μg of r-TPA, the posterior synechiae gradually resolved from 2 to 24 h in all 10 cases with posterior synechiae. At 24 h after application of r-TPA, no eye had posterior synechiae.
Ten patients underwent pas plana vitrectomy. During the operation, no fibrin exudates in the anterior chamber were noted in any cases, and pupil size was large enough to perform vitrectomy. Anterior chamber lavage to remove anterior chamber hyphaema before vitrectomy was needed in case 2 only. No anterior chamber manipulation was necessary in any other cases.
Four patients developed mild complications after r-TPA injection, including three cases (case 6, case 7, and case 9) of transient increased IOP, which was subsequently controlled by short-term antiglaucoma treatment, and one case (case 2) of hyphaema, which was minimal and easily removed with anterior chamber lavage during pars plana vitrectomy.
Case report
Case 9
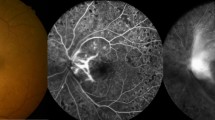
A 69-year-old woman underwent uncomplicated phacoemulsification and posterior chamber intraocular lens implantation in the left eye. On postoperative day 11, the patient presented with blurring vision in her left eye and painful red eye. Endophthalmitis was suspected and she was treated with intravitreal vancomycin, ceftazidime, and dexamethasone at a local hospital. Her condition did not improve, and she was referred to our department. At her first visit to our clinic, vision was 6/12 in the right eye and light perception only in the left eye. The right eye was unremarkable except for cataract. Slitlamp examination disclosed diffuse corneal oedema, anterior chamber cell (+++), exudative membrane over the pupil, and a posterior chamber intraocular lens with 270° posterior synechiae in the left eye (Figure 3a). The fundus was not visible in the left eye and a B scan showed vitreous opacity and a flat retina. Acute postoperative endophthalmitis was diagnosed. She was treated with intravitreal injections of vancomycin 1 mg/0.1 cc, ceftazidime 2.25 mg/0.1 cc, and dexamethasone 0.32 mg/0.08 cc after anterior chamber aspiration and vitreous tapping. Then, 25 μg/0.05 cc of r-TPA was injected into the anterior chamber through the limbus with a 30-gauge needle. At 2 h following r-TPA injection, the fibrin had almost completely disappeared. After 6 h, the fibrin and posterior synechiae had completely disappeared and the pupil could be dilated from 0.36 to 0.68 in ratio size (Figure 3b). One day after injection, the IOP was increased to 28 mm Hg and controlled with topical antiglaucoma eye drops. After 4 days, a pars plana vitrectomy was performed to clear the severe vitreous opacity. During the operation, the pupil could be almost fully dilated and the anterior chamber was clear enough to view the posterior segment. The culture from a vitreous specimen showed Staphylococcus haemolyticus. At 8 months after operation, the patient's visual acuity was 6/12 with a normal appearing anterior segment on slitlamp examination. There was no posterior segment inflammation and IOP was 16 mm Hg without any medication.
Discussion
Endophthalmitis is an uncommon but serious postoperative complication, requiring prompt diagnosis and timely treatment. The symptoms include red eye, pain, discharge, and blurring vision. The signs include decreased visual acuity, conjunctival congestion, corneal oedema, anterior chamber cell flare, and vitritis.10 Hypopyon and fibrinous membrane have also been noted in some severe cases. The pathogenesis of the fibrin response secondary to the infection is unclear, but it appears to involve both breakdown of the blood–ocular barrier by inflammation and dysfunction of the coagulation and fibrinolytic pathway.11 These extensive fibrinous membranes significantly increase the morbidity associated with the infectious process. They may result in posterior synechiae, pupillary block, peripheral anterior synechiae, and secondary angle closure glaucoma. An extensive fibrinous membrane with posterior synechiae makes the pupil difficult to dilate, which interferes with fundus examination and following vitrectomy, if necessary. Treatment of endophthalmitis with steroids should be done carefully. Steroid treatment usually takes several weeks and may not ultimately be effective. Therefore, active fibrinolysis may be a more potent therapeutic option in these urgent cases.
r-TPA has been described as a relatively safe agent, which causes less inflammatory reaction and systemic bleeding tendency compared with other fibrinolytic agents.7 Intraocular injection of r-TPA had been reported to be effective in the treatment of fibrinous reaction after cataract surgery,12 vitrectomy,4, 6 penetrating keratoplasty,13 glaucoma surgery,14 and traumatic hyphaema.15 There have, however, been only a few published series in which patients with endophthalmitis were treated with r-TPA. We treated 12 patients with severe fibrin reactions secondary to endophthalmitis with intracameral r-TPA injection.
Published papers about the use of r-TPA for treatment of fibrinous reactions secondary to endophthalmitis are limited. In 1991, Baziuk et al16 reported that intravitreous r-TPA does not play a beneficial role in the treatment of experimentally induced bacterial endophthalmitis. In 1993, Ryan and Mizener17 showed that fibrinolysis with intraocular r-TPA did not accelerate clearance of inflammation or decrease fibroproliferative complications in an animal model of endophthalmitis. The role of intracameral injection of r-TPA in patients with endophthalmitis has not yet been determined. Erol et al18 reported on two patients with severe anterior chamber fibrinous membrane secondary to endophthalmitis in whom they used intracameral r-TPA (25 μg/0.1 cc) to clear the fibrinous membrane. Complete fibrinolysis was observed in both cases. The time for clearance of the fibrin membranes was 2 and 4.5 h, respectively. Damji et al19 reported on two patients with dense fibrinous membrane over the pupils and intraocular lens after intravitreal antibiotics injection for treatment of endophthalmitis. They performed intracameral injection of r-TPA (25 μg/0.1 cc) to clear the fibrinous membrane. At 1 h following r-TPA injection, the fibrin had almost completely disappeared in both patients. Pupillary block and peripheral anterior synechiae had also almost completely resolved in one patient. In 2006, Riaz et al20 reported using r-TPA for clot dissolution following endophthalmitis in one patient. The patient had complete clot dissolution within 2 h without any complications.
To our knowledge, this study is the largest series in which r-TPA was used as an adjuvant treatment in endophthalmitis associated with severe anterior chamber exudates. The efficacy of intracameral 25 μg r-TPA was assessed with regard to fibrinolysis, lysis of posterior synechiae, and dilated pupil size in ratio. We found complete fibrinolysis was accomplished within 14 h after application of r-TPA. Actually, complete fibrinolysis was accomplished within 6 h in 10 cases. In only two cases, did it take more than 6 h to achieve complete fibrinolysis. We believe the exact time to complete fibrinolysis was less than the recorded time in the two remaining cases, because we did not check so frequently after 6 h. Our results demonstrating that intracameral r-TPA is highly effective for fibrinolysis in endophthalmitis cases are in accord with previous reports.18, 19, 20
Posterior synechiae in 10 of 10 patients disappeared within 24 h after intracameral r-TPA injection. These results are compatible with those in the 1998 study by Heiligenhaus et al.7 Heiligenhaus et al7 observed that the frequencies of synechiae and capsule fibrosis were reduced by r-TPA injection; however, Erol et al18 reported that posterior synechiae in three of their cases did not disappear despite the fact that fibrin clearance occurred after r-TPA injection. The rapid disappearance of posterior synechiae in our cases might be because they were treated so quickly, within days, after formation. Because the endophthalmitis in our patients was controlled, no recurrent fibrin formation or posterior synechia was found during follow-up.
Our results showed that the median pupil size in ratio 24 h after r-TPA injection was significantly larger than before injection. The difference in pupil size ratio was more remarkable in cases in which the posterior synechiae were larger than 180°. Our results also showed that intracameral r-TPA is an effective adjuvant in dilation of the pupil, which facilitated observation of the fundus and eliminated anterior chamber manipulation during vitrectomy. Surgical removal of an anterior chamber fibrinous membrane before pars plana vitrectomy may cause complications such as miosis, iris bleeding, and corneal endothelium damage. Such complications make the subsequent vitrectomy more difficult to perform. To prevent these complications, minimal or no anterior segment manipulation should be done. In our study, 10 patients underwent pars plana vitrectomy. During the operations, no fibrin exudates in anterior chamber were noted and pupil size was large enough to perform vitrectomy in all cases. No anterior chamber manipulation was done in any case except case 2. Anterior chamber lavage to remove anterior chamber hyphaema was performed before vitrectomy in case 2. To the best of our knowledge, until now, there have been no reports in the literature on such pupil size change.
After complete fibrinolysis, the vitreous opacity could be evaluated. Pars plana vitrectomy was performed on 10 cases due to an absent red reflex. Four of these patients had diabetes. All of these patients had final best-corrected visual acuity ⩾3/60. Seven of these patients (70%) had final best-corrected visual acuity ⩾6/30. Only two of these patients (20%) had final best-corrected visual acuity ⩾6/12. Compared with the Endophthalmitis Vitrectomy Study,21 this group not only had less proportion with poor vision, but also had less patients achieve good vision. Due to our limited number of cases, our results just revealed the adjunctive role of r-TPA in treating endophthalmitis. A large, prospective, randomized control study is necessary to establish the absolute benefit of vitrectomy in these patients.
During the follow-up period, there were four patients who suffered mild complications, including minimal hyphaema in case 2 and transient high IOP in cases 6, 7, and 9. Other reported complications of r-TPA injection, including vitreous haemorrhage, intraocular haemorrhage, recurrent fibrin formation, and retinal toxicity,3, 4, 5, 6 were not observed in our patients. However, this is a study on just 12 subjects; it may be limited to pick up rare but potential side effects. In this study, we did not evaluate the reported complications involving sterile endophthalmitis and corneal oedema, as our focus was on endophthalmitis. Before treatment, all cases had corneal oedema and 10 cases had hypopyon. One day after treatment, no case had increased the height of hypopyon or the degree of cell number in anterior chamber. The cornea was clear up after the infection was controlled in all cases.
The optimal dose of r-TPA for intraocular use is still controversial. Retinal toxicity has been described in rabbit eyes at doses of 25 μg and larger.22 The reported effective dosage of r-TPA has ranged from 3 to 25 μg.5, 23 Boldt et al23 reported that the minimum effective dose of r-TPA for fibrinolysis in eyes with severe postvitrectomy fibrin was between 1.5 and 3 μg. Our results show intracameral injection of 25 μg of r-TPA for these patients is promising and safe in the treatment of severe fibrin in endophthalmitis. The optimal dosage of r-TPA should be further established.
In conclusion, in this small case series, intracameral injection of 25 μg/0.05 ml r-TPA seemed to be safely and effectively given for treatment of significant fibrin reaction in the patient with acute postoperative endophthalmitis. Furthermore, it is recommended for use in those patients who have severe fibrin in the anterior chamber associated with small pupil size and posterior synechiae more than 180°. Due to our limited number of cases, a large, prospective, randomized control study is necessary to establish the absolute benefit of intracameral r-TPA injection and the optimal dose in these patients.
References
Lewis H, Han D, Williams GA . Management of fibrin pupillary-block glaucoma after pars plana vitrectomy with intravitreal gas injection. Am J Ophthalmol 1987; 103: 180–182.
Kim MH, Koo TH, Sah WJ, Chung SM . Treatment of total hyphema with relatively low-dose tissue plasminogen activator. Ophthalmic Surg Lasers 1998; 29: 762–766.
Lundy DC, Sidoti P, Winarko T, Minckler D, Heuer DK . Intracameral tissue plasminogen activator after glaucoma surgery. Indications, effectiveness, and complications. Ophthalmology 1996; 103: 274–282.
Jaffe GJ, Lewis H, Han DP, Williams GA, Abrams GW . Treatment of postvitrectomy fibrin pupillary block with tissue plasminogen activator. Am J Ophthalmol 1989; 108: 170–175.
Williams GA, Lambrou FH, Jaffe GA, Snyder RW, Green GD, Devenyi RG et al. Treatment of postvitrectomy fibrin formation with intraocular tissue plasminogen activator. Arch Ophthalmol 1988; 106: 1055–1058.
Jaffe GJ, Abrams GW, Williams GA, Han DP . Tissue plasminogen activator for postvitrectomy fibrin formation. Ophthalmology 1990; 97: 184–189.
Heiligenhaus A, Steinmetz B, Lapuente R, Krallmann P, Althaus C, Steinkamp WK et al. Recombinant tissue plasminogen activator in cases with fibrin formation after cataract surgery: a prospective randomised multicentre study. Br J Ophthalmol 1998; 82: 810–815.
Siatiri H, Beheshtnezhad AH, Asghari H, Siatiri N, Moghimi S, Piri N . Intracameral tissue plasminogen activator to prevent severe fibrinous effusion after congenital cataract surgery. Br J Ophthalmol 2005; 89: 1458–1461.
Jaffe GJ, Green GD, Abrams GW . Stability of recombinant tissue plasminogen activator. Am J Ophthalmol 1989; 108: 90–91.
Kresloff MS, Castellarin AA, Zarbin MA . Endophthalmitis. Surv Ophthalmol 1998; 43: 193–224.
Mehta JS, Adams GG . Recombinant tissue plasminogen activator following paediatric cataract surgery. Br J Ophthalmol 2000; 84: 983–986.
Wedrich A, Menapace R, Ries E, Polzer I . Intracameral tissue plasminogen activator to treat severe fibrinous effusion after cataract surgery. J Cataract Refract Surg 1997; 23: 873–877.
Snyder RW, Lambrou FH, Williams GA . Intraocular fibrinolysis with recombinant human tissue plasminogen activator. Experimental treatment in a rabbit model. Arch Ophthalmol 1987; 105: 1277–1280.
Koerner F, Boehnke M . Clinical use of recombinant plasminogen activator for intraocular fibrinolysis. Ger J Ophthalmol 1992; 1: 354–360.
Laatikainen L, Mattila J . The use of tissue plasminogen activator in post-traumatic total hyphaema. Graefes Arch Clin Exp Ophthalmol 1996; 234: 67–68.
Baziuk N, Fang T, Peyman GA, Gremillion Jr CM . Intravitreal recombinant tissue plasminogen activator in the treatment of experimentally induced bacterial endophthalmitis. Int Ophthalmol 1991; 15: 79–86.
Ryan EH, Mizener JB . Tissue plasminogen activator and Staphylococcus epidermidis endophthalmitis. Arch Ophthalmol 1993; 111: 1117–1122.
Erol N, Ozer A, Topbas S, Yildirim N, Yurdakul S . Treatment of intracameral fibrinous membranes with tissue plasminogen activator. Ophthalmic Surg Lasers Imaging 2003; 34: 451–456.
Damji KF, O'Connor MD, Hill V . Tissue plasminogen activator for treatment of fibrin in endophthalmitis. Can J Ophthalmol 2001; 36: 269–271.
Riaz Y, Mehta JS, Femando A, Ferguson V . Recombinant tissue plasminogen activator (r-TPA) in fibrin dissolution due to postoperative endophthalmitis. Ann Acad Med Singapore 2006; 35: 723–725.
The Endophthalmitis Vitrectomy Study Group. Results of the Endophthalmitis Vitrectomy Study: a randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Arch Ophthalmol 1995; 113: 1479–1496.
Irvine WD, Johnson MW, Hernandez E, Olsen KR . Retinal toxicity of human tissue plasminogen activator in vitrectomized rabbit eyes. Arch Ophthalmol 1991; 109: 718–722.
Boldt HC, Abrams GW, Murray TG, Han DP, Mieler WF . The lowest effective dose of tissue plasminogen activator for fibrinolysis of postvitrectomy fibrin. Retina 1992; 12: S75–S79.
Acknowledgements
This study was supported by Grant VGHKS-92-65 from Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan. We thank Professor Luo-Ping Ger for her statistical counseling.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wu, TT., Wang, HH. Intracameral recombinant tissue plasminogen activator for the treatment of severe fibrin reaction in endophthalmitis. Eye 23, 101–107 (2009). https://doi.org/10.1038/sj.eye.6702984
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702984
Keywords
This article is cited by
-
Rebound iritis with a well-circumscribed anterior chamber fibrin mass after uncomplicated cataract surgery
Journal of Ophthalmic Inflammation and Infection (2021)
-
Intracameral tissue plasminogen activator in trabeculectomy: a 1-year prospective, randomized, controlled study
International Ophthalmology (2020)
-
Very late-onset flap margin corneal ulcer following laser in situ keratomileusis
International Ophthalmology (2019)