Abstract
The Low-Pressure Glaucoma Treatment Study is a double-masked, randomized trial comparing the visual outcomes of 190 low-pressure glaucoma patients randomized to intraocular pressure reduction with brimonidine tartrate or timolol maleate. Baseline characteristics of participants are compared to published studies.
Similar content being viewed by others
Introduction
Open-angle glaucoma is a family of disorders characterized by a slow progressive neurodegeneration of retinal ganglion cells and their axons1 with degenerative changes along the retinogeniculocortical pathway.2 Normal-tension glaucoma is a type of open-angle glaucoma that occurs with an untreated intraocular pressure (IOP) in the statistically normal range, usually ⩽21 mmHg. My personal preference is to use the term ‘low-pressure glaucoma’ (LPG), rather than ‘normal-tension glaucoma’. Use of the term ‘normal’ in this condition relates to statistically normal, not pathologically normal. It is awkward to use ‘normal’ when discussing the disease with a patient who is worried about blindness, and the only ‘tension’ involved is that experienced by the patient and the ophthalmologist in facing this disease.
Low-pressure and high-pressure open-angle glaucoma are a continuum and cannot be separated by a single IOP level. The degree of IOP is the most important risk responsible for disease progression and the only factor amenable for change. Several clinical trials have confirmed the value of decreasing IOP in patients with ocular hypertension,3, 4 high-pressure open-angle glaucoma,5, 6, 7 and LPG.7, 8, 9 However, decreasing IOP does not necessarily halt the glaucomatous process.
Basic biological research over the past decade has been directed to mechanisms and treatments that underlie chronic neurodegenerative disorders, including glaucoma,10 such as the steps of neuronal apoptosis including responses to excitatory neurotransmitters, regulation of ion channel activities, and modulation of signal transduction pathways.
Neuroprotection is a therapeutic strategy directed at keeping retinal ganglion cells alive and functionally connected to their targets in the brain. α2-Adrenergic agonists have a neuroprotective effect in animal models of focal cerebral ischaemia.11 Systemic administration of brimonidine (Alphagan, Allergan Inc., Irvine, CA, USA), a selective α2-adrenergic agonist, has been shown to protect the optic nerve and retinal ganglion cells from secondary degeneration following a partial crush injury to the adult rat optic nerve12 and to protect retinal ganglion cells in the ocular hypertensive rat model.13 Possible molecular mechanisms for brimonidine's neuroprotective effect relates to upregulation of neuronal survival factors, brain-derived neurotrophic factor mRNA expression in retinal ganglion cells,14 and basic fibroblast growth factor mRNA expression in the retina.15
Neuroprotective activity must be demonstrated in randomized controlled clinical trials, which was the purpose of the Low-pressure Glaucoma Treatment Study (LoGTS). This paper reviews LoGTS study design and descriptions of the baseline patient characteristics.16
Study design
LoGTS is a multicentre, prospective, randomized, double-masked, two-arm parallel group study comparing the efficacy of brimonidine 0.2% vs timolol 0.5% to alter the course of LPG as measured by the rate of visual field progression. Study investigators are listed in Table 1.Subjects included 190 men and women, ⩾30 years of age, with previously diagnosed LPG in at least one eye and untreated IOP of ⩽21 mmHg on a diurnal pressure curve on day zero. The diagnosis of LPG required open iridocorneal angles by gonioscopy and glaucomatous visual field defects in at least one eye on Humphrey 24-2 full-threshold standard automatic perimetry. At least two visual field examinations with acceptable reliability standards were required within the prior 6 months. Vision of at least 20/40 was also required.
Pertinent exclusion criteria included a history of treated or untreated IOP greater than 21 mmHg and an untreated IOP greater than 21 mmHg during a pre-randomization diurnal curve. Patients with advanced glaucoma (mean deviation>15 decibels) were excluded, as well as those with evidence of exfoliation, pigment dispersion, or prior filtration surgery.
The primary end point was visual field. Patients were examined at 1 and 4 months after initiation of treatment randomization and every 4 months thereafter. Baseline visual field was defined as the average of two pre-randomization examinations. Optic discs were evaluated by physician assessment every 4 months and by photographs at baseline and every year thereafter. Photographs were evaluated at the Optic Disc Reading Center. Central corneal thickness (CCT) was measured.
Age
The average patient age was 64.9±10.7 years (mean±SD). Twenty-two patients (11.6%) were younger than 50 years of age. The Beaver Dam Eye Study17 had shown earlier that the prevalence of LPG increased with age, from 0.2% in the 43–54 age group to 1.6% in the over 75 age group, with 63.6% of the patients older than 64 years. In the LoGTS, only 54.2% of patients were older than 64, a smaller percentage than the Beaver Dam Study. This may relate to improved clinical evaluation of the optic nerve. The incidence of LPG at younger ages will surely increase as more attention is placed on evaluation of the optic nerve during routine eye examinations.
Sex
There were more women (n=113; 59.5%) than men (n=77; 40.5%; P=0.0003). Earlier reports on gender distribution of LPG have reported greater frequency in women,18, 19 greater frequency in men,20 or an equal distribution between the sexes.17
Family history
In the LoGTS, 30% of the patients had a family history of chronic open-angle glaucoma, and a 4% had a family history of LPG.
Migraine
Phelps et al21 reported a 37% incidence of migraine in LPG patients, higher than in normal subjects or COAG patients by about 22%. A history of migraine headaches was reported in nine participants (4.7%), a finding similar to earlier findings in the Beaver Dam Study17 and a study by Lewis et al.22
Vasospasm
Although previous reports have cited a high occurrence of functional peripheral vasospasm (up to about 65%),20, 23 only 16 LoGTS participants (8.4%) reported a history compatible with Raynaud's phenomenon.
Visual field loss
Visual field defects in both eyes were present in 137 patients (72.1%); unilateral defects were present in 53 patients (27.9%) at baseline, with the left eye more commonly involved (56.6%). This was similar to the 25% occurrence of unilateral field loss (64% left eye) in LPG reported by Poinoosawmy et al.24
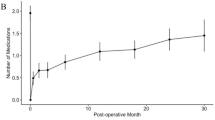
The unilateral field loss patients were younger than those with bilateral defects, with the proportion of unilateral cases decreasing with increasing age (Figure 1). The younger age of these patients may relate to earlier detection of optic nerve damage in those with a normal IOP.
Cupping
As expected, cup-to-disc ratios in the unilateral field loss participants were higher (P<0.0001) in the eyes with field loss (0.75±0.12) than in the fellow eyes without visual field damage (0.60±0.17).
Optic disc haemorrhage
Evaluation of baseline optic disc photographs was performed by three observers for the presence of a disc haemorrhage defined as adjacent to or touching the disc edge and within the rim tissue. A haemorrhage was present in 29 patients (32 eyes).
IOP
The mean of the four baseline diurnal readings of nontreated IOP was equal in both eyes (Table 2). There was no difference between eyes in the mean nontreated diurnal IOP of the 137 bilateral field loss patients. There were 18 bilateral patients who had some asymmetry in pressure. Nontreated diurnal IOP was similar between the eyes of the 53 unilateral field loss subjects. Most eyes were equal in IOP by 1 mmHg, although there were 12 subjects who had higher pressure in the field loss eye and eight subjects who had lower pressure in the field loss eye.
Corneal thickness
CCT (microns) was measured in 168 of 171 phakic patients. Mean CCT was 543±35 with a range from 435 to 655. CCT was less than 500 in 15 patients (30 eyes; 8.9%) and more than 600 in 11 patients (22 eyes; 7.1%). There was no statistically significant difference in CCT between the bilateral field loss patients and the unilateral field loss patients. The impact of corneal thickness obviously is that thin CCTs can underestimate the true IOP and can classify a patient inaccurately as having LPG (IOP less than 22 mmHg in our study). Shah et al25 have reported low mean CCTs in 52 of 514 patients with low-pressure glaucoma. The LoGTS does not confirm an excess of thin corneas in LPG patients.
Summary
The baseline characteristics of the large group of LPG patients enrolled in the prospective LoGTS clinical trial provide useful information on IOP, visual field loss, and optic nerve haemorrhages. These data can help in formulating better treatment paradigms for open-angle glaucoma patients with relatively low IOPs.
References
Kerrigan-Baumrind LA, Quigley HA, Pease ME, Kerrigan DF, Mitchell RS . Number of ganglion cells in glaucoma eyes compared with threshold visual field tests in the same persons. Invest Ophthalmol Vis Sci 2000; 41: 741–748.
Yücel YH, Zhang Q, Weinreb RN, Kaufman PL, Gupta N . Effects of retinal ganglion cell loss on magno-, parvo-, and koniocellular pathways in the lateral gengiculate nucleus and visual cortex in glaucoma. Prog Retin Eye Res 2003; 22: 465–481.
Kass MA, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JL, Miller JP . The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol 2002; 120: 701–713.
Gordon MO, Beiser JA, Brandt JD, Heuer DK, Higginbotham EJ, Johnson CA . The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol 2002; 120: 714–720.
The AIGS Investigators. The Advanced Glaucoma Intervention Study (AGIS). 7: the relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol 2000; 130: 429–440.
Lichter PR, Musch DC, Gillespie BW, Guire KE, Janz NK, Wren PA et al. Interim clinical outcomes in the Collaborative Initial Treatment Study comparing initial treatment randomized to medications or surgery. Ophthalmology 2001; 108: 1943–1953.
Heijl A, Leske MC, Bengtsson B, Hyman L, Bengtsson B, Hussein M . Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol 2002; 120: 1268–1279.
Collaborative Normal-tension Study Group. Comparison of glaucomatous progression between untreated patients with normal-tension glaucoma and patients with therapeutically reduced intraocular pressures. Am J Ophthalmol 1998; 126: 487–497.
Collaborative Normal-tension Study Group. The effectiveness of intraocular pressure reduction in the treatment of normal-tension glaucoma. Am J Ophthalmol 1998; 126: 498–505.
Weinreb RN, Levin LA . Is neuroprotection a viable therapy for glaucoma? Arch Ophthalmol 1999; 117: 1540–1544.
Maier C, Steinberg GK, Sun GH, Zhi GT, Maze M . Neuroprotection by the alpha-2 adrenoreceptor agonist dexmedetomidine in a focal model of cerebral ischemia. Anesthesiology 1993; 79: 306–312.
Yoles E, Wheeler LA, Schwartz M . Alpha2-adrenoreceptor agonists are neuroprotective in a rat model of optic nerve degeneration. Invest Ophthalmol Vis Sci 1999; 40: 65–73.
WoldeMussie E, Ruiz G, Wijono M, Wheeler LA . Neuroprotection of retinal ganglion cells by brimonidine in rats with laser-induced chronic ocular hypertension. Invest Ophthalmol Vis Sci 2001; 42: 2849–2855.
Gao H, Qiao X, Cantor LB, WuDunn D . Up-regulation of brain-derived neurotrophic factor expression by brimonidine in rat retinal ganglion cells. Arch Ophthalmol 2002; 120: 797–803.
Lai RK, Chun T, Hasson D, Lee S, Mehrbod F, Wheller L . Alpha-2 adrenoceptor agonist protects retinal function after acute retinal ischemic injury in the rat. Vis Neurosci 2002; 19: 175–185.
Krupin T, Liebmann JM, Greenfield DS, Rosenberg LF, Ritch R, Yang JW . The Low-pressure Glaucoma Treatment Study (LoGTS): study design and baseline characteristics of enrolled patients. Ophthalmology 2005; 112: 376–385.
Klein BE, Klein R, Sponsel WE, Franke T, Cantor LB, Martone J et al. Prevalence of glaucoma. The Beaver Dam Eye Study. Ophthalmology 1992; 99: 1499–1504.
Chumbley LC, Brubaker RF . Low-tension glaucoma. Am J Ophthalmol 1976; 81: 761–767.
Goldberg I, Hollows FC, Kass MA, Becker B . Systemic factors in patients with low-tension glaucoma. Br J Ophthalmol 1981; 65: 56–62.
Drance SM, Sweeney VP, Morgan RW, Feldman F . Studies of factors involved in the production of low tension glaucoma. Arch Ophthalmol 1973; 89: 457–465.
Phelps CD, Corbett JJ . Migraine and low-tension glaucoma. A case–control study. Invest Ophthalmol Vis Sci 1985; 26: 1105–1108.
Lewis RA, Vijayan N, Watson C, Keltner J, Johnson CA . Visual field loss in migraine. Ophthalmology 1989; 96: 321–326.
Gasser P, Flammer J . Influences of vasospasm on visual function. Doc Ophthalmol 1987; 66: 3–18.
Poinoosawmy D, Fontana L, Wu JX, Bunce CV, Hitchings RA . Frequency of asymmetric visual field defects in normal-tension and high-tension glaucoma. Ophthalmology 1998; 105: 988–991.
Shaw S, Chatterjee A, Mathai M, Kelly SP, Kwartz J, Henson D et al. Relationship between corneal thickness and measured intraocular pressure in a general ophthalmology clinic. Ophthalmology 1999; 106: 2154–2160.
Acknowledgements
This study was supported by an unrestricted grant to the Low-pressure Glaucoma Study Group from Allergan Inc., Irvine, CA, USA and the Chicago Center for Vision Research, Chicago, IL, USA. The author has no financial interests in the drugs or devices described in this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Krupin, T. A clinical trial studying neuroprotection in low-pressure glaucoma. Eye 21 (Suppl 1), S51–S54 (2007). https://doi.org/10.1038/sj.eye.6702890
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702890
Keywords
This article is cited by
-
The Japan Glaucoma Society guidelines for glaucoma 5th edition
Japanese Journal of Ophthalmology (2023)
-
Neurodegeneration in Alzheimer’s disease and glaucoma: overlaps and missing links
Eye (2020)