Abstract
Objective
To compare the retrobulbar haemodynamic parameters in the ophthalmic artery (OA) and short posterior ciliary arteries (SPCA) in pseudoexfoliative and primary open-angle glaucoma patients.
Subjects and methods
fourty-three eyes from 43 patients with pseudoexfoliative glaucoma (PXE) and 31 eyes from 31 patients with primary open-angle glaucoma (POAG) who met the inclusion/exclusion criteria were included in this prospective cross-sectional study. Colour Doppler imaging measurements, peak systolic velocity (PSV), and end-diastolic velocity (EDV) were assessed in the OA and posterior ciliary arteries (PCA). Pourcelot resistivity indices (RI) were calculated. Visual function was assessed using the 24-2 Swedish Interactive Threshold Algorithm (SITA). The main outcomes of the study were PSV, EDV, and RI in the OA and SPCA.
Results
In POAG patients, PSV and EDV were significantly lower in the OA, P=0.003 and P<0.001 respectively, and in the PCA, P=0.003 and P<0.001 respectively, when compared with the PXE group. The RI was significantly higher, P<0.001, in both vessels, in the POAG group.
Conclusion
The results of this study have found reduced PSV and EDV and increased RI in the retrobulbar vessels of POAG patients when compared with PXE patients.
Similar content being viewed by others
Introduction
Although elevated intraocular pressure (IOP) has been identified as a major risk factor for glaucoma progression,1, 2, 3 there is also increasing evidence that disturbed ocular blood flow (OBF) is a primary and independent risk factor for glaucoma progression.4, 5, 6
However, the question of whether the impact of ocular blood flow is similar, in the different types of glaucoma, remains.
Many different studies, using different types of instruments, suggested that on average ocular blood flow (OBF) is decreased in some glaucoma patients, especially in normal-tension glaucoma (NTG) and in primary open-angle glaucoma (POAG) patients with progressive visual field damage.6, 7, 8
Pseudoexfoliation syndrome is an age-related disorder of the extracellular matrix characterized by production and progressive accumulation of small, white deposits of a fibrillar extracellular material in many ocular and extraocular tissues.
The prevalence of pseudoexfoliation syndrome in POAG populations is much higher than in age-matched nonglaucomatous ones.
Several blood flow disturbances have been reported in patients with pseudoexfoliative glaucoma (PXE).9, 10 However, another study did not find differences between eyes with exfoliative glaucoma and normal controls.11
Our aim was to compare the value of colour Doppler imaging (CDI) measurements, peak systolic velocity (PSV), end–diastolic velocity (EDV), and Pourcelot resistivity indices (RI) in the ophthalmic artery (OA) and posterior ciliary arteries (PCA) between patients with PXE and patients with primary POAG.
Subjects and methods
This prospective cross-sectional study included 43 eyes of 43 patients with PXE and 31 eyes of 31 patients with POAG examined during the period from January 2003 to April 2004 in our clinic.
The study was approved by the local ethic committee. All patients were included in this study during the initial clinical open-angle glaucoma (OAG) diagnosis and had never previously been treated for glaucoma. The Doppler measurements were performed by the same experienced observer who was masked to the clinical diagnosis. All patients were fully informed about the details of the study protocol. Written informed consent was obtained from all subjects at the beginning of the study in accordance with the Declaration of Helsinki principles.
Each subject underwent a standard ophthalmic examination, including review of medical history, best-corrected visual acuity, and slit-lamp examination of the anterior segment with dilated pupils, with the aim to detect pseudoexfoliation, IOP measurement using Goldmann aplanation tonometry, gonioscopy, dilated funduscopic examination using a 78-diopter lens, stereoscopic optic disc photography, and three automated perimetry using the 24-2 Swedish Interactive Threshold Algorithm (SITA) (Carl Zeiss Meditec Inc., Dublin, CA, USA).
For glaucoma diagnosis, three visual field examinations were performed, two within 1 month of the beginning of the study.
Glaucomatous field defects were defined according to the following guidelines: as a minimum of one location in the paracentral or nasal step regions corresponding to sectors 1 or 2, or to the inferior 3 location in sector 3 of the Glaucoma Hemifield Test12 exhibiting repeatable abnormality at the P<0.5% level by pattern deviation probability analysis; or as two or more locations situating in a cluster exhibiting repeatable abnormality at the P<2% level, or lower, by pattern deviation probability analysis excluding any location in the cluster that was situated in the opposite horizontal hemifield.
Patients were included if one or both eyes exhibited mild or moderate visual field defects in terms of the classification of Hodapp et al13 and modified for the program 24-2 and the SITA standard algorithm by Litwak.14
Patients with unreliable visual field assessment (false negatives, false positives, or fixation losses exceeding 30%) were excluded.
Patients receiving systemic medications that affect IOP or systemic blood pressure were ineligible unless the patient's medication dosages were stable ⩾6 months before the screening visit.
Only one eye that fulfilled all inclusion criteria and none of the exclusion criteria was designed as the study eye; in the case where both eyes from the same patient fulfilled all inclusion criteria, and none of the exclusion criteria, the study eye was chosen randomly. Table 1 summarizes the main inclusion and exclusion criteria.
Central corneal thickness (CCT) was measured using an ultrasonic pachymeter (Corneo-gage plus 2, Sonogage, Cleveland, OH, USA). One drop of benoxinate was applied to the eye before the measurement was being taken. Six measurements were carried out and the average was recorded. All readings were performed by one observer trained in the technique.
Systolic (SBP) and diastolic (DBP) blood pressures were measured on the upper arm by sphygnomanometry. Heart rate was measured by palpation of radial pulse. These parameters were measured every 10 min and all of them remained constant in each individual throughout all examinations.
Mean arterial pressure (MAP) was calculated as DBP+ (SBP–DBP).
Ocular perfusion pressure (OPP) was calculated as MAP–IOP.
All CDI examinations were performed (model SSA-340, Toshiba Medical Systems, Tustin, CA), USA by the same experienced observer.
A 7.5 MHz vector-array transducer was applied to the closed eyelid using a coupling gel and care was taken care to avoid any pressure to the eye itself. During the examination, subjects were in supine position, with the head tilted forward at about a 30° angle. Details of the technique have been previously published.15
Measurements of the OA flow were performed approximately 10–15 mm posterior to the globe, where the echographic signals are stronger. The SPCA images were taken temporally and nasally to the optic nerve just behind the posterior pole to the eye globe. The angle between transducer and orientation of the vessels was corrected.
Peak systolic velocity (PSV) and end diastolic velocity (EDV) were measured in the OA and medial and lateral PCA. Although medial and lateral PCA were individually assessed, the mean value of both was used for the statistical analysis.
The PSV and EDV were used to calculate the Pourcelot RI according to the following equation: RI=PSV−EDV/PSV.
Statistical analysis
Sample size was calculated for an α level of 0.05, two sides, a power of 90%, and a minimal detectable difference in means of 5% between groups. For the purpose of statistical analysis, only one randomly chosen eye was included for patients with bilateral affliction.
Results are expressed as a mean (standard deviation). In order to establish an initial comparison, the Fisher exact test was used to evaluate the significance of the differences between groups in categorical variables (gender, race, diagnosis, and systemic medication). The difference between the study groups in the quantitative variables was analysed with the one-way analysis of variance (ANOVA). A P-value <0.01 was considered statistically significant. Analysis was performed using SPSS 12.0.16
Results
Demographic and clinical characteristics of the study population are shown in Table 2. No significant differences were found with respect to SBP and DBP between the two groups. However, the mean age was higher in the PXE group, P<0.001.
The MD and PSD of the visual field were significantly worse in the PXE group, P<0.001, than in the POAG group.
The IOP was significantly higher, P<0.0001, in the PXE group. There was no significant difference in CCT between the two study groups.
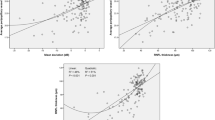
In the POAG group, the PSV and EDV were significantly lower in the OA, P=0.003 and, P<0.001, respectively, and PCA, P=0.003 and P<0.001, respectively, when compared with the PXE patients group (Table 3).
The RI was significantly higher, P<0.001, in both vessels, in the POAG group (Table 3).
Discussion
The results of this study have found reduced PSV and EDV and increased RI in the retrobulbar vessels of POAG patients when compared with PXE patients.
In POAG patients, our results are consistent with those previously reported in which retrobulbar blood flow reductions are greater in the eye with more damage.17, 18 However, our study failed to confirm this assumption in the PXE group.
There are relatively few studies that have evaluated the haemodynamic parameters of PXE patients. Our findings dissent from the findings reported by Yüksel et al,19 who reported that some haemodynamic parameters in the retrobulbar vessels were altered in patients with PXE, even with pseudoexfoliation syndrome without glaucoma.
Yüksel et al19 reported lower PSV and EDV and higher RI in both OA and PCA than our group. It may be argued that the differences between the results of the Yüksel study and our results may be due to the use of topical therapy in the Yüksel study. Although several papers have reported systemic and ocular vascular alterations in patients with pseudoexfoliation syndrome,20, 21, 22, 23 our results suggested that the OBF alterations were stronger in the POAG patients group.
The well-recognized parameter in the pathogenesis of PXE is increased IOP.24, 25 Pseudoexfoliation is also believed to be an important independent risk factor in patients with ocular hypertension.26, 27
Limitations of this study exist that warrant consideration. It is possible that the differences between the two study groups in age, IOP, and visual field damage may justify the differences in blood flow parameters between POAG and PXE patients. However, Harris et al,28 using CDI, found that in healthy subjects the ophthalmic arterial EDV decreased and RI rose with advancing age. Furthermore, Gallassi et al29 found that in normal subjects the flow velocities of all considered vessels progressively decline whereas RI values increase with advancing age. Glaucomatous eyes with uncontrolled IOP and with visual field worsening showed a statistically significant decrease in the EDV flow velocities and an increase in the resistivity index value in ciliary arteries.29 Geyer et al,30 using the Langhams pneumotonometer, reported that for younger women the pulsatile ocular blood flow (POBF) was significantly higher than for older women.
Although the PXE subjects were older, with increased IOP and more visual field damage than POAG patients, the ocular blood flow alterations were higher in the POAG patients group.
Therefore, we suggest different pathogenic mechanisms for POAG and PXE. Further research investigating the relationship between ocular blood flow – IOP and visual field deterioration, and longitudinal follow-up in the same population could be helpful in determining the relative value of each for early prediction of glaucomatous damage.
References
Gordon MO, Beiser JA, Brandt JD et al. The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol 2002; 120: 714–720.
Kass MA, Heuer DK, Higginbotham EJ et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol 2002; 120: 701–713.
Heijl A, Leske MC, Bengtsson B et al. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol 2002; 120: 1268–1279.
Galassi F, Sodi A, Ucci F et al. Ocular hemodynamics and glaucoma prognosis: a color Doppler imaging study. Arch Ophthalmol 2003; 121: 1711–1715.
Satilmis M, Orgul S, Doubler B, Flammer J . Rate of progression of glaucoma correlates with retrobulbar circulation and intraocular pressure. Am J Ophthalmol 2003; 135: 664–669.
Martinez A, Sanchez M . Predictive value of color doppler imaging in a prospective study of visual field progression in primary open-angle glaucoma. Acta Ophthalmol Scand 2005; 83: 716–723.
Flammer J, Orgül S, Costa VP, Orzalesi N, Krieglstein GK, Serra LM† et al. The impact of ocular blood flow in glaucoma. Prog Retin Eye Resea 2002; 21: 359–393.
Gherghel D, Orgul S, Gugleta K et al. Relationship between ocular perfusion pressure and retrobulbar blood flow in patients with glaucoma with progressive damage. Am J Ophthalmol 2000; 130: 597–605.
Sobour G, Finazzo C, Boles Carenini A . Monolateral Pseudoexfoliation capsulae: a study of choroidal blood flow. Acta Ophthalmol Scand 1997; 75(Suppl 224): 13–14.
Repo LP, Suhonen MT, Teräsvirta ME et al. Color Doppler imaging of the ophthalmic artery blood flow spectra of patients who have had a transient ischemic attack. Correlations with generalized iris transluminance and pseudoexfoliation syndrome. Ophthalmology 1995; 102: 1199–1205.
Mistlberger A, Gruchmann M, Hitzl W et al. Pulsatile ocular blood flow in patients with pseudoexfoliation. Spektrum der Augenheilkunde 2000; 14: 14–18.
Asman P, Heijl A . Glaucoma Hemifield Test. Automated visual field evaluation. Arch Ophthalmol 1992; 110: 812–819.
Hodapp E, Parrish II RK, Anderson DR . Clinical Decisions in Glaucoma. St Louis: Mosby, 1993.
Lalle PA . Evaluation of automated perimetry. In: Litwak A (ed). Glaucoma Handbook. Butherworth-Heinamann: Boston, 2001 pp 97–167.
Martinez A, Gonzalez F, Capeans C, Perez R, Sanchez-Salorio M . Dorzolamide effect on the ocular blood flow. Invest Ophthalmol Vis Sci 1999; 40: 1270–1275.
SPSS (computer program) Version 12.0. SPSS Inc.: Chicago, 2004.
Costa VP, Sergott RC, Spaeth GL, Moster MR, Katz LJ, Schmidt CM et al. Color Doppler imaging in glaucoma patients with asymmetric cups. J Glaucoma 1994; 3(Suppl 1): 91–97.
Nicolela MT, Drance SM, Rankin SJ, Buckley AR, Walman BE . Color Doppler imaging in patients with asymmetric glaucoma and unilateral visual field loss. Am J Ophthalmol 1996; 121: 502–510.
Yükel N, Karabas VL, Arslan A, Demirci A, Çaglar Y . Ocular hemodynamics in pseudoexfoliation syndrome and pseudoexfoliation glaucoma. Ophthalmology 2001; 108: 1043–1049.
Schlötzer-Schrehardt U, Koca MR, Naumann GOH, Volkholz H . Pseudoexfoliation syndrome. Ocular manifestations of a systemic disorder? Arch Ophthalmol 1992; 110: 1752–1756.
Naumann GOH, Schlötzer-Schrehardt U, Küchle M . Pseudoexfoliation syndrome for the comprehensive ophthalmologist. Intraocular and systemic manifestations. Ophthalmology 1998; 105: 951–968.
Hollo G, Lakatos P, Farkas K . Cold pressor test and plasma endothelin-1 concentration in primary open-angle and capsular glaucoma. J Glaucoma 1998; 7: 105–110.
Ocakoglu O, Koyluoglu N, Kayiran A, Tamcelik N, Ozkan S . Microvascular bloos flow of the optic nerve head and peripapilar retina in unilateral exfoliation syndrome. Acta Ophthalmol Scand 2004; 82: 49–53.
Ritch R . Exfoliation syndrome—The most common identifiable cause of open-angle glaucoma. J Glaucoma 1994; 3: 176–178.
Ritch R . Exfoliation syndrome and occludable angle. Trans Am Ophthalmol Soc 1994; 92: 845–944.
Mitchell P, Wang JJ, Hourihan F . The relationship between glaucoma and pseudoexfoliation: The Blue Mountains eye study. Arch Ophthalmol 1999; 117: 1319–1324.
Grodum K, Heijl A, Bengston B . Risk of glaucoma in ocular hypertension with and without pseudoexfoliation. Ophthalmology 2005; 112: 386–390.
Harris A, Harris M, Biller J, Garzocil T, Zarlty D, Ciulla TA et al. Aging affects the retrobulbar circulation differently in women and men. Arch Ophthalmol 2000; 118: 1076–1080.
Gallassi F, Nuzzaci G, Sodi A, Cappelli S, Vielmo A . Possible correlations of ocular pressure and visual field alterations in glaucoma: a study by means Color Doppler imaging. Ophthalmologica 1994; 208: 304–308.
Geyer O, Silver DM, Mathalon N, Massey AD . Gender and age affects on pulsatile ocular blood flow. Ophthal Res 2003; 35(5): 247–250.
Ferris 3rd FL, Kassoff A, Bresnick GH, Bailey I . New visual acuity charts for clinical research. Am J Ophthalmol 1982; 94: 91–96.
Acknowledgements
Financial support: This study was funded in part by research Grant no C-00-13 from the Red Tematica en Oftalmología (Thematic Network in Ophthalmology). Conflict of interest: Authors did not have any financial interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Martinez, A., Sanchez, M. Ocular haemodynamics in pseudoexfoliative and primary open-angle glaucoma. Eye 22, 515–520 (2008). https://doi.org/10.1038/sj.eye.6702676
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702676
Keywords
This article is cited by
-
Hemodynamics of the temporal and nasal short posterior ciliary arteries in pseudoexfoliation syndrome
International Ophthalmology (2021)
-
Retrobulbar hemodynamic parameters in open-angle and angle-closure glaucoma patients
Eye (2012)
-
Ocular perfusion pressure and retrobulbar haemodynamics in pseudoexfoliative glaucoma
Graefe's Archive for Clinical and Experimental Ophthalmology (2008)
-
Retrobulbar hemodynamic parameters in pseudoexfoliation syndrome and pseudoexfoliative glaucoma
Graefe's Archive for Clinical and Experimental Ophthalmology (2008)