Abstract
Background/aims
To describe the use of photodynamic therapy (PDT) in the management of symptomatic serous retinal detachment associated with choroidal naevi.
Methods
Interventional case series. The records of seven patients with choroidal naevus and associated serous retinal detachment, treated with PDT were reviewed retrospectively. Main outcome measures were Snellen visual acuity, clinical appearance, and ocular tomographic findings.
Results
All seven patients showed a reduction in the degree of serous detachment and symptomatic improvement. Five patients showed a corresponding improvement in visual acuity that persisted over a mean period of 9 months.
Conclusion
PDT appears to be effective in the management of serous retinal detachment associated with choroidal naevus.
Similar content being viewed by others
Introduction
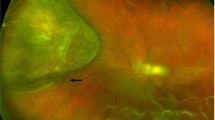
Although the majority of choroidal naevi are asymptomatic, studies have shown that approximately 11% of cases may become symptomatic.1 Symptoms may arise for a number of reasons including serous retinal detachment, photoreceptor atrophy, or sub-retinal choroidal neovascularization. Various treatments have been tried for serous retinal detachment including argon laser photocoagulation2 and transpupillary thermotherapy.3
Over the last few years, photodynamic therapy (PDT) with verteporfin has been used for a number of ophthalmic conditions both vascular, such as choroidal neovascularization secondary to age-related macular degeneration,4 centro-serous retinopathy,5 and macular oedema secondary to radiation retinopathy6; and neoplastic such as choroidal haemangioma7 and choroidal metastases.8 In general, PDT is well tolerated with relatively little collateral damage to vital structures and for that reason we elected to offer PDT as a treatment for symptomatic patients with serous retinal detachment associated with choroidal naevi.
Materials and methods
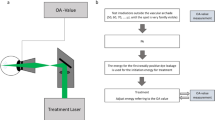
Records of all patients seen in our ocular oncology clinic are stored in an electronic database. Review of these records identified seven patients with symptomatic choroidal naevus treated with PDT in the period July 2002 to November 2005. All patients had been referred as possible cases of uveal melanoma. Each patient underwent full ophthalmic examination including measurement of Snellen visual acuity, slit-lamp examination, and indirect ophthalmoscopy. Ancillary investigations included fundus photography, A and B-scan ultrasonography, fluorescein and ICG angiography and where available, ocular coherence tomography. Risk factors for growth such as surface orange pigment, thickness, symptoms, subretinal fluid, and peripapillary location were assessed for each patient. In each case, the diagnosis was felt to be choroidal naevus and observation was recommended. Subsequently, each of the seven patients developed symptoms attributable to serous retinal detachment, principally blurring or distortion of vision. In no case was there evidence of growth of the lesion nor of choroidal neovascularization and after appropriate counselling, each patient was offered treatment with PDT. PDT was administered according to the TAP protocol.4 A single intravenous dose of verteporfin (6 mg/m2) was infused over 10 min. Five minutes following the infusion, diode laser (690 nm wavelength) of 600 mW/cm2 intensity was applied to the surface of the naevus for 83 s per application. If a single application was insufficient to cover the lesion then overlapping spots were applied.
Results
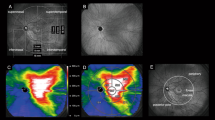
Seven patients (five females, two males, age range 41–64 years) were treated with PDT between July 2002 and November 2005. Four patients received one treatment (Figure 1), two patients received two treatments, and a single patient received three treatments over a 2-year period. No patient suffered any acute side effect relating to the use of PDT. Mean follow-up was 14 months (range 6–38 months). Visual acuity results are shown in Table 1. All seven patients showed symptomatic improvement with a reduction in visual blur or distortion. Five patients demonstrated a sustained improvement in visual acuity. In one patient, acuity remained unchanged and a further patient acuity decreased from 6/9 to 6/36 over a 3-year period. This patient underwent three sessions of PDT over a 2-year period and noted visual improvement after the first two sessions. At the last assessment, the macula was dry; however, RPE/photoreceptor atrophy was noted.
Conclusion
Although symptoms are a recognized risk factor for growth of uveal melanocytic lesions, they themselves do not indicate malignancy. One study1 showed that 11% of otherwise benign choroidal naevi exhibited symptoms secondary to serous retinal detachment (50%), photoreceptor atrophy (42%), or subretinal choroidal neovascularization (8%). A number of treatments have been recommended for fluid accumulation associated with choroidal naevi including argon laser2 and transpupillary diode laser thermotherapy.3
PDT is now well established as a treatment for a number of ophthalmic conditions principally choroidal neovascularization secondary to age-related macular degeneration4 and choroidal haemangioma.7 In addition, there have been numerous reports published describing the use of PDT in conditions as diverse as retinal capillary angioma,9 centro-serous retinopathy,5 choroidal metastasis,8 and exudative radiation retinopathy.6 The mode of action of PDT is not completely understood. Histological studies have shown that the principal effect of PDT is a selective occlusion of the choriocapillary layer with relative sparing of photoreceptors and retinal pigment epithelium.10 It is possible that in our patients, the resultant reduction in blood flow reduced fluid transudation through an attenuated retinal pigment epithelium overlying these longstanding naevi.
In conclusion, PDT appears to be a useful treatment for symptomatic serous detachment associated with choroidal naevi, at least in the short term. Longer follow-up will show whether these beneficial effects are maintained.
References
Gonder JR, Augsberger JJ, McCarthy EF, Shields JA . Visual loss associated with choroidal nevi. Ophthalmology 1982; 89 (8): 961–965.
Slusher MM, Weaver RG . Presumed choroidal naevi and sensory retinal detachment. Br J Ophthalmol 19977; 61: 414–416.
Duquesne N, Hajji Z, Jean-Lous B, Grange J-D . Choroidal naevi associated with serous macular detachment. J Fr Ophthalmol 2002; 25: 393–398.
TAP Study Group. Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin: one-year results of 2 randomized clinical trials-TAP report 1. Arch Ophthalmol 1999; 117: 1329–1345.
Canakis C, Livir-Rallatos C, Panayiotis Z, Livir-Rallatos G, Persidis E, Conway MD et al. Ocular photodynamic herapy for serous macular detachment in the diffuse retinal pigment epitheliopathy variant of idiopathic central serous chorioretinopathy. Am J Ophthalmol 2003; 136: 750–752.
Bakri SJ, Beer PM . Photodynamic therapy for maculopathy due to radiation retinopathy. Eye 2005; 19: 795–799.
Singh AD, Kaiser PK, Sears JE, Gupta M, Rundle PA, Rennie IG . Photodynamic therapy of circumscribed choroidal haemangioma. Br J Ophthalmol 2004; 88: 1414–1418.
Harbour JW . Photodynamic therapy for choroidal metastasis from carcinoid tumor. Am J Ophthalmol 2004; 137: 1143–1145.
Aaberg Jr TM, Aaberg Sr TM, Martin DF, Gilman JP, Myles R . Three cases of large retinal capillary hemangiomas treated with verteporfin and photodynamic therapy. Arch Ophthalmol 2005; 123: 328–332.
Schmidt-Erfurth U, Laqua H, Schlotzer-Schrehard U, Viestenz A, Naumann GOH . Histopathological changes following photodynamic therapy in human eyes. Arch Ophthalmol 2002; 120: 835–844.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rundle, P., Rennie, I. Management of symptomatic choroidal naevi with photodynamic therapy. Eye 21, 1531–1533 (2007). https://doi.org/10.1038/sj.eye.6702623
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702623
Keywords
This article is cited by
-
Treatment response to intravitreal bevacizumab in small pigmented choroidal lesions with subretinal fluid
BMC Ophthalmology (2019)
-
Lasers for the treatment of intraocular tumors
Lasers in Medical Science (2013)