Abstract
Purpose
To evaluate retinal sensitivity and fixation patterns in patients with Best's dystrophy by microperimetry (MP) and to correlate the results with static perimetry and retinal morphology seen by autofluorescence (AF).
Methods
Central 10° visual fields in 11 patients with Best's dystrophy (VA: 0.5±0.38) were recorded by the Octopus M2 TOP program and by MP (MP1, Nidek Technologies). AF was recorded by HRA (Heidelberg Engineering).
Results
High correlation (R=0.75, −0.76, −0.48) was found between static perimetry (MS, MD and CLV indices) and MP. Based on MP and AF results, three groups of patients were formed. Patients in the first two groups fixated inside the central nonuniform hypo- and hyperfluorescent AF ring area, next to relative (Group 1) or absolute scotoma (Group 2). Inner parts of the retina close to the fovea were most affected, whereas regions closer to the periphery of the 10° visual field showed near normal function. As the disease progressed, there was an evident shift of fixation to preferential retinal locus (PRL) in eight eyes with visual acuity 0.2 or less (Group 3). Fixation shift was superior in four eyes, temporal in two eyes, and nasal in two eyes.
Conclusion
MP enabled a highly sensitive topographic monitoring of retinal function, showing central or pericentral fixation in the early stages, until loss of central function, in eyes with VA 0.2 or less, caused evident shift of fixation to PRL. PRL was never situated inside the central uniform hypofluorescent area, but corresponded with the hyperfluorescent ring seen with AF imaging.
Similar content being viewed by others
Introduction
Best's vitelliform dystrophy (BVD) usually starts at an early age and progressively affects a patient's central vison.1 It is caused by the mutation in the VMD2 gene, encoding an integral membrane protein bestrophin that forms the chloride channel in the basolateral membrane of the RPE.2, 3, 4 BVD is a clinically heterogenous and pleomorphic disease where ophthalmoscopically visible changes often do not correspond with deterioration of visual function.
It is well known that patients with low vision from macular diseases have disrupted central vision, frequently including macular scotomas.5 In the majority of patients with low vision from central sensory deficit, the visual system has adapted by choosing an eccentric preferred retinal locus (PRL) to perform visual tasks that used to be performed by nonfunctioning fovea.
It has recently become possible to study the macular scotoma characteristics and visual performances by a microperimetry (MP)-based nonmydriatic fundus camera with an eye-tracker. This is a relatively new psychophysical method that enables one to compare retinal morphology with retinal function by simultaneously testing central retinal sensitivity and fixation patterns in relation to the fundus image. Visual fields examined with fundus perimetry showed reliable measurements in a range comparable to conventional computerised perimetry in normal individuals.6, 7 MP has a great potential for achieving deeper understanding of how patients with macular scotomas use their remaining vision. In patients with juvenile macular dystrophies, there might be ‘subclinical’ pathology adjacent to the visible atrophic regions on the fundus that is affecting visual performance and is not visible on ophthalmoscopy or fluorescein angiography.8 The type of scotoma may affect shifting of fixation points and possibly result in a difference in visual acuity.9
Fundus autofluorescence imaging (AF) provides new information regarding the morphologic status of RPE by giving information about content and spatial distribution of lipofuscin in eyes with retinal dystrophies.10, 11 Lipofuscin accumulation is common in many retinal dystrophies, showing different patterns of distribution on the patient's fundus.12, 13 The evolution of the AF pattern in BVD indicates centrifugal spreading of retinal dysfunction, showing initial hyperfluorescence areas centrally in the fovea, which are later replaced by central hypofluorescence areas surrounded by hyperfluorescent rings.14 The pattern of AF in patients with BVD shows regionally increased AF at the centre of the macula.15 A higher than normal fundus AF was reported in 109 of 118 patients with inherited macular dystrophies, among them 16 patients with BVD.16
The aim of the present study was to evaluate the central retinal function in patients with BVD by studying retinal sensitivity, types of retinal scotomas, and fixation patterns by MP, and to correlate the results with conventional static perimetry. The influence of fixation shift on type of central scotomas seen by static perimetry was studied and the results of MP testing were superimposed onto the AF imaging, to see how ‘subclinical’ pathology of altered RPE morphology affects retinal function, types of scotoma and shiftings of fixation.
Patients and methods
A total of 11 patients with BVD (five females, six males, age from 15 to 61 years, mean VA: 0.5±0.38) were included in the study. The diagnosis was based on detailed family history, evident macular changes and absence of the light peak on EOG.
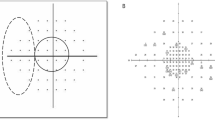
MP (MP1, Nidek Technologies) was performed on all the patients. Microperimeter is an optical instrument with an incorporated eye tracking system for functional retinal mapping, enabling fundus-controlled static perimetry of the central visual field. The central 10° visual field was tested with the Humphrey 10–2°16 dB56s or Humphrey 10–2°4 dB56s program (fast strategy, background illumination: 1.27 cd/m2, stimulation time 200 ms, stimulation spot size: Goldmann III). In all, 0 dB (equivalent to 1.27 cd/m2) represented the brightest luminance, and the stimulus intensity varied from 0 to 20 dB. The 16 dB program was used in 16 eyes and the 4 dB pattern in six eyes with worse visual acuity. The average retinal sensitivity for all 56 tested points was calculated. Results were expressed as percentages (%) of the normal value (normal meaning either 16 or 4 dB, depending on which program was used). In order to see the topographic distribution of retinal sensitivity in relation to the fovea, tested points were connected in the form of five ‘concentric’ rings (Figure 1). The average retinal sensitivity for each ring was calculated separately and expressed as a percentage of the normal value.
A red cross was used for fixation. The stability of fixation was determined by MP1, by monitoring how many fixation points were within 2–4° away from the fixation cross. Owing to advanced fundus changes in patients with macular diseases, it is often hard to determine the precise location of the fovea. Rohrschneider, who studied the exact foveal location in relation to the optic disc in normal individuals, found that the mean angle [α] between the horizontal line through the centre of the disc and the line connecting the centre of the disc with the fovea was relatively stable with the value being −5.6°±3.3°.17
The mean angle [α] was therefore calculated in our patients with the help of the equation tg[α]=y/x, x being the horizontal line from the centre of the optic disc to the foveal plane and the y being the vertical distance between the horizontal line through the optic disc and the fovea. According to data about the normal mean angle the fixation of our patients was determined to be central or eccentric. It was noted that in some patients (Table 1, Group 3: patients 6 and 7) with evident horizontal shifting of fixation (x plane), the mean angle [α] remained in the normal range, whereas it changed dramatically with only minor vertical shifting of fixation (y plane). This is due to the fact that the proportion of y/x is around 1 : 10, so only minor changes in y plane are needed to change the [α]. The location of the fixation relative to scotoma was determined in two ways: first, it was examined whether the fixation was at the edge of scotoma or at a certain distance from scotoma, and second, spatial direction of eccentric fixation was determined by the most dominant direction in relation to the fovea.
The central 10° visual field was tested by the Octopus 101 M2 TOP program. The visual field was determined by using the visual field indices: MS (mean sensitivity), MD (mean defect), and CLV (corrected loss variance).
Fundus AF was recorded using a confocal scanning laser ophthalmoscope (Heidelberg Engineering Angiograph, HRA) according to the method described by Holz et al.18 An argon blue laser (488 nm) was used for excitation. A wide band-pass filter with a cutoff at 500 nm was inserted in front of the detector to record AF. The AF images showed a certain centrifugal pattern according to the progression of the disease—initially, there were localised areas of nonuniform hyperfluorescence centrally, later being replaced by central uniform hypofluorescent areas surrounded by hyperfluorescent rings. The horizontal radius of uniform hypofluorescent areas as well as the outer border of all hyperfluorescent rings was determined. The results of MP testing were superimposed onto the AF images with the Adobe Photoshop 7.0 program, precisely fitting all the retinal vessels, in order to compare types of fixation and retinal sensitivity with AF image.
The research followed the tenets of the Declaration of Helsinki and was approved by the Ethics Committee at the Ministry of Health of Slovenia.
Results
Topographic evaluation of retinal function by comparing MP testing and AF
The clinical characteristics are summarised in Table 1. Based on MP testing and AF imaging, the patients were classified in three groups according to the pattern of fixation change with progression of BVD. The right eye of patient 7 was excluded due to technical problems with MP.
Patients in Group 1 (eight eyes) were fixating centrally next to relative scotoma inside the nonuniform hyperfluorescent region, as seen with AF (Figure 2). The fixation was stable, with less than 2° shifting away from the mean angle of fixation.
Group 1. Patient fixating next to relative scotoma inside the nonuniform hyperfluorescent area as seen with AF. VA: 1.0. (Table 1, Group 1: patient 2).
Patients in Group 2 (five eyes) were fixating centrally and pericentrally, next to 0 dB relative or absolute scotoma, inside or at the edge of a nonuniform hypo- and hyperfluorescent round lesion seen with AF (Figure 3). Fixation was stable in all of them with less than 2° shifting away from the mean angle of fixation.
Group 2. Patient with ring scotoma and stable central fixation next to 0 dB absolute scotoma. The hyperfluorescent round central area, representing still-functioning retina with stable fixation being surrounded with a hypofluorescent area (corresponding to absolute and relative ring scotoma) and a hyperfluorescent ring. There is a normally functioning retina outside the outer hyperfluorescent ring.VA: 0.4. (Table 1, Group 2: patient 6).
Patients in Group 3 (eight eyes) were fixating eccentrically at PRL more than 8° away from the mean angle of fixation (Figure 4). AF images showed a uniform hypofluorescent area centrally, corresponding to absolute scotoma, surrounded with a hyperfluorescent ring. PRL was located either at the edge of hyperfluorescent ring or further away on the normally appearing retina with AF imaging. The fixation was stable in three eyes, relatively unstable in four eyes, and unstable in one eye. It shifted superior in four eyes, temporal in two eyes, and nasal in two eyes.
Group 3. LE of the same patient as in Figure 2. with dense central scotoma and temporal parafoveal shifting of fixation. There is a uniform hypofluorescent area centrally, corresponding to absolute and relative central scotoma, being surrounded with a hyperfluorescent ring. The location of the new PRL corresponded with the hyperfluorescent ring seen with the AF imaging, appearing like a border between the atrophic and normal functioning part of the retina. VA: 0.2. (Table 1, Group 3: patient 6).
The data of patients in different groups are summarised in Table 2.
Correlation between MP and static perimetry
There was a high correlation found between MP and static perimetry (Figures 5, 6 and 7). The correlation coefficient was higher for MS and MD (R=0.75 and R=−0.76) than for CLV index (R=−0.48).
MP enabled us to correlate retinal morphology with retinal function, simultaneously observing the fixation pattern. A patient with paracentral shifting of fixation is shown as a case report in order to show how important fixation pattern is when interpreting the type of scotoma seen with static perimetry in patients with macular diseases (Figure 8).
A 31-year-old female (Table 1, patient 7, Groups 2 and 3) with relatively symmetric macular lesions on colour fundus photographs, but different extent of retinal damage seen with AF imaging. In her right eye with still central and stable fixation (VA: 0.8), there was a nonuniform, relatively hypofluorescent area centrally (corresponding to 0 dB relative scotoma), being surrounded with a hyperfluorescent ring. In her left eye, with absolute central scotoma and eccentric shift of fixation to PRL towards papillae (VA: 0.1), there was a relatively uniform hypofluorescent area (corresponding to the absolute central scotoma) centrally, being surrounded with a double concentric hyperfluorescent ring. PRL was located approximately between these two rings at the ‘border’ between the normally and abnormally functioning parts of the retina. Note that absolute central scotoma with nasal shifting of fixation in her left eye (seen with MP) may erroneously be interpreted as eccentric when seen only with static perimetry.
MP in five concentric rings within the 10° visual field in patients with central fixation
In order to see the topographic distribution of retinal sensitivity in relation to the fovea, the results of retinal sensitivity of centrally and pericentrally fixating patients (Groups 1 and 2) were represented in the form of five concentric rings (Table 3, Figure 1).
The scotomas were most dense in the first concentric ring (within 1.4° of the fovea), being 57.9% of mean normal value, getting progressively shallower when moving towards the periphery of the central 10° visual field.
Discussion
Progression of BVD, indicated with deterioration of VA and more dense central scotomas detected with static perimetry, showed a high correlation with MP results. The compatibility of MP and static perimetry has already been proven showing that test results obtained by MP can be related to test results obtained by Octopus M1 in the same location.6, 7 Our study is, as far as we know, the first one that compares MP and static perimetry in patients with Best's disease. The MP method appears to be qualitatively superior to automatic perimetry, with an important ability of fundus-controlled fixation screening. With static perimetry, central scotoma may erroneously be interpreted as eccentric unless the fact of shifting fixation to PRL is known (Figure 8).
Previous studies have shown that size, location and density of scotomas as well as location of PRL cannot be consistently inferred from the ophthalmoscopic appearance of the macula. In our study, it has been also shown that AF imaging helps to define ‘subclinical pathology’ in the early stages of the disease. The AF imaging in patients with central or slightly eccentric fixation usually showed a round, nonuniform area of hypo- and hyperfluorescence, corresponding to relative or absolute scotomas (Groups 1 and 2). The inner parts of the retina close to the fovea were the most affected, whereas parts closer to the periphery of the 10° visual field showed nearly normal function. With progression of the disease, there was a centrifugal spreading of retinal dysfunction from the centre towards the periphery, with progressive enlargment of central uniform hypofluorescent areas and shifting of fixation to PRL in eyes with visual acuity 0.2 or lower (eight eyes in Group 3). It has already been proposed that the absence of AF centrally, perceived at the site of atrophy in later stages, is indicative for loss of photoreceptor cells or at least their outer segments.19 On the other hand, hyperfluorescent regions at the edge of atrophy, showing excessive lipofuscin accumulation, still show function, with PRL being located at the outer edge of the hyperfluorescent ring (Figure 4). The fixation in Group 3 shifted superiorly in four eyes, temporally in two eyes, and nasally in two eyes. A large study of PRL in relation to macular scotomas in a low-vision population has shown that there is a strong tendency to avoid field defects below fixation, as this may interfere with many visual tasks such as walking and reading that require information from the inferior visual field.5 Among our patients, there was only one patient with minor shifting of the fixation inferior of the fovea (Table 1, Group 2: patient 8), thus having a visual defect in the lower visual field as in cases that had been reported to be rare. On the AF image of this eye, there was a relatively small hypofluorescent area corresponding to absolute scotoma, thus probably not interfering so much with visual function.
In comparison to the pattern of fixation reported in Stargardt's disease, with dense central scotoma, there was a superior shift of fixation observed in three out of four eyes, with unstable fixation in all the eyes.9 Interestingly, the fixation in patients with BVD, although eccentric (Group 3), was stable in three out of eight eyes, relatively unstable in four, and unstable in one eye only. This may be due to the fact that in patients with Stargardt's disease, the damage between the eyes was relatively symmetric (VA: 0.01 o.u.), whereas it showed asymmetry in patients with Best's disease. The stability of fixation (except for those patients with bilateral stable fixation) was never symmetric between the eyes of the same patient. The eye with worse visual acuity and shifting of fixation to PRL (Table 1, patients 5, 6) showed relatively unstable fixation, whereas the other eye of the same patient with better visual acuity showed central, stable fixation. In patients with bilaterally poor visual acuity and shifting of fixation to PRL (Table 1, patients 9, 11), the eye with less vertical shifting showed better fixation than the other one.
In conclusion, MP enabled a highly sensitive topographic monitoring of the retinal function, showing central or pericentral fixation in early stages until loss of central function, in eyes with visual acuity 0.2 or less, caused evident shift of fixation to PRL.
References
Best F . Über eine hereditäre Maculaaffektion: Beitrage zur Vererbungslehre. Z Augenheilkund 1905; 13: 199.
Stone EM, Nichols BE, Streb LM, Kimura AE, Sheffield VC . Genetic linkage of vitelliform macular degeneration (Best's disease) to chromosome 11q13. Nat Genet 1992; 1(4): 246–250.
Bakall B, Marknell T, Ingvast S, Koisti MJ, Sandgren O, Li W et al. The mutation spectrum of the bestrophin protein—functional implications. Hum Genet 1999; 104(5): 383–389.
Pianta MJ, Aleman TS, Cideciyan AV, Sunness JS, Li Y . In vivo micropathology of Best macular dystrophy with optical coherence tomography. Exp Eye Res 2003; 76: 203–211.
Fletcher DC, Schuhard RA . Preferred retinal loci relationship to macular scotomas in a low vision population. Ophthalmology 1997; 104(4): 632–638.
Andersen MVN . Scanning laser ophthalmoscope microperimetry compared with octopus perimetry in normal subjects. Acta Ophthalmol Scand 1996; 74: 135–139.
Rohrschneider K, Becker M, Schumacher N, Fendrich T, Volcker HE . Normal values for fundus perimetry with Scanning Laser Ophthalmoscope. Am J Ophthalmol 1998; 126(1): 52–58.
Sunness JS, Applegate CA, Haselwood D, Rubin GS . Fixation patterns and reading rates in eyes with central scotomas from advanced atrophic age related macular degeneration and Stargardt disease. Ophthalmology 1996; 103: 1458–1466.
Mori F, Ishiko S, Kitaya N, Takamiya A, Sato E, Hikichi T et al. Scotoma and fixation patterns using scanning laser ophthalmoscope microperimetry in patients with macular dystrophy. Am J Ophthalmol 2001; 132(6): 897–902.
Delori FC, Dorey CK, Staurenghi G, Arend O, Goger DG, Weiter JJ et al. In vivo fluorescence of the ocular fundus exhibits retinal pigment epithelium lipofuscin characteristics. Invest Ophthalmol Vis Sci 1995; 36: 718–729.
Delori FC, Staurenghi G, Arend O, Dorey CK, Goger DG, Weiter JJ .In vivo measurement of lipofuscin in Stargardt's disease—fundus flavimaculatus. Invest Ophthalmol Vis Sci 1995; 35: 2327–2331.
Von Rückmann A, Fitzke FW, Bird AC . Distribution of fundus autofluorescence with scanning laser ophthalmoscope. Br J Ophthalmol 1995; 79: 407–412.
Kennedy CJ, Rakozcky PE, Constable IJ . Lipofuscin of the retinal pigment epithelium. A rewiev. Eye 1995; 9: 763–771.
Jarc-Vidmar M, Kraut A, Hawlina M . Fundus autofluorescence imaging in Best's vitelliform dystrophy. Klin monatsbl Augenheilkund 2003; 220: 861–867.
Lois N, Halyfard AS, Bird AC, Fitzke FW . Quantitative evaluation of fundus autofluorescence imaged ‘in vivo’ in eyes with retinal disease. Br J Ophthalmol 2000; 84: 741–745.
von Rückmann A, Fitzke FW, Bird AC . In vivo fundus autofluorescence in macular dystrophies. Arch Ophthalmol 1997; 115: 609–615.
Rohrschneider K . Determination of the location of the fovea on the fundus. Invest Ophthalmol Vis Sci 2004; 45: 3257–3258.
Holz FG . Autofluorescenz-imaging der Makula. Ophthalmologe 2001; 98: 10–18.
von Rückmann A, Schmidt KG, Fitzke FW, Bird AC, Jacobi KW . Fundus autofluorescence in patients with hereditary macular dystrophies, malattia leventinese, familial dominant and age-related drusen. Klin Monatsbl Augenheilkd 1998; 213: 81–86.
Acknowledgements
This study was supported by the Grant of Ministry of Education, Science and Sports of Republic of Slovenia No. J3-4393. Authors are grateful to Barbara Klemenc for technical support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jarc-Vidmar, M., Popovič, P. & Hawlina, M. Mapping of central visual function by microperimetry and autofluorescence in patients with Best's vitelliform dystrophy. Eye 20, 688–696 (2006). https://doi.org/10.1038/sj.eye.6701949
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701949