Abstract
Purpose
To estimate the prevalence of posterior embryotoxon (PE) in the general ophthalmic clinic and to identify any features of PE that suggest that it is pathological rather than physiological.
Methods
Over 700 consecutive patients of all ages were examined with the slit lamp during their routine eye clinic appointment. Patients with posterior embryotoxon were invited to return for full ocular examination including keratometry, corneal topography, and gonioscopy.
Results
In all, 49 out of 723 patients were found to have PE. This gives a prevalence of 6.8% with an age range of 18 months to 95 years. There was a higher prevalence in the younger age group of 22.5% (age range 18 months to 20 years) compared to 5.9% in the older age range (21–95 years).
A total of 29 patients with PE returned for further examination. Six patients had glaucoma (two with Axenfeld's syndrome and one with aniridia), and one had ocular hypertension. In all, 20 patients had bilateral PE on slit-lamp examination, which increased to 24 with gonioscopy. The majority of the PE was seen temporally (97.9%) and limited to a few clock hours. Gonioscopy showed that eight patients with PE had associated inferior pigmentation of schwalbes line.
Conclusion
This large series found the prevalence of PE the general ophthalmic clinic to be 6.8%. Its presence should prompt careful anterior segment examination, including gonioscopy, to identify any associated abnormalities that may carry a risk of glaucoma. Children should also be assessed for any associated systemic or genetic abnormality.
Similar content being viewed by others
Introduction
Posterior embryotoxon (PE) is a corneal abnormality that is visible with slit-lamp biomicroscopy as a thin grey-white, arcuate ridge on the inner surface of the cornea, adjacent to the limbus. It is an anteriorly displaced Schwalbes line, the junction of Descemets membrane and the uveal trabecular meshwork. Histolgically, it consists of a central collagen core surrounded by a thin layer of descemets membrane, and is separated from the anterior chamber by a layer of endothelium. It may be an isolated finding or seen in the presence of other ocular anomalies, in particular Axenfeld–Riegers syndrome, or systemic disease, such as Alagille's syndrome.1
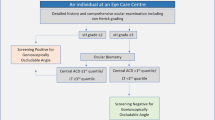
PE has been found to be present in anything from 8 to 32% of the general population.1, 2, 3, 4, 5 PE occurs in up to 95% of patients with Alagille's syndrome.6 This has led to the proposal that its presence could be used as a screening tool to aid diagnosis and avoid the need for more invasive tests in children with chronic cholestasis. However, an incidence of PE in the general population of 30% would make it useless for this task. Some of the studies of the incidence of PE are small, consider an isolated population, or are histological studies where the anomaly found might not have been easily visible clinically. This prospective study was therefore undertaken to estimate the prevalence of PE in the general ophthalmic clinic and to determine if there are any features that suggest that it is pathological rather than physiological.
Methods
An initial observational study was carried out by all of the authors during a 3-week period. Two clinics run by clinical assistants were not included because they were not confident of their ability to recognise PE, but all other clinics in the department were included. A total of 723 consecutive patients attending the eye clinic were examined for the presence of PE, which was visible without the need for gonioscopy. PE was defined as the presence of a prominent schwalbes line seen at the limbus. This consists of a ridge of tissue on the inner surface of the cornea and not just the golden glow of the trabecular region seen commonly at the limbus.
In all, 49 patients were identified with PE, and 42 were invited to return for a more detailed examination. The inclusion criteria for invitation were age over 12 years (gonioscopy being difficult to perform below this age) and the ability to be examined at the slit lamp. A total of 29 patients returned and were examined by a single observer (CR). This included a full medical and ophthalmic history, visual acuity, autorefraction, automated corneal topography, slit-lamp examination with applanation tonometry, indirect gonioscopy with a Goldman lens, and fundoscopy.
The extent of PE was measured in clock hours and the location recorded. If it occurred between 2–4 and 8–10 clock hours, it was considered to be in a nasal or temporal location depending on the eye. Gonioscopy was used to assess any difference between the extent of the PE compared with routine slit-lamp examination and to identify any associated angle abnormality. The angle was graded according to the Schaffer system, and the presence of pigmentation in the trabeculum, PE, or elsewhere was noted. Refractive errors and corneal topography were compared to the location of the PE to look for any association. The diagnosis of glaucoma was based on established findings of characteristic visual field loss and optic nerve changes.
This study was approved by the local ethics committee, and all patients gave informed consent.
Results
The initial prevalence survey found that 49 out of the 723 patients examined in the general ophthalmic clinic had PE. This gives a prevalence of 6.8% (age range 18 months to 95 years). Table 1 gives a breakdown of the figures in each 10-year age range. There was a higher prevalence in the younger age group of 22.5% (age range 18 months to 20 years) compared to 5.9% in the older age range (21–95 years).
In all, 29 patients returned for further examination. One patient had anirida with enucleation of one eye and multiple surgery on the remaining eye making it impossible to assess the features of PE. Five of the remaining 28 patients had glaucoma. The glaucoma was due to acute angle closure, primary open angle glaucoma, secondary to trauma, and in two eyes there was evidence of Axenfeld's syndrome. The other patients were seen in the clinic for a variety of unrelated reasons.
The PE seen with slit-lamp examination alone was unilateral in eight patients and bilateral in 20 patients. Gonioscopy increased the identification of PE and showed it to be bilateral in 24 patients. This means that for the 28 patients examined, 48/56 eyes had PE on slit-lamp examination, which increased to 52/56 eyes with gonioscopy. Four eyes of four patients had no evidence of PE with either examination method.
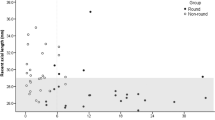
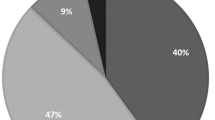
Evaluation of the external characteristics of PE was performed in the 48 eyes (of 28 patients) with PE visible at the slit-lamp. Here PE was most frequently located in the temporal position (47/48 eyes, 97%). It was located nasally in 22/48 eyes (45.8%). On average, the PE occupied 1.8 clock hours for either position ranging from 0.5 to 4 clock hours nasally, and up to 5 clock hours temporally. No patient had complete 360° PE on initial examination but gonioscopy revealed larger degrees of PE, with 16 eyes (in 10 patients) having complete PE on gonioscopic examination. The two patients with Axenfeld syndrome had only a few clock hours of PE with associated iris strands.
Gonioscopy of all 52 eyes that had evidence of PE revealed that the majority, 46/52 eyes (92.3%), had open angles. Table 2 summarises the gonioscopic findings. A total of 12 patients had evidence of pigmentation of either the trabeculum or inferior Schwalbes line. The majority of these had an association that might account for this increased pigment. The commonest anterior segment feature seen was cataracts in 12 patients. No patient had evidence of iris hypoplasia. Fundoscopy was unremarkable in 33 eyes of 20 patients. Evidence of congenital anomalies with tilted discs, coloboma, or optic disc drusen was seen in four eyes of three patients (see Table 3).
The refractive error distribution had no particular pattern with both hypermetropic and myopic errors being found. Three patients had evidence of high astigmatism (>2 D) and one patient had amblyopia due to a unilateral high myopia of −11D. No relationship was found between the position of the PE and the refractive error or corneal topography.
A review of the notes of the 49 patients of all ages who were identified as having PE during our observational study revealed that nine had evidence of glaucoma. Two-thirds (6/9) of the patients under the age of 20 have disorders that might be associated with anterior segment abnormalities. These include inherited cataracts, iris coloboma, microphthalmos and coloboma in a ring chromosome 19 mosaic abnormality, velocardiofacial syndrome (which is associated with juvenile onset glaucoma), and two cases of X-linked albinism. None had signs of glaucoma.
Discussion
PE was first described by Axenfeld in 1920. The incidence of PE varies between studies and many are hampered by the small sample size or the nature of the sample selection. Early studies were histological and found it to be present in up to 20% of eyes.3 Burian et al7 found an incidence of 15% both clinically and histologically, and showed that this was similar for both foetus and adult eyes. They recognised that glaucoma occurs in the presence of anomalies of the iris and angle, not just isolated PE. Forsius et al3 studied 498 subjects from an isolated Finnish Island community and found an incidence of 32%. Alkemade4 looked at 200 patients and found that although present in 12% of people, it affected only 8% of eyes. He could not confirm an association with iris stromal hypoplasia and found no difference in the rate of PE in a group of 100 patients with glaucoma. A recent study of 440 randomly selected patients in Japan found that 24.3% of patients had PE, many with associated abnormalities and neural crest cell maldevelopment.5 The relatively high number of associated abnormalities may arise from the nature of the patients being seen in a university hospital setting.
This study is the largest clinical study of PE. The overall prevalence was found to be 6.8% in the general ophthalmic clinic, lower than previous studies. The difference in the prevalence of PE between different age groups is related to the characteristics of these groups. Only a relatively small number of younger patients were seen and they were more likely to be referred because of ocular or systemic disease that is associated with anterior segment dysgenesis. Adult patients were commonly referred for age-related problems such as cataracts and diabetic screening. Also with increasing age, the PE becomes more difficult to see due to peripheral corneal opacity such as arcus senilis.
PE is seen with anterior segment abnormalities, which are thought to result from developmental arrest of structures derived from neural crest cell origin late in gestation.8, 9 This neurocristopathy may be a unifying concept for the associated optic nerve anomalies and systemic disease seen in conditions such as Alagille or Axenfeld–Reiger syndromes. Molecular genetic studies reveal that a number of mutations in genes controlling anterior segment development will result in the formation of PE and other abnormalities.10, 11 For example, defects in PITX2 and FOXC1 are associated with Axenfeld–Reiger syndrome and JAG1 with Alagille's syndrome.2, 10, 11, 12
Axenfeld–Reiger syndrome is an autosomal dominant condition characterised by iris strands spanning the angle to insert into the prominent Schwalbes line.10 The PE while often extensive in this condition may only be visible with gonioscopy, or be limited as in the two cases in this study.9 It carries a 50% risk of glaucoma, usually of early onset. All younger patients with PE should therefore be examined with gonioscopy.
This study does not address the risk of glaucoma in the presence of PE. Although there was a high proportion (18.4%) of patients with PE and glaucoma, this reflects the large number of patients with glaucoma who are followed up in the general clinics of this district hospital. Shields9 showed no increased risk for glaucoma in the presence of isolated PE, but the association of other anterior segment abnormalities with glaucoma is well recognised. The extent of PE viewed externally did not predict the presence of any underlying condition, and no link between refractive error, astigmatism, and the position of PE was found. Most of the children who were found to have PE had complete or extensive PE and associated anterior segment dysgenesis. Although this was not a population-based study, the wide variety of disorders associated with PE in children, none with Alagille's syndrome, indicate that this is a very nonspecific tool in the diagnosis of Alagille's syndrome. The presence of PE may be helpful in putting together the features of the syndrome, but it is not diagnostic and would not necessarily prevent the need for more invasive investigations.
In conclusion, the prevalence of PE in the general ophthalmic clinic was found to be 6.8%. No particular features of PE suggest that it is pathological rather than physiological, but the presence of other anterior segments abnormalities is significant. The presence of PE should prompt careful anterior segment examination and gonioscopy. It is important to identify any anterior segment syndromes, such as Axenfeld–Reiger, that will require long-term follow-up because of the risk of glaucoma. Children seen in the ophthalmic clinic with PE should be carefully examined for evidence of anterior segment dysgenesis, and any associated systemic or genetic abnormalities. A family history should be sought and because of the variability of expression an examination of parents and siblings considered.
References
Waring GO, Rodrigues MM, Laibson PR . Anterior chamber cleavage syndrome. Surv Ophthalmol 1975; 20: 3–27.
Azuma N, Yamada M . Missense mutation at the C terminus of the PAX6 gene in ocular anterior segment anomalies. Invest Ophthalmol Vis Sci 1998; 39: 828–830.
Forsius H, Eriksson A, Fellman J . Embryotoxon corneae posterius in an isolated population. Acta Ophthamol 1964; 42: 42–49.
Alkemade P . Dysgenesis Mesodermalis of the Iris and the Cornea. Charles C Thomas: Assen, Netherlands, 1969.
Ozeki H, Shirai S, Majima A, Sano M, Ikeda K . Clinical evaluation of posterior embryotoxon in one institution. Jpn J Ophthalmol 1997; 41: 422–425.
Hingorani M, Nischal KK, Davies A, Bentley C, Vivian A, Baker AJ et al. Ocular abnormalities in Alagille syndrome. Ophthalmology 1999; 106: 330–337.
Burian HM, Braley AE, Allen L . Visibility of the ring of Schwalbe and the trabecular zone. Arch Ophthalmol 1955; 53(6): 767–782.
Johnston MC, Noden DM, Hazelton RD . Origins of avian ocular and periocular tissue. Exp Eye Res 1979; 29: 27–43.
Shields MB . Axenfeld–Rieger syndrome: a theory of mechanism and distinctions from the iridocorneal endothelial syndrome. Trans Am Ophthalmol Soc 1983; 81: 736–784.
Alward LWM . Axenfeld–Rieger syndrome in the age of molecular genetics. Am J Ophthalmol 2000; 130: 107–115.
Hanson IM, Fletcher JM, Jordan T, Brown A, Taylor D, Adams RJ et al. Mutations at the PAX6 locus are found in heterogeneous anterior segment malformations including Peter's anomaly. Nat Genet 1994; 6: 168–173.
Jones EA, Clement-Jones M, Wilson DI . JAGGED1 expression in human embryos: correlation with the Alagille syndrome phenotype. J Med Genet 2000; 37: 658–662.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented as a free paper at the Royal College of Ophthalmologists Annual Congress, May 2001
Rights and permissions
About this article
Cite this article
Rennie, C., Chowdhury, S., Khan, J. et al. The prevalence and associated features of posterior embryotoxon in the general ophthalmic clinic. Eye 19, 396–399 (2005). https://doi.org/10.1038/sj.eye.6701508
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701508
Keywords
This article is cited by
-
Management of adults with Alagille syndrome
Hepatology International (2023)
-
Marshall–Smith syndrome
Journal of Perinatology (2015)