Abstract
Retinopathy of prematurity (ROP) is a well-recognized condition in premature babies born today and in the recent past. One would not normally expect to come across evidence of its existence among older patients. We present a case of apparent regressed ROP in a lady born in May 1939, prior to the documented reports of the first cases.
Similar content being viewed by others
Main
Case report
A 62-year-old lady presented with gradually decreasing vision in her right eye. She was myopic with a past history of retinal detachment in her left eye. There was no family history of any eye problems, and the patient did not volunteer any past medical history of note.
On examination, corrected visual acuities were 6/18 in the right eye, hand movements in the left. There was a left convergent squint, and bilateral lens opacities accounting for the decrease in vision in the right eye.
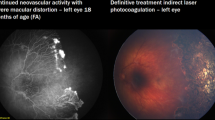
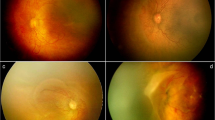
Dilated fundal examination on the right side revealed an abnormal disc appearance with peripapillary atrophy and marked dragging of the vessels (Figures 1 and 2). There was temporal vitreous condensation and abnormal vitreo-retinal attachment at the equator. Vascularization appeared complete to the periphery. No fundal view was possible on the left side.
On further questioning of the patient, a history of premature birth was elicited. Her parents told her that she had been born early, weighing ‘less than a bag of sugar’. She was cared for in a rudimentary neonatal unit, within Leeds Maternity Hospital at Hyde Terrace. A diagnosis of regressed ROP was made.
In support of this diagnosis were several factors. The patient had a history of premature birth, and there was no family history of eye problems as would be expected in familial exudative vitreoretinopathy, which has clinical similarities to ROP but an autosomal dominant inheritance pattern. The patient was myopic with a prescription in her right eye of −4.00/−0.50 × 180°. Biometry showed this to be a refractive myopia with an axial length of 23.15 mm, and high keratometry readings of 47.0 and 49.0 D. Gallo and Fagerholm1 looked at myopia up to 5 D in ROP patients, and noted the association with high keratometry readings rather than long axial lengths as the mechanism for the myopia. Another factor was that the retina was vascularized to the periphery, as would be expected in regressed ROP.
Regressed ROP is a risk factor for retinal detachment,2 and in our patient prophylactic argon retinopexy was carried out before proceeding to uneventful phacoemulsification surgery.
Comment
ROP, previously known as retrolental fibroplasia, came to the attention of ophthalmologists in the 1940s.3 It is interesting to consider the first reports of ROP in the context of developing neonatal care. Efforts to try and preserve lives of premature infants began in the 1870s. The first incubators were developed with the aim of keeping the child warm,4,5 with later addition of piped oxygen.6 Initially oxygen was used in short bursts, but use of continuous oxygen became widespread later. Literature from the time suggests that the use of incubators with oxygen was commonplace in both the US and the UK by the late 1930s. By the 1940s, the concept of separate neonatal units had spread to large centres in Europe and the US, and the numbers of surviving premature babies started to rise.
The first cases of ROP were described in Boston in 1941,7 with over a hundred further cases seen over 1942–1943. As more became known about the condition, the first signs were described making early diagnosis possible.
In England, ROP was not described until later. Crosse and Evans traced its history back to 1946.8,9 They were unable to find evidence of the condition's existence in children born prior to this date, despite searching older pathology records for conditions that may have been misdiagnosed. Literature from Oxford suggests that no cases were seen there in children born prior to 1947.10
Our patient, who was born earlier than the first reported cases of ROP in this country, seems likely to have received supplemental oxygen as a neonate, and presents a clinical picture consistent with regressed ROP. Her existence suggests that the beginning of the ‘epidemic’ of ROP may have been earlier and affected more babies than previously suspected. This becomes increasingly relevant as more people from this age group present for consideration of cataract surgery, underlining the importance of thorough preoperative assessment to reduce the risk of perioperative retinal detachment. The possibility of regressed ROP should also be borne in mind in patients with an appropriate history presenting with retinal detachment.
References
Gallo JE, Fagerholm P . Low grade myopia in children with regressed ROP. Acta Ophthalmol (Copenh) 1993; 71(4): 519–523.
Farr AK, Stark WJ, Haller M . Cataract surgery by phacoemulsification in adults with retinopathy of prematurity. Am J Ophthalmol 2001; 132(3): 306–310.
Silverman WA . Retrolental Fibroplasia: A Modern Parable. Grune & Stratton, Inc.: New York, NY, 1980.
Grulee CG, Bonar BE . The Newborn – Physiology and Care. D Appleton and Co.: New York/London, 1926.
Baker JP . The Machine in the Nursery – Incubator Technology and the Origins of Newborn Intensive Care. The Johns Hopkins University Press: Baltimore, London, 1996.
Hess JH . Oxygen unit for premature and very young infants. Am J Dis Child 1934; 47: 916–917.
Terry TL . Extreme prematurity and fibroplastic overgrowth of persistent vascular sheath behind each crystalline lens. 1. Preliminary report. Am J Ophthalmol 1942; 25: 203–204.
Crosse VM . The problem of retrolental fibroplasias in the city of Birmingham. Tr. Ophthalmol Soc UK 1951; 71: 609–612.
Evans PJ . Retrolental fibroplasia. Trans Ophthalmol Soc UK 1951; 71: 613–616.
Houlton ACL, Coxon M, Jackson CRS, Bembridge BA . A study of cases of retrolental fibroplasia seen in Oxford. Trans Ophthalmol Soc UK 1951; 71: 583–608.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cuthbertson, F., Bishop, F. & Dabbs, T. The earliest case of retinopathy of prematurity?. Eye 18, 314–315 (2004). https://doi.org/10.1038/sj.eye.6700622
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700622