Abstract
Purpose To study the expression of the extracellular matrix (ECM) proteins, tenascin, laminin, and fibronectin in the conjunctiva of patients with active vernal keratoconjunctivitis (VKC).
Methods Conjunctival biopsy specimens were obtained from nine patients with active VKC and 6 normal control subjects. The presence and distribution of tenascin, laminin, and fibronectin were assessed microscopically with immunohistochemical techniques and a panel of monoclonal and polyclonal antibodies directed against tenascin, laminin, and fibronectin.
Results In normal conjunctiva, weak immunoreactivity for tenascin was localized to the walls of blood vessels in the upper substantia propria. Weak immunoreactivity for laminin was located at the epithelial–stromal junction and in the walls of blood vessels. Staining for fibronectin was absent. In VKC specimens, intense immunoreactivity for tenascin was noted in the substantia propria associated with the inflammatory infiltrate and in the perivascular stroma. Intense immunoreactivity for laminin around all stromal vessels and fibrillar immunoreactivity among basal epithelial cells were noted. There was no immunoreactivity for fibronectin.
Conclusion Our data indicate increased deposition of tenascin and laminin in the conjunctiva from patients with active VKC. Our findings suggest that tenascin and laminin might play distinct roles in chronic inflammation seen in VKC.
Similar content being viewed by others
Introduction
Vernal keratoconjunctivitis (VKC) is a chronic, seasonally exacerbated bilateral external allergic ocular inflammation characterized by tarsal conjunctival giant papillae and limbal thickening and opacification resulting from hyperplasia of conjunctival connective tissue. Conjunctival remodelling, characterized by extensive deposition of the interstitial proteins collagen types I, III, IV, V, and VII in the substantia propria, is a hallmark of the lesions of VKC.1,2
Inflammation is characterized by the appearance of many extracellular matrix (ECM) components in a spatial and sequential pattern suggesting that mechanisms functioning during embryonic development may be recapitulated during inflammation.3 Tenascin is a large hexameric ECM glycoprotein that is found in embryonic tissues, especially at epithelial–mesenchymal junctions, and in developing brain tissue, where it probably plays a role in epithelial–mesenchymal induction and migration. Its expression is restricted in adult human tissues, and re-expression occurs during wound healing, tissue remodelling, and in tumour stroma. Tenascin is believed to play important roles in tissue development, wound healing, and repair, because it mediates several cellular activities including cell adhesion and antiadhesion, migration, proliferation, and differentiation.4,5 Laminin constitutes one of the major ECM components of the basement membrane and is known to have effects on diverse cell functions such as cell migration, growth, and differentiation.6 Fibronectin is a large-molecular-weight adhesive glycoprotein that participates in the regulation of cell proliferation and migration, especially during wound healing.7
Since conjunctival remodelling is a feature of VKC, we hypothesized that the extracellular matrix proteins tenascin, laminin, and fibronectin are upregulated in the conjunctiva from patients with active VKC. To test our hypothesis, we used immunohistochemical techniques to study the expression of tenascin, laminin, and fibronectin in the conjunctiva from patients with active VKC and from normal individuals.
Patients and methods
Patients
Nine consecutive patients with active VKC seen at the outpatient clinic of King Abdulaziz University Hospital were included in the study. The patients were six males and three females. The mean age was 12.6±2.3 years (range: 8–15 years). The symptoms mentioned by all the patients were itching, redness, photophobia, and tearing. Each patient underwent complete ophthalmic examination and the corneal and conjunctival changes were noted and recorded. All patients had the limbal form of the disease characterized by broad gelatinous infiltrates of the limbus. Nasal or temporal limbal conjunctival biopsy specimens were obtained from each patient. None of the patients was on topical therapy before obtaining the biopsy. In addition, six limbal conjunctival biopsy specimens were obtained from the same areas in patients undergoing strabismus surgery without obvious inflammation and served as controls. The controls were from the same age group.
Immunohistochemical staining
The conjunctival biopsy specimens were immediately snap frozen in Tissue-Tek optimum cutting temperature (OCT) compound (Miles Laboratories, IN, USA) and maintained at −80oC until use. For immunohistochemistry, 5 μm serially cut cryostat sections were dried overnight at room temperature, fixed in absolute acetone for 10 min, then treated with 2% hydrogen peroxide in methanol for 3 min to block endogenous peroxidase activity, and stained with a three-step avidin–biotinylated peroxidase-labelled complex procedure. The slides for tenascin detection were incubated with monoclonal mouse anti-human tenascin antibody (DAKO-tenascin, TN2, Carpinteria, CA, USA) diluted 1 : 50. The slides for laminin detection were incubated with polyclonal antilaminin antibody (CAPPEL, Turnhout, Belgium) diluted 1 : 50. The slides for fibronectin detection were incubated with rabbit anti-human fibronectin antibody (DAKO A/S, Glostrup, Denmark) diluted 1:750. The sections were then incubated with the biotinylated secondary antibody and reacted with the avidin–biotinylated peroxidase complex (Dakopatts, Copenhagen-Denmark). All incubations were carried out for 30 min at room temperature, then washed in three changes of phosphate-buffered saline at pH 7.2 for 15 min. The reaction product was visualized by incubation for 10 min in 0.05 M acetate buffer at pH 4.9, containing 0.05% 3-amino-9-ethyl-carbazole and 0.01% hydrogen peroxide, resulting in bright-red immunoreactive sites. The slides were faintly counterstained with Harris haematoxylin. Finally, the sections were rinsed with distilled water and coverslipped with glycerol. Slides used as controls for the staining were treated in an identical manner, except that an irrelevant antibody was used in the first step or the primary antibody was omitted. Positive controls were previously positive-staining tissue, and included samples from the small intestine from patients with Crohn's disease and samples from the liver.
Results
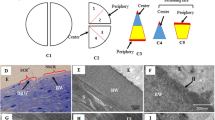
There was no staining in the negative control slides. In normal conjunctival tissue specimens, weak immunoreactivity for tenascin was limited to the walls of blood vessels in the upper substantia propria (Figure 1). Weak immunoreactivity for laminin was observed at the epithelial–stromal junction and in the walls of blood vessels (Figure 2). There was no immunoreactivity for fibronectin.
All VKC specimens showed similar findings. Intense band-like imunoreactivity for tenascin was noted in the upper substantia propria (Figure 3). There was a close association between tenascin expression and the inflammatory infiltrate (Figure 4). The composition of the inflammatory infiltrate in VKC was described in previous reports.8,9,10 In addition, intense immunoreactivity for tenascin was noted in the perivascular areas in the substantia propria (Figure 3). Intense immunoreactivity for laminin was noted around all stromal vessels. In addition, fibrillar immunoreactivity for laminin was noted among the basal epithelial cells (Figure 5). There was no immunoreactivity for fibronectin.
Discussion
In normal conjunctiva, tenascin was weakly expressed in the walls of blood vessels. This observation was consistent with the findings of previous reports.11 In contrast, the conjunctiva from patients with active VKC showed increased tenascin immunoreactivity. Our results point to a clear association between the inflammatory infiltrate and tenascin immunoreactivity in the upper substantia propria close to the epithelial cells. The finding of a close correlation between the inflammatory infiltrate and tenascin expression is supported by others.3 In normal conjunctiva, laminin immunoreactivity was localized at the basement membrane areas of the conjunctival epithelium and stromal blood vessels. This observation was consistent with the findings of previous studies that localized laminin immunoreactivity in basement membranes of conjunctival epithelium and blood vessels.12 In VKC specimens, intense immunoreactivity for laminin was noted around stromal vessels and fibrillar immunoreactivity was noted among basal epithelial cells. Although, some groups have found fibronectin in the basement membranes of the conjunctival epithelium and stromal blood vessels,12 we did not detect fibronectin in the conjunctiva from normal controls and patients with VKC. Thus, our results suggest that the conjunctiva is lacking fibronectin or that in the conjunctiva there is another fibronectin isoform that our antibody did not recognize. Several studies demonstrated that cytokines such as transforming growth factor-β (TGF-β) are the major known upregulators of tenascin13 and laminin14 synthesis.
The function of inflammatory cells participating in chronic inflammation may be modulated through the altered organization of ECM in chronically inflamed tissues. It has been suggested that tenascin acts as an immunomodulator altering the adhesion properties of human monocytes, B cells, and T cells, and inhibits T-lymphocyte activation.15 Laminin serves as a substrate for the attachment and spreading of human inflammatory cells. Cell adhesion to laminin has been shown to affect cellular functions including enhanced cytokine production by T-lymphocytes,16 enhanced mast cell activation and secretion,17 and proliferation of macrophages.18 There is also evidence from in vitro studies that tenascin promoted the transition of endothelial cells from a resting to a sprouting phenotype,19 and that laminin induces differentiation of human endothelial cells into capillary-like structures.20 In addition, tenascin and laminin increase the expression of matrix metalloproteinase-9 (gelatinase B) by macrophages.21 The presence of tenascin and laminin in VKC might, therefore, increase the activity of matrix metalloproteinases, which in turn promotes the breakdown of ECM, and possibly modulates ECM remodelling which are components of chronic inflammatory response. In a previous study, we demonstrated a significant increased expression of gelatinase B in the conjunctiva from patients with VKC.22
In conclusion, these results indicate that chronic inflammation in VKC is associated with increased deposition of tenascin and laminin that may reflect remodelling of the conjunctiva. The adhesive properties of tenascin and laminin may offer a relevant explanation for the mechanism by which inflammatory cells transmigrate into conjunctiva of patients with VKC. In addition, tenascin and laminin are able to induce the expression of matrix metalloproteinases. These enzymes would disrupt the integrity of the ECM, allowing invasion of inflammatory cells and contributing to tissue remodelling.
References
Abu El-Asrar AM, Geboes K, Al-Kharashi SA, Al-Mosallam AA, Tabbara KF, Al-Rajhi AA et al. An immunohistochemical study of collagens in trachoma and vernal keratoconjunctivitis. Eye 1998; 12: 1001–1006.
Leonardi A, Brun P, Tavolato M, Abatangelo G, Plebani M, Secchi AG : Growth factors and collagen distribution in vernal keratoconjunctivitis. Invest Ophthalmol Vis Sci 2000; 41: 4175–4181.
Kusubata M, Hirota A, Ebihara T, Kuwaba K, Matsubara Y, Sasaki T et al. Spatiotemporal changes of fibronectin, tenascin-C, fibulin-1, and fibulin-2 in the skin during the development of chronic contact dermatitis. J Invest Dermatol 1999; 113: 906–912.
Jones FS, Jones PL . The tenascin family of ECM glycoproteins: structure, function, and regulation during embryonic development and tissue remodelling. Dev Dyn 2000; 218: 235–259.
Chiquet-Ehrismann R, Hagios C, Matsumoto K . The tenascin gene family. Perspect Develop Neurobiol 1994; 2: 3–7.
Lin ML, Bertics PJ . Laminin responsiveness is associated with changes in fibroblast morphology, motility, and anchorage-independent growth: cell system for examining the interaction between laminin and EGF signaling pathways. J Cell Physiol 1995; 164: 593–604.
Vartio T, Vaheri A . Fibronectin; chains of domains with diversified functions. Trends Biochem Sci 1983; 8: 442–424.
Abu El-Asrar AM, Geboes K, Al-Kharashi S, Tabbara KF, Missotten L, Desmet V . Adhesion molecules in vernal keratoconjunctivitis. Br J Ophthalmol 1997; 81: 1099–1106.
Abu El-Asrar AM, Fatani RA, Missotten L, Geboes K . Expression of CD23/CD21 and CD40/CD40 ligand in vernal keratoconjunctivitis. Eye 2001; 15: 217–224.
Abu El-Asrar AM, Al-Kharashi SA, Al-Mansouri S, Missotten L, Geboes K . Langerhans' cells in vernal keratoconjunctivitis express the costimulatory molecule B7-2 (CD86), but not B7-1 (CD80). Eye 2001; 15: 648–654.
Mastuda A, Tagawa Y, Mastuda H . TGF-β2, tenascin, and integrin β1 expression in superior limbic keratoconjunctivitis. Jpn J Ophthalmol 199l; 43: 251–256.
Fukuda K, Chikama T, Nakamura M, Nishida T . Differential distribution of subchains of the basement membrane components type IV collagen and laminin among the amniotic membrane, cornea, and conjunctiva. Cornea 1999; 18: 73–79.
Linnala A, Kinnula V, Laitinen LA, Lehto V-P, Virtanen I . Transforming growth factor-β regulates the expression of fibronectin and tenascin in BEAS 2β human bronchial epithelial cells. Am J Respir Cell Mol Biol 1995; 13: 578–585.
Neubauer K, Kruger M, Quondamatteo F, Knittel T, Saile B, Ramadori G . Transforming growth factor-beta 1 stimulates the synthesis of basement membrane proteins laminin, collagen type IV and entactin in rat liver sinusoidal endothelial cells. J Hepatol 1999; 31: 692–702.
Ruegg CR, Chiquet-Ehrismann R, Alkan SS . Tenascin, an extracellular matrix protein, exerts immunomodulatory activities. Proc Natl Acad Sci USA 1989; 86: 7437–7441.
Li YQ, Kobayashi M, Yuan L, Wong J, Matsushita K, Hamada JJ et al. Protein kinase C mediates the signal for interferon-gamma mRNA expression in cytotoxic T cells after their adhesion to laminin. Immunology 1998; 93: 455–461.
Vliagoftis H, Metcalfe DD . Characterization of adhesive interactions between mast cells and laminin isoforms: evidence of a principal role for α6 integrin. Immunology 1997; 92: 553–560.
Ohki K, Kohashi O . Laminin promotes proliferation of bone marrow-derived macrophages and macrophage cell lines. Cell Struct Funct 1994; 19: 63–71.
Canfield AE, Schor AM . Evidence that tenascin and thrombospondin-1 modulate sprouting of endothelial cells. J Cell Sci 1995; 108: 797–809.
Ponce ML, Nomizu M, Kleinman HK . An angiogenic laminin site and its antagonist bind through the alpha (V) beta 3 and alpha 5 beta 1 integrins. FASEB J 2001; 15: 1389–1397.
Khan KMF, Falcone DJ . Role of laminin in matrix induction of macrophage urokinase-type plasminogen activator and 92-kDA metalloproteinase expression. J Biol Chem 1997; 272: 8270–8275.
Abu El-Asrar AM, Van Aelst I, Al-Mansouri S, Missotten L, Opdenakker G, Geboes K . Gelatinase B in vernal keratoconjunctivitis. Arch Ophthalmol 2001; 119: 1505–1511.
Acknowledgements
The authors thank Ms Christel Van den Broeck, for technical assistance, and Mrs Connie B. Unisa-Marfil and Mrs Bernice Bilson for secretarial work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abu El-Asrar, A., Meersschaert, A., Al-Kharashi, S. et al. Immuno-histochemical evaluation of conjunctival remodelling in vernal keratoconjunctivitis. Eye 17, 767–771 (2003). https://doi.org/10.1038/sj.eye.6700453
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700453