Abstract
Purpose To evaluate the compression characteristics of the human lens nucleocortex in relation to its LOCSIII clinical grading.
Methods Sixteen subjects undergoing planned extracapsular cataract surgery had pre-operative slit-lamp examination and assessment of cataract LOCSIII grade followed by postoperative in vitro evaluation of the nucleus with measurement of ‘linear compressibility’ by a purpose-designed caliper incorporating a strain gauge, enabling the derivation of a graph of nuclear compression (D (mm) against applied force (F (N)).
Results Nuclear colour correlates with the force required to compress a lens to 75% of its original depth (F75) (R = 0.625, P = 0.017). Nuclear opalescence correlates with the force required to compress a lens to 75% of its original depth (R = 0.651, P = 0.012) and inversely with linear compressibility (ΔD/ΔF, the slope of the graph of nuclear compression against applied force) (R = −0.610, P = 0.014). F75 is a direct and linear compressibility is an inverse related parameter of lens nucleus ‘hardness’.
Conclusion A new instrument is described which allows measurement of ‘hardness’-related compression characteristics of the human cataract in vitro. There is a relationship between the LOCSIII clinical classification of nuclear cataracts and mechanical compression characteristics of the cataractous lens. LOCSIII classification may aid the preoperative planning of an appropriate surgical approach to an individual cataract.
Similar content being viewed by others
Introduction
Phacoemulsification has become the technique of first choice for cataract surgery in the developed world. Advantages over extracapsular cataract extraction (ECCE) include faster rehabilitation, fewer or no suture-related problems, and less astigmatism.
It is only recently that final best-corrected acuity has been shown to be better in phaco surgery than ECCE.1 However, the visual outcome of a complicated phacoemulsification procedure or a phacoemulsification to ECCE conversion may be worse than that of an elective ECCE.
The hardness of the lens is a major contributing factor to the surgical difficulty in some of these cases. Preoperative knowledge of lens hardness would be helpful in planning a surgical approach to minimise the risk of complications.
We have previously reported the correlation of hardness with lens classification. This study used a lens guillotine, and Lens Opacities Classification System II (LOCSII). A new instrument that measures lens dimensions under standard conditions was designed and is described below. This instrument can be used to investigate the resistance of the extracted cataract to compression along its anterior-posterior (A–P) diameter. Distinct from hardness, though related to it, this characteristic might be important in the behaviour of the cataract during surgery.
Definition of mechanical characteristics of the lens
Mechanical properties of matter have strict definitions in engineering terms, but different related properties may each contribute to how a tissue behaves during surgery.
Hardness is the resistance of a material to penetration by a pointed tool. Hardness of a material is inversely related to its compressibility. The harder a lens, the less it will be compressed by a given force, and the lower its compressibility. Compressibility (C) is proportional to change in volume (V) divided by original volume and inversely proportional to change in applied pressure (P).

The term ‘hardness’ is used in this paper to represent a number of characteristics of the lens related to but distinct from hardness as defined by the mechanical definition above.
Stiffness of a material is the ratio between the force applied to the material and the deflection produced by that force, and is related to its hardness.
Stiffness of a material is also inversely proportional to its elasticity. Elasticity is a property of a material which enables it to regain its original shape and dimensions when force is removed. Elasticity is defined by Young’s modulus (E), stress over strain, where strain is change in thickness (ΔD) divided by original thickness (D), and stress is force of compression (F) over area of compression (A). According to Hooke’s law, the stress in a material is proportional, within certain limits, to the strain producing it. Outside these limits permanent deformation of the material may occur.

For the purpose of the current study linear compressibility is defined as the slope of the plot of change in thickness divided by change in force (ΔD/ΔF). Where area of compression and original thickness of the lens are constant this ratio is inversely proportional to stress over strain, and therefore represents a parameter proportionate to elasticity of the material and compressibility of a lens. It is inversely related to stiffness and may be considered a parameter inversely related to ‘hardness’ of the lens.
The force required to compress the lens to 75% of its original depth (F75) is also considered a parameter related to stiffness or ‘hardness’ of the lens, as long as it lies within the elastic limits of the lens. Although diseased lenses were studied, a deformation of 25% in thickness was considered to be unlikely to be outside the elastic limits. Figure 1 is representative, demonstrating that F75 lies on the linear portion of the compression graph for the illustrated lens. F75 is inversely correlated with the linear compressibility.
Linear compressibility and F75 are parameters that are measured by the lens ‘hardness’ (linear compressibility) device.
This paper seeks to identify the preoperative characteristics of the lens correlating with the mechanical characteristics of the nucleus, and to describe a new instrument with which such mechanical characteristics can be measured.
Materials and methods
A pilot study was undertaken on encapsulated lenses of donor eyes and nucleocortex of patients undergoing planned extracapsular cataract surgery or phaco-ECCE conversions. This allowed testing of instrumentation, evaluation of repeatability of measurements on lenses, determination of the order of measurements, and optimum time to measurement.
At the time of recruitment for the study (March–June 1998), it was appreciated that the phacoemulsification technique of cataract surgery allowed faster visual rehabilitation, and this was expressed to the patients. Patients were told that the results were awaited of the outcomes of the National Cataract Audit1 and randomised controlled studies comparing phacoemulsification with ECCE, but in the experience of the authors visual outcomes and complication rates were similar. The authors did not feel it unethical to perform ECCE surgery in a unit also performing phacoemulsification since many of the patients had specific indications for ECCE (see Table 1). Others had had first eye ECCE surgery and were very pleased with the result, and one of the surgeons in the department held ECCE as his procedure of choice. Ethics committee approval for the study was granted by the local research ethics committee. The main study was performed prospectively on lenses of 16 patients undergoing planned standard ECCE technique. Informed consent was obtained from all patients.
The nucleocortex was transferred to a container of Balanced Salt Solution for subsequent measurement within 3 h (although the pilot study suggested that measurements had a high degree of repeatability after several days, agreeing with other authors’ experience).2
Instrumentation
Lens ‘hardness’ device
An instrument for measuring parameters related to the ‘hardness’ or stiffness of lens nuclei was developed (Figure 2). This comprises a calibrated caliper with electronic strain gauge measuring the force resisting compression (0.01 mm intervals and 0.01 newton (N) intervals, respectively). A Perspex baseplate incorporates a shallow dished lens retainer. Parallel movable jaws restrain lens movement in the horizontal direction. The distance between the jaws is adjustable with a lead screw. A potentiometer is attached to the moving jaws in order to measure separation distance, which is indicated by an electronic digital readout. A strain gauge is attached to one of the jaws, and an electronic pressure monitor indicates the applied force.
Lens ‘hardness’ device. (a) Arms of the perspex device (left) have integrated sensors to determine force of compression and lens dimensions. Cataract is seen in the nucleus well. Digital display of cataract dimensions is seen on the right. (b) Electronic pressure monitors are seen on the right. (c) Schematic representation of lens ‘hardness’ device.
A gantry constructed adjacent to the lens well supports an arm with an in-built strain gauge. A force-applying 3.5 mm Perspex rod extends downwards directly over the lens well. The height of the arm is adjustable and a second potentiometer allows height to be indicated on the electronic caliper display, the applied force being indicated on a second electronic pressure monitor.
With this instrument it is possible to measure linear compressibility in both horizontal and vertical directions. In this study it was decided to evaluate the latter only, ie changes in the anterior to posterior (A–P) diameter, depth or thickness of the nucleus with applied force.
Measurements taken In vivo
-
1
Preoperative Lens Opacities Classification III (LOCSIII) grade.3
-
2
Biomicroscopic assessment of nuclear size: For this study, the method of assessment involved alignment of the vertical slit beam to be incident on the eye at 45°, with the patient instructed to look forwards, and the observer viewing stereoscopically. The beam height was increased until the height of the slit beam appeared to be equal to the apparent horizontal extent of the slit beam through the nuclear part of the lens. The measurement of the slit beam height was read off the scale to the nearest 0.1 mm. Correction was made neither for magnification nor for angle of incidence, as it was proposed to examine correlation between this measurement and the physical size of the nucleus, not compare them directly.
In vitro
-
1
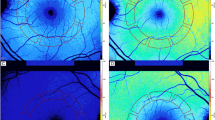
Assessment of linear compressibility: Physical measurements of nuclear dimensions, taken at increasing applied force, giving a plot of applied force F in newtons (N), against nuclear compression D in millimetres (mm) (Figure 3). The data derived from the current study, plotted in graphical form, represent a good fit to a straight line for each lens. The slope of this line, which for the purpose of this study is called linear compressibility, is a parameter inversely related to stiffness or ‘hardness’ of the lens. In simple terms a soft lens can be compressed more than a hard lens by a given force. Measurements were repeated to confirm that they were being taken in the range of elasticity of the lens, and to confirm that the act of compression of the lens during measurement was not altering the properties of the lens (Figure 4 illustrates this for a typical lens).
Figure 3 -
2
Measurement of the force (F75) required to compress the lens to 75% of its original A–P diameter. This is a parameter directly related to lens stiffness or ‘hardness’.
For the purposes of correlation between the physical and ultrasound characteristics of the lenses in vivo, A-scan biometry, and in vitro ultrasound assessment of the nuclei were also made (unpublished data, subject of future papers).
Statistical analysis
Statistical analysis was performed using Microsoft Excel, and Graphpad Instat computer software. Correlation coefficients and statistical tests of significance were used to relate data sets. Comparisons of interest were prospectively planned, and multiple comparisons were found to be significant at least at the 5% level. No correction for multiple comparisons was deemed necessary.
Results
Patient ages ranged from 60 to 90 years (mean 74.8 years, SD 8.0 years). Cataract type was simple in 12 cases: one was post-vitrectomy, one was in a diabetic, one was associated with steroid use and one was associated with both a history of trauma and pseudoexfoliation.
Full preoperative LOCSIII and biomicroscopic evaluation was possible in 15 of 16 patients. Maturity of one mature white lens precluded LOCSIII nucleus assessment; another mature lens allowed evaluation of nuclear colour and opalescence despite a white cortex. All lenses underwent measurement of lens linear compressibility. For each lens data strongly fitted a straight line. R2 values ranged from 0.721 (lens 12) to 0.993 (lens 16) (mean 0.902, SD 0.086). For clarity, the data for the 16 lenses are shown on four separate graphs (Figure 3).
Force to compress the lens to 75% of its original A–P dimension could not be measured in one lens due to lens crush.
Table 1 illustrates clinical in vivo and in vitro data for each lens.
Analyses
Linear compressibility and force required to compress the nucleus to 75% of its original anterior–posterior diameter
It was confirmed that the two mechanical characteristics of the lens used in the present study, namely linear compressibility and F75, were correlated with each other (R = −0.718, R2 = 0.516, P = 0.003).
Nuclear size and linear compressibility
A negative correlation was found between linear compressibility and in vitro nuclear size (R = −0.706, R2 = 0.498, P = 0.002), suggesting that the larger nuclei are ‘harder’ nuclei. It was a surprising finding that clinically it was not easy at the slit lamp to accurately assess nuclear size in all cases. There was in fact a negative correlation between this assessment and that of measured extracted nucleus (R = −0.713, R2 = 0.509, P = 0.003).
Mechanical characteristics of the lens and LOCSIII
An inverse correlation was found between linear compressibility and the nuclear opalescence (R = −0.610, R2 = 0.372, P = 0.014) and nuclear colour (R = −0.423, R2 = 0.179, P = 0.116) scores on LOCSIII scales, though the latter did not reach statistical significance. The force required to compress the lens to 75% of its original A–P diameter was, however, significantly correlated with nuclear opalescence (R = 0.651, R2 = 0.423, P = 0.012), and nuclear colour (R = 0.625, R2 = 0.390, P = 0.017). Neither cortical lens opacity (R2 = 0.179, P = 0.185) nor posterior subcapsular (R2 = 0.021, P = 0.610) grading showed a significant correlation with linear compressibility. There was a high positive correlation between nuclear opalescence and nuclear colour scores (R = 0.794, R2 = 0.631, P = 0.0004) agreeing with the findings of other workers that these features are associated.4
Age
Unlike previous work, this study found a positive relationship neither between age and LOCSIII grading, nor between age and size or mechanical characteristics of the cataract. The correlation coefficient for the relationship between age and nuclear opalescence was R = −0.344 (R2 = 0.119, P = 0.21), and that for the relationship between age and nuclear colour was R = −0.353 (R2 = 0.124, P = 0.196). There was a significant correlation neither between age and nuclear size (R = 0.191, R2 = 0.037, P = 0.476) nor between age and linear compressibility (R = −0.01, R2 = 0.0001, P = 0.972).
Discussion
On the basis of this and on previous research it is found that larger nuclei tend to be harder nuclei. However, clinically it was not easy at the slit lamp to accurately assess nuclear size. In two patients assessment of nuclear size was not possible due to mature lens opacity, or small pupil. In others it appeared that in particular ‘softer’ lens nuclei were overestimated in size. Slit lamp estimation of nuclear size is therefore not a good guide to ‘hardness’. Other preoperative correlates of ‘hardness’ are therefore required.
Further evidence is presented for the link between the preoperative LOCS grading, and in vitro parameters of lens ‘hardness’: This study confirms the findings of our group and others that in vivo nuclear colour and nuclear opalescence are related to nuclear ‘hardness’.5,6,7,8,9,10,11
Previous studies including those of our group have used automated lens guillotines to measure hardness.5,6,7,8,9 A criticism of this technique is that measurement in this way might be affected by friction between the instrument penetrating the lens and the lens structure. This criticism is also partly valid for the elegant devices described by Pau (probe and dynamometer)10 and Czygan and Hartung (penetrating indenter).2,11 The hardness of a lens is likely to change throughout the lens. Another criticism specifically of the lens guillotine is that the parameter used to denote hardness, the weight of fluid required to divide a nucleus into two, cannot reflect these changes. The instrument described in this paper is able to measure changing resistance to deformation of a lens or stiffness throughout the lens.
The data from the present study, using the new instrument, did not require mathematical transformation to enhance best fit to a straight line. For each lens the data fitted a straight line well. The expected graphical form derived for a lens of uniform density would indeed be expected to be linear (Figure 5a). Deviations from a straight line might be expected at the commencement of compression where the whole area of the force-applying Perspex rod may not be touching the lens, or due to non uniformity of the lens ‘hardness’. Typical lenses might be expected to have a gradually decreasing ‘hardness’ from nucleus outward, and the resultant force against compression graph may show a logarithmic decrease in slope (Figure 5b). If the centre of the lens has become very different in ‘hardness’ from the surrounding epinucleus a different graph shape would be seen (Figure 5c). Where the data deviate from a straight line, for example in lens 3 (Figure 3), this may be explained by differences in ‘hardness’ within the cataract.
The instrument used in the present study is more appropriate than a lens guillotine if discontinuities in ‘hardness’ are present. This technique is more likely to be able to determine or confirm such variations in ‘hardness’ through the lens than lens guillotine devices. Should the slope of the graph change throughout compression of the lens, linear compressibility can be measured for the portion of the graph of interest.
Due to the small numbers of lenses in the present study, differential hardness within a single lens was not measured by this study, and analysis was limited to the mean slope of the measurements for each cataract. This may reduce the accuracy of assessments of linear compressibility in this series.
Previous studies relating ‘hardness’ with nuclear appearance have all used various colour reference scales, or other lens classification systems. Although many such classifications have been published, one of the most popular in the past has been the LOCSII12 scale used by our group5,6,9 and those of Gullapalli et al7 and Assia et al.8
The LOCSIII grading system was chosen in preference to the LOCSII scale used previously by our group. The former has superseded the latter. It has the advantages of linear progression, can be used at the slit lamp13 and has a high degree of repeatability,3 in addition to being internationally recognised, and available from the authors to any interested groups. This study is the first to have confirmed the relationship between the physical characteristics of a cataract and its preoperative grading using the LOCSIII scale.
Although photographic image analysis densitometry,14,15,16,17 or digital image analysis18,19,20 as it becomes more widespread, might provide some more objective measures to enhance our preoperative assessment of cataracts and facilitate studies on progression of lens opacities,21 the LOCSIII and other cataract grading systems have been shown to have high inter-observer and intra-observer repeatability13,18,22,23,24 and to demonstrate some consistency between different classifications.24,25,26,27 New techniques such as photon spectroscopy for in vivo analysis of lenses remain to be further investigated.28
Other workers have studied in vitro features such as size,29 chemical,30,31 dielectric properties32 or histological appearance33 of lenses and linked them with preoperative features such as nuclear colour, but have not examined nuclear hardness. Assia et al8 examined the link between histological appearance and nuclear hardness, but found no relationship when simple staining techniques were used.
The numbers of lenses in the present series was too small to determine whether maturity of lenses per se was associated with nuclear ‘hardness’, though both the mature lenses in this series were among the ‘hardest’ cataracts. Other workers have suggested that slit lamp biomicroscopic features of intralenticular pressure, cortical status and nuclear colour can aid in consistently planning phaco surgery in mature lenses.6,34 At least one group, however, has questioned the reliability of clinical grading of nuclear cataract in the presence of increasingly severe cortical and posterior subcapsular cataract.35
Conclusions
We have described the use of a new instrument in measuring mechanical parameters of the lens closely related to stiffness or ‘hardness’. We conclude that nuclear colour and opalescence as measured using the LOCSIII clinical classification of cataracts are useful indicators of the mechanical characteristics of the lens. We recommend that these two features of the LOCSIII classification should feature prominently in the preoperative assessment of cataract. We suggest the LOCSIII classification of cataracts may aid the preoperative planning of an appropriate surgical approach to an individual cataract.
References
Desai P, Minassian DC, Reidy A . National cataract surgery survey 1977–8: a report of the results of the clinical outcomes. Br J Ophthalmol 1999; 83: 1336–1340
Czygan G, Hartung C . Mechanical testing of isolated senile human eye lens nuclei. Med Eng Phys 1996; 18: 345–349
Chylack LT Jr, Wolfe JK, Singer DM, Leske MC, Bullimore MA, Bailey IL et al. The Lens Opacities Classification System III. Arch Ophthalmol 1993; 111: 831–836
Thompson JR, Deane JS, Hall AB, Rosenthal AR . Associations between lens features assessed in the Oxford Clinical Cataract Classification and Grading System. Ophthalmic Epidemiol 1997; 4: 207–212
Heyworth P, Thompson GM, Tabandeh H, McGuigan S . The relationship between clinical classification of cataract and lens hardness. Eye 1993; 7: 726–730
Tabandeh H, Thompson GM, Heyworth P . Lens hardness in mature cataracts. Eye 1994; 8: 453–455
Gullapalli VK, Murthy PR, Murthy KR . Colour of the nucleus as a marker of nuclear hardness, diameter and central thickness. Ind J Ophthalmol 1995; 43: 181–184
Assia EI, Medan I, Rosner M . Correlation between clinical, physical and histopathological characteristics of the cataractous lens. Graefes Arch Clin Exp Ophthalmol 1997; 235: 745–748
Tabandeh H, Thompson GM, Heyworth P, Dorey S, Woods AJ, Lynch D . Water content, lens hardness and cataract appearance. Eye 1994; 8: 125–129
Pau H . The significance of brown coloration with regard to lens nuclear hardness in the case of extracapsular lens extraction. Ger J Ophthalmol 1992; 1: 139–141
Czygan G, Hartung C . On the correlation of mechanical and optical properties of cataractous eye lens nuclei. Biomed Tech 1997; 42: 2–6
Chylack LT Jr, Lesce MC, McCarthy D, Khu PM, Kashiwagi T, Sperduto R . Lens Opacities Classification System II. Arch Ophthalmol 1989; 107: 991–997
Karbassi M, Khu PM, Singer DM, Chylack LT Jr . Evaluation of lens opacities classification system III applied at the slitlamp. Optom Vis Sci 1993; 70: 923–928
Magno BV, Freidlin V, Datiles MB 3rd . Reproducibility of the NEI Scheimpflug Cataract Imaging System. Invest Ophthalmol Vis Sci 1994; 35: 3078–3084
Kashiwagi T, Khu PM . New method of measuring nuclear cataract in color Scheimpflug photographs. Ophthalmic Res 1990; 22 Suppl 1: 24–28
Khu PM, Kashiwagi T . Quantitating nuclear opacification in color Scheimpflug photographs. Invest Ophthalmol Vis Sci 1993; 34: 130–136
Sasaki K, Fujisawa K, Sakamoto Y . Quantitative evaluation of nuclear cataract using image analysis. Ophthalmic Res 1992; 24 Suppl 1: 26–31
Duncan DD, Shukla OB, West SK, Schein OD . New objective classification system for nuclear opacification. J Opt Soc Am A 1997; 14: 1197–1204
Garrett SK, Robman LD, McCarty CA, Thomas AP, McNeil JJ, Taylor HR . Reproducibility of automatic standard digital analysis of lens opacities. Aust NZ J Ophthalmol 1998; 26 Suppl 1: S29–S31
Robman LD, McCarty CA, Garrett SK, Stephenson H, Thomas AP, McNeil JJ, Taylor HR . Comparison of clinical and digital assessment of nuclear optical density. Ophthalmic Res 1999; 31: 119–126
Foo KP, Maclean H . Measured changes in cataract over six months: sensitivity of the Nidek EAS-1000. Ophthalmic Res 1996; 28 Suppl 2: 32–36
Panchapakesan J, Cumming RG, Mitchell P . Reproducibility of the Wisconsin cataract grading system in the Blue Mountains Eye Study. Ophthalmic Epidemiol 1997; 4: 119–126
Braccio L, Camparini M, Graziosi P, Baratta G, Ferrigno L, Williams SL et al. An independent evaluation of the Age-Related Eye Disease Study (AREDS) cataract grading system. Curr Eye Res 1998; 17: 53–59
Hall AB, Thompson JR, Deane JS, Rosenthal AR . LOCS III versus the Oxford Clinical Cataract Classification and Grading System for the assessment of nuclear, cortical and posterior subcapsular cataract. Ophthalmic Epidemiol 1997; 4: 179–194
Chylack LT Jr, Wolfe JK, Friend J, Khu PM, Singer DM, McCarthy D et al. Quantitating cataract and nuclear brunescence, the Harvard and LOCS systems. Optom Vis Sci 1993; 70: 886–895
Rouhiainen P, Rouhiainen H, Notkola IL, Salonen JT . Comparison of the lens opacities classification system II and Lensmeter 701. Am J Ophthalmol 1993; 116: 617–621
Taylor HR, Lee JA, Wang F, Munoz B . A comparison of two photographic systems for grading cataract. Invest Ophthalmol Vis Sci 1991; 32: 529–532
Bursell SE, Baker RS, Weiss JN, Haughton JF, Rand LI . Clinical photon correlation spectroscopy evaluation of human diabetic lenses. Exp Eye Res 1989; 49: 241–258
Ayaki M, Ohde H, Yokoyama N . Size of the lens nucleus separated by hydrodissection. Ophthalmic Surg Lasers 1993; 24: 492–493
Bhat KS, John A, Reddy PR, Reddy PS, Reddy VN . Effect of pigmentation on glutathione redox cycle antioxidant defense in whole as well as different regions of human cataractous lens [published erratum appears in Exp Eye Res 1992; 54: 317]. Exp Eye Res 1991; 52: 715–721
Mota MC, Ramalho JS, Carvalho P, Quadrado J, Baltar AS . Monitoring in vivo lens changes. A comparative study with biochemical analysis of protein aggregation. Doc Ophthalmol 1992; 82: 287–296
Matsuoka R, Watanabe M, Ueno H . [A study of coloring in human lens nucleus-association of four inorganic elements and dielectric behavior with nuclear color]. [Japanese] Nippon Ganka Gakkai Zasshi 1997; 101: 359–364
Jongebloed WL, Kalicharan D, Los LI, Worst JG . Study of the substructure of the Morgagni and Brunescens cataract with the TAO non-coating technique. Part 2: Brunescens cataract. Doc Ophthalmol 1992; 82: 161–168
Basti S . Different faces of the white cataract: a phaco surgeon’s perspective. Aust NZ J Ophthalmol 1999; 27: 53–56
Maraini G, Pasquini P, Sperduto RD, Bonacini M, Carrieri MP, Corona R et al. The effect of cataract severity and morphology on the reliability of the Lens Opacities Classification System II (LOCS II). Invest Ophthalmol Vis Sci 1991; 32: 2400–2403
Acknowledgements
The authors wish to thank Mr Don Ritchie, Mr Ron Clarke and Mr Ian Eversden for their technical support, Dr ALT Killingback for help with analyses, Professor JM Bland for statistical advice and Mr Irving K Luke for supplying nuclei.
Author information
Authors and Affiliations
Corresponding author
Additional information
Proprietary interest: None Presented as a poster at the Royal College of Ophthalmologists Annual Congress, Harrogate, May 2000
Rights and permissions
About this article
Cite this article
Smith, J., El-Brawany, M., Nassiri, D. et al. The relationship between nuclear colour and opalescence on the LOCSIII scale and physical characteristics of cataract nuclei. Eye 16, 543–551 (2002). https://doi.org/10.1038/sj.eye.6700119
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700119
Keywords
This article is cited by
-
Application of prechop technique in phacoemulsification for cataract patients with highly liquefied vitreous: a retrospective study
BMC Ophthalmology (2022)
-
Corneal endothelial function after phacoemulsification using the fluid-based system compared to conventional ultrasound technique
Eye (2007)
-
Stiffness gradient in the crystalline lens
Graefe's Archive for Clinical and Experimental Ophthalmology (2007)