Abstract
Background:
Putative breast cancer stem cells might express surface markers such as aldehyde dehydrogenase 1 (ALDH1) and BMI-1 proteins. The aim of this study was to explore the expression of these proteins in breast cancers from an African population and their associations with the basal-like phenotype (BLP) and other molecular characteristics.
Methods:
We analysed 192 paraffin-embedded breast carcinoma samples by tissue microarrays and immunohistochemical methods.
Results:
In total, 88 tumours (48%) expressed ALDH1, whereas 46 (25%) expressed BMI-1 protein. Expression of ALDH1 was associated with high histological grade (P<0.0005), high mitotic count (P<0.0005), high nuclear grade (P<0.0005), oestrogen receptor (ER) negativity (P<0.0005), progesterone receptor (PR) negativity (P=0.009), p53 expression (P=0.034), cytokeratin 5/6 positivity (P=0.008), epidermal growth factor receptor (EGFR) expression (P=0.015) and the BLP (P<0.0005), whereas it was inversely associated with BMI-1 staining (P=0.009). On the other hand, BMI-1 expression was associated with low histological grade (P=0.004) and ER positivity (P=0.001).
Conclusion:
There was a high prevalence of ALDH1 expression among breast carcinomas and associations with basal markers and features of aggressive tumours. Studies are required to elucidate the importance of these findings for improved understanding of breast cancer biology.
Similar content being viewed by others
Main
Human breast cancers have been reported to contain a sub-population of cancer cells similar to epithelial stem cells (Hamburger and Salmon, 1977; Al-Hajj et al, 2003; Abraham et al, 2005). These cells have the ability to self-renew and undergo differentiation to phenotypically diverse populations of tumour cells (Al-Hajj et al, 2003). It has been suggested that cancer stem cells drive the growth and spread of malignant tumours (Al-Hajj et al, 2003), and the stem cell hypothesis might have important implications for clinical management (Ginestier et al, 2007; Tanei et al, 2009).
The molecular diversity and subclassification of breast cancers have been reported in several studies during recent years (Perou et al, 2000; Sorlie et al, 2003; Rakha et al, 2008). Five tumour subgroups with different prognosis and response to adjuvant therapy have been identified. Of these, the basal-like and HER2 subtypes are of particular interest as both have a poor prognosis (Sorlie et al, 2001; Yang et al, 2007). The basal-like phenotype (BLP) is characterised by the expression of basal cell markers, and it overlaps with the triple-negative phenotype (TNP; ER−/PR−/HER2−) (Tischkowitz et al, 2007). It was reported that basal-like and BRCA1-associated breast carcinomas, which are also related (Foulkes et al, 2003) were both enriched with CD44+/CD24− candidate stem cells (Honeth et al, 2008), and BRCA1 has been suggested to represent a stem cell regulator (Foulkes, 2004).
Previous studies indicate that stem cell-like populations in breast tissue are characterised by the expression of aldehyde dehydrogenase 1 (ALDH1), and breast cancer stem cells were isolated on the basis of increased ALDH1 expression (Ginestier et al, 2007). Thus, in the breast, expression of ALDH1 is considered to be a marker of both normal and malignant stem and progenitor cells (Ginestier et al, 2007). In established breast cancers, ALDH1 expression has been associated with poor clinical outcome (Ginestier et al, 2007) and resistance to chemotherapy (Sladek et al, 2002; Tanei et al, 2009). Furthermore, studies have indicated that human breast cancers and cell lines contain a sub-population of cells characterised by CD44+/CD24−/low/Lin− cell surface markers, and a partial overlap between CD44+/CD24−/low/Lin− and ALDH1-positive populations was reported (Al-Hajj et al, 2003; Ginestier et al, 2007; Fillmore and Kuperwasser, 2008). It is noteworthy that putative cancer stem cells expressing the combined CD44+/CD24−/low/ALDH1+ phenotype showed an especially high tumourigenic capacity, being able to form tumours from as few as 20 cells (Ginestier et al, 2007).
The importance of BMI-1, a transcriptional repressor of the polycomb group of transcription factors (Alkema et al, 1993) and a key regulator of self-renewal in both normal and malignant stem cells (Liu et al, 2006), has been more controversial. Still, BMI-1 has been linked to mammary carcinogenesis in some previous studies (Dimri et al, 2002; Datta et al, 2007). Although some find BMI-1 expression to be associated with a favourable prognosis (Kim et al, 2004; Arnes et al, 2008; Choi et al, 2009), others have reported the opposite (Glinsky et al, 2005; Silva et al, 2007).
Breast cancers in African populations and among African Americans seem to be more aggressive than breast cancers in Caucasians (Ikpatt et al, 2002; Jones et al, 2004), and better insight about differences in tumour characteristics (Porter et al, 2004; Fregene and Newman, 2005; Morris et al, 2007; Bird et al, 2008) may suggest strategies to improve clinical management among Africans. In general, there is some evidence that the limitation of chemotherapy and radiation treatment may be associated with the inability to target breast cancer stem cells (Phillips et al, 2006; Fillmore and Kuperwasser, 2008; Li et al, 2008; Tanei et al, 2009), and the efficacy of HER2 inhibitors may relate to their influence on stem cell populations in HER2-positive tumours (Korkaya et al, 2008).
On this background, the purpose of our study was to examine the expression of candidate stem cell markers ALDH1 and BMI-1 in breast cancer in relation to basal-like markers, other molecular features and clinicopathological phenotype. These markers were examined in tumours from an African population in which breast cancer is assumed to be more aggressive and also associated with frequent basal-like differentiation (Nalwoga et al, 2007). In these populations, early diagnosis and effective treatment is especially challenging (Gakwaya et al, 2008).
Materials and methods
Patient series
Cases of primary breast carcinoma with available and technically suitable archival paraffin blocks from the period 1990 to 2002 were identified in the Kampala Cancer Registry at the Department of Pathology, Makerere University College of Health Sciences, Kampala (Uganda). The Registry serves an area of about 1914 km2, which comprises of Kampala with neighbouring urban and semi-urban areas (Gondos et al, 2005) and an estimated population of 1.7 million in 2002 (Population Council, 2004). The population of females >15 years of age is about 530 000. The Baganda from the Central region is the largest ethnic group in the county, but other ethnic groups are represented. The registry methods of collecting data and results have been previously reported (Wabinga et al, 1993).
Altogether, 192 cases were included in the study, and 87 other cases with inadequate tissue available were excluded. Clinical information was obtained from the histology reports. The mean age was 46.2 years (range 18–80 years). Duration of symptoms as reported by 127 patients at the time of presentation was 17.1 months on average (median 9 months; range 0.5–108 months). The cutoff point for long duration was 9 months (median value). Stage of disease at the time of diagnosis was available in only 22 patients; the majority (n=12) were in stage 4, 8 (36%) were in stage 3, whereas stage 1 and 2 contributed 9%. All cases were re-examined histologically (by HN and JBA) and classified according to the World Health Organisation (Tavassoli and Devilee, 2003) and histological grading was performed in accordance with the Nottingham criteria (Elston and Ellis, 1991). Nuclear grade and mitotic count was also recorded as separate variables according to the same criteria. The permission to conduct this research was obtained from the Research Ethical Committee at Makerere University College of Health Sciences.
Tissue microarray
The tissue microarray (TMA) technique has been validated in several studies (Camp et al, 2000). TMA was performed on 192 cases using archival tissues of invasive breast carcinomas according to Kononen et al (1998). Representative tumour areas were identified on haematoxylin and eosin-stained slides, and a minimum of three tissue cylinders (diameter 1 mm) were punched from selected areas of the donor block and mounted into the recipient paraffin block using a custom-made precision instrument (Beecher Instruments, Silver Spring, MD, USA). Sections of 5 μm thickness of the resulting TMA blocks were made by standard technique.
Immunohistochemistry
The TMA sections were stained with antibodies as shown in Table 1. Sections were deparaffinised in xylene, rehydrated through a series of graded alcohols and rinsed in distilled water. Antigen retrieval based on microwave oven heating with retrieval buffer at 750 W for 10 min followed by 350 W for 15 min (an extra 5 min at 350 W was added for p53, p63 and BMI-1, and 15 min for Ki-67) was used for all antibodies, except epidermal growth factor receptor (EGFR) for which proteinase predigestion for 10 min was applied. Tris–EDTA pH 9.0 retrieval buffer was used for all markers except ALDH1 for which citrate buffer pH 6.0 was used. Sections were allowed to cool at room temperature for 20 min and then thoroughly rinsed in buffer solution and placed in the Dako Autostainer (DakoCytomation, Glostrup, Denmark) for staining. Endogenous peroxidase activity was blocked by incubating sections with 0.03% hydrogen peroxidase containing sodium azide for 5 min, followed by rinsing with buffer solution. Then sections were incubated with specific antibodies at room temperature. Regarding antibodies, P-cadherin and ALDH1 were obtained from BD Biosciences (Oxford, UK), mouse anti-EGFR was obtained from Zymed Laboratories (San Francisco, CA, USA), and BMI-1 was produced as previously described (Arnes et al, 2008), whereas all other antibodies were obtained from DakoCytomation A/S. All antigens were detected by the DakoCytomation EnVision+ system-horseradish peroxidase for 30 min, except BMI-1 for which the CSA II kit (DakoCytomation) was used. After rinsing the sections in buffer solution, we developed the peroxidase by incubating with freshly prepared 3,3′-diaminobenzidine chromogen solution for 10 min. Sections were then rinsed in distilled water and counterstained with Meyer's haematoxylin. Cases of breast or colonic carcinoma previously known to be positive for the markers studied were used as positive controls. For c-kit, a gastrointestinal stromal tumour (GIST) was used.
Evaluation of staining
Tumours without interpretable cores (2.6–4.7%) because of insufficient tumour tissue were omitted from the analysis. A total of 183–187 cases could be evaluated for the various markers. The oestrogen receptor (ER), progesterone receptor (PR), HER2, EGFR, Ki-67, p53, p63, cytokeratin (CK) 5/6, P-cadherin, c-kit and BMI-1 were evaluated as previously described (Engelsen et al, 2006; Stefansson et al, 2006; Arnes et al, 2008; Nalwoga et al, 2008). Regarding ALDH1, cytoplasmic staining was evaluated, whereas nuclear staining alone was considered nonspecific and was not included in the analysis.
For BMI-1, a staining index (values 0–9) was determined by multiplying the score for intensity of staining (none=0, weak=1, moderate=2 and strong=3) with the score for proportion of tumour cells stained (<10%=1, 10–50%=2, >50%=3) (Arnes et al, 2008). The majority of cases (75%) had staining index 0, and therefore the cutoff was 0=negative and 1–9=positive. For ALDH1, the median staining index was 2, and the cutoff point was set at 0–2=negative and 3–9=positive. Ki-67 proliferative rate was determined as previously described (Nalwoga et al, 2007). The cutoff point for Ki-67 was set at 20.0% based on the median value for this series.
Molecular subtypes
There is no consensus on how to define different molecular subtypes of breast cancer by immunohistochemical markers, and overlapping categories exist. We used criteria on the basis of this literature (Carey et al, 2006; Yang et al, 2007; Sihto et al, 2008) for subclassification into molecular subtypes. In accordance with Carey et al (2006), we defined the luminal A (ER+ and/or PR+, HER2−), luminal B (ER+ and/or PR+, HER2+), HER2+ subtype (ER−, PR−, HER2+) and the basal-like subtype (ER−, HER2− and CK 5/6+ and/or EGFR+) subgroups. Tumours negative for all the five markers (ER, PR, HER2, CK 5/6 and EGFR) were considered as unclassified. This definition for luminal B tumours does not identify all luminal B tumours because only 30–50% are HER2+ and the rest are classified with the luminal A. We therefore merged luminal A and luminal B into the luminal subtype. Further, in accordance with our previous studies, we included P-cadherin staining in the definition of BLP (Nalwoga et al, 2007; Arnes et al, 2008). Using the Arnes et al (2008) criteria, we defined BLP profiles as follows: BLP1: concurrent ER−, HER2− and CK 5/6+; BLP2: concurrent ER−, HER2− and P-cadherin+; BLP3: concurrent ER−, HER2− and EGFR+; BLP4: concurrent ER−, HER2− and CK 5/6+ and/or EGFR+; BLP5: concurrent ER−, HER2− and positivity for one or more basal markers (CK 5/6, P-cadherin and EGFR). BLP4 is identical to the core basal phenotype as defined by Nielsen et al (2004) and Tischkowitz et al (2007).
Statistical analysis
Statistical analysis was performed using the SPSS version 15.0 software (SPSS Inc, Chicago, IL, USA). We examined the association between ALDH1 and BMI-1 expression with other tumour characteristics using χ2-test and Fisher's exact test. The t-test was used to detect the differences in average age between groups. A P-value of <0.05 was considered significant for any statistical test used.
Results
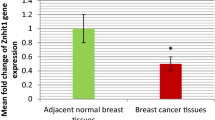
In all, 88 tumours (48%) were positive for ALDH1, whereas 95 (52%) were negative for ALDH1 (Figure 1). The majority (62%) of ALDH1-positive cases were high-grade ductal carcinomas. Altogether, 40 cases (46%) showed staining in >10% of the tumour cells, whereas 16 of 88 (18%) cases had a diffuse staining in ⩾50% of the tumour cells. Overall, the expression of ALDH1 seemed to be evenly distributed throughout the tumour cell population, although there were some cases with clusters of positively stained cells within the diffuse pattern. The average percentage of stained tumour cells in positive cases was 18%. Of the ALDH1-positive tumours, 31% were of the luminal subtype (27.3% luminal A, 3.4% luminal B), 31% had a basal-like subtype (core basal phenotype; BLP4), 16% were in the HER2 subtype and 23% were in the unclassified category. A majority (53%) of the ALDH1-positive cases were triple-negative tumours.
Table 2 shows ALDH1 expression and associations with clinicopathological characteristics. Patients with a shorter duration of symptoms were more likely to express ALDH1 than those with longer duration of symptoms (odds ratio 2.2; 95% confidence interval 1.05–4.5, P=0.036). The ALDH1 expression was significantly associated with markers of poor prognosis, such as high histological grade, high mitotic counts, high nuclear grade, ER negativity, PR negativity, and p53 expression. No associations were found between ALDH1 expression and HER2 status, p63 or c-kit positivity.
As shown in Table 3, CK5/6 was positive in 15%, P-cadherin in 27% and EGFR in 20% of all cases. One or more of these were positive in 33% of the cases (61 of 185). A total of 86 tumours (46%) were of the luminal subtypes (42%, luminal A, 4% luminal B), 22% (41 of 186) had a basal-like subtype, the HER2 subtype contributed 12% (23 of 186), and 19% (36 of 186) were in the unclassified group. Regarding the different BLP profiles, 15% (27 of 186) were BLP1, 22% (41 of 187) were BLP2, 17% (31 of 186) were BLP3, 22% (41 of 186) were BLP4 (core basal phenotype) and 26% (49 of 186) were BLP5. All tumours in the different BLP profiles were triple negative in this series. A majority of the triple-negative tumours showed basal-like differentiation; 53% (41 of 77) had a core basal profile (BLP4), whereas 64% (49 of 77) of the TNP tumours had positive expression of at least one of the three basal markers (CK5/6, P-cadherin, EGFR) combined with ER– and HER2–, corresponding to the BLP5 profile.
Table 3 also shows the relationship between ALDH1 positivity and molecular subtypes of breast cancer. The ALDH1 expression was significantly associated with molecular subtype and BLP profiles as defined in this paper, as well as with TNP and individual basal markers CK 5/6 and EGFR. Thus, the BLP, the HER2 subgroup and the unclassified category were more likely to express ALDH1 than the luminal subtypes.
In all, 46 tumours (25%) were positive for BMI-1 staining. The majority of cases (61%) were of the luminal subtype (54.3% luminal A, 6.5% luminal B), whereas the basal-like category contributed 22%, 11% were in the HER2 subgroup and 7% were unclassified. In total, 13 tumours (28%) were triple negative. The BMI-1 positivity was mostly associated with features of good prognosis, such as low histological grade (P=0.011), low mitotic counts (P=0.010) and ER positivity (P=0.001). Further, BMI-1 expression was inversely associated with the TNP (P=0.037) and with ALDH1 positivity (P=0.009). Tumours in the luminal subtype (odds ratio 5.4; 95% confidence interval 1.05–19.2, P=0.005) were more likely to express BMI-1 than unclassified tumours. No association was found between BMI-1 expression and the other subtypes, the basal markers such as CK5/6, P-cadherin, EGFR, and the BLP profiles.
Discussion
In this study, our aim was to explore the expression of candidate stem cell markers ALDH1 and BMI-1 in breast cancers from an African population and their possible associations with BLP and other molecular markers. We found that ALDH1 expression was associated with features of aggressive tumours such as high histological grade, high nuclear grade, high mitotic count, p53 expression and ER/PR negativity. In addition, ALDH1 expression was associated with a short duration of symptoms. Thus, ALDH1 status might represent an indicator of aggressive breast cancer (Ginestier et al, 2007; Morimoto et al, 2009). In support of this, others have suggested that the amount of cancer stem cells within breast tumours may correspond to the risk of distant metastases (Abraham et al, 2005; Glinsky et al, 2005).
It has been observed that basal-like breast cancers might be enriched with CD44+/CD24− cells (Honeth et al, 2008), and an overlap between CD44+/CD24− cells and ALDH1-positive cell populations were described (Ginestier et al, 2007). Moreover, the CD44+/CD24−/ALDH1+ phenotype identified a highly tumourigenic cell population that was able to form tumours from as few as 20 cells. Our results showed that ALDH1 was significantly associated with the basal-like subtype and different BLP profiles, as well as with individual basal markers CK 5/6 and EGFR, similar to what others have reported (Ginestier et al, 2007). To speculate, our findings might be related to the aggressive behaviour and therapy resistant features of the basal-like breast cancer subtype (Sorlie et al, 2001; Banerjee et al, 2006; Fillmore and Kuperwasser, 2008; Li et al, 2008). Moreover, we found a significant association between ALDH1 expression and the triple-negative tumours, a group whose poor prognosis has been widely reported (Dent et al, 2007).
Our findings indicate a higher frequency of ALDH1 expression (48%) in this series of breast cancer from an African population, compared with 19 and 30% in two different Caucasian populations described by Ginestier et al (2007). We also found more extensive staining in positive cases (Ginestier et al, 2007). Further, in comparison with data derived from breast tumours in Caucasian and Asian populations (Ginestier et al, 2007; Morimoto et al, 2009; Tanei et al, 2009) regarding ALDH1 positivity rate in tumours with similar characteristics (histological grade, ER, HER2, Ki-67), we observed that tumours from our present series stained in a higher percentage of cases in most poor prognosis categories (such as high histological grade, ER-negative cases, HER2-negative cases, tumours with high Ki-67 expression). Hence, apart from methodological discrepancies, biological differences might be present when comparing breast cancers from African and Caucasian populations (Elledge et al, 1994; Ikpatt et al, 2002; Jones et al, 2004; Porter et al, 2004). In line with this, a poorer outcome has been observed in African and African-American patients (Wojcik et al, 1998; Ikpatt et al, 2002) when compared with breast cancers among Caucasians, with differences in the spectrum of tumour characteristics and prognostic features such as the presence of tumour necrosis, low ER positivity rate, high HER2-positive rate, and a high frequency of basal-like features (Mbonde et al, 2001; Ikpatt et al, 2002; Carey et al, 2006; Nalwoga et al, 2006, 2007; Morris et al, 2007; Bird et al, 2008).
In contrast to our findings on ALDH1, the expression of BMI-1, another candidate stem cell marker (Arnes et al, 2008), was inversely associated with ALDH1 and related to features of good prognosis, such as low histological grade, low mitotic count, ER positivity and absence of TNP (Kim et al, 2004; Choi et al, 2009). This is in line with our recent studies of breast cancer (Arnes et al, 2008) and other tumours (Bachmann et al, 2008; Engelsen et al, 2008). The frequency of BMI-1 expression (25%) was lower than those found in other studies (43–62%) (Kim et al, 2004; Arnes et al, 2008; Choi et al, 2009). Others have found different results, BMI-1 expression being associated with more aggressive tumours (Glinsky et al, 2005; Silva et al, 2007). In addition, Glinsky et al (2005) found that expression of a BMI-1-driven 11 gene signature was associated with risk of metastases in breast carcinoma. The explanation for this inverse relationship is not known.
In conclusion, we observed a high prevalence of ALDH1 staining in this series of invasive breast carcinomas from Uganda. Expression of ALDH1 was significantly associated with a BLP and with features of aggressive tumours. Assessment of ALDH1 expression might help to identify a high-risk (Sreerama and Sladek, 1997) subgroup of breast cancers in this population. More studies are required to elucidate the possible significance of these stem cell markers in breast cancer patients.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Abraham BK, Fritz P, McClellan M, Hauptvogel P, Athelogou M, Brauch H (2005) Prevalence of CD44+/CD24−/low cells in breast cancer may not be associated with clinical outcome but may favor distant metastasis. Clin Cancer Res 11: 1154–1159
Al-Hajj M, Wicha MS, Benito-Hernandez A, Morrison SJ, Clarke MF (2003) Prospective identification of tumourigenic breast cancer cells. Proc Natl Acad Sci USA 100: 3983–3988
Alkema MJ, Wiegant J, Raap AK, Berns A, van Lohuizen M (1993) Characterization and chromosomal localization of the human proto-oncogene BMI-1. Hum Mol Genet 2: 1597–1603
Arnes JB, Collett K, Akslen LA (2008) Independent prognostic value of the basal-like phenotype of breast cancer and associations with EGFR and candidate stem cell marker BMI-1. Histopathology 52: 370–380
Bachmann IM, Puntervoll HE, Otte AP, Akslen LA (2008) Loss of BMI-1 expression is associated with clinical progress of malignant melanoma. Mod Pathol 21: 583–590
Banerjee S, Reis-Filho JS, Ashley S, Steele D, Ashworth A, Lakhani SR, Smith IE (2006) Basal-like breast carcinomas: clinical outcome and response to chemotherapy. J Clin Pathol 59: 729–735
Bird PA, Hill AG, Houssami N (2008) Poor hormone receptor expression in East African breast cancer: evidence of a biologically different disease? Ann Surg Oncol 15: 1983–1988
Camp RL, Charette LA, Rimm DL (2000) Validation of tissue microarray technology in breast carcinoma. Lab Invest 80: 1943–1949
Carey LA, Perou CM, Livasy CA, Dressler LG, Cowan D, Conway K, Karaca G, Troester MA, Tse CK, Edmiston S, Deming SL, Geradts J, Cheang MC, Nielsen TO, Moorman PG, Earp HS, Millikan RC (2006) Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA 295: 2492–2502
Choi YJ, Choi YL, Cho EY, Shin YK, Sung KW, Hwang YK, Lee SJ, Kong G, Lee JE, Kim JS, Kim JH, Yang JH, Nam SJ (2009) Expression of Bmi-1 protein in tumour tissues is associated with favorable prognosis in breast cancer patients. Breast Cancer Res Treat 113: 83–93
Datta S, Hoenerhoff MJ, Bommi P, Sainger R, Guo WJ, Dimri M, Band H, Band V, Green JE, Dimri GP (2007) Bmi-1 cooperates with H-Ras to transform human mammary epithelial cells via dysregulation of multiple growth-regulatory pathways. Cancer Res 67: 10286–10295
Dent R, Trudeau M, Pritchard KI, Hanna WM, Kahn HK, Sawka CA, Lickley LA, Rawlinson E, Sun P, Narod SA (2007) Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res 13: 4429–4434
Dimri GP, Martinez JL, Jacobs JJ, Keblusek P, Itahana K, Van Lohuizen M, Campisi J, Wazer DE, Band V (2002) The Bmi-1 oncogene induces telomerase activity and immortalizes human mammary epithelial cells. Cancer Res 62: 4736–4745
Elledge RM, Clark GM, Chamness GC, Osborne CK (1994) Tumour biologic factors and breast cancer prognosis among white, Hispanic, and black women in the United States. J Natl Cancer Inst 86: 705–712
Elston CW, Ellis IO (1991) Pathological prognostic factors in breast-cancer. 1. The value of histological grade in breast-cancer – experience from a large study with long-term follow-up. Histopathology 19: 403–410
Engelsen IB, Mannelqvist M, Stefansson IM, Carter SL, Beroukhim R, Oyan AM, Otte AP, Kalland KH, Akslen LA, Salvesen HB (2008) Low BMI-1 expression is associated with an activated BMI-1-driven signature, vascular invasion, and hormone receptor loss in endometrial carcinoma. Br J Cancer 98: 1662–1669
Engelsen IB, Stefansson I, Akslen LA, Salvesen HB (2006) Pathologic expression of p53 or p16 in preoperative curettage specimens identifies high-risk endometrial carcinomas. Am J Obstet Gynecol 195: 979–986
Fillmore CM, Kuperwasser C (2008) Human breast cancer cell lines contain stem-like cells that self-renew, give rise to phenotypically diverse progeny and survive chemotherapy. Breast Cancer Res 10: R25
Foulkes WD (2004) BRCA1 functions as a breast stem cell regulator. J Med Genet 41: 1–5
Foulkes WD, Stefansson IM, Chappuis PO, Begin LR, Goffin JR, Wong N, Trudel M, Akslen LA (2003) Germline BRCA1 mutations and a basal epithelial phenotype in breast cancer. J Natl Cancer Inst 95: 1482–1485
Fregene A, Newman LA (2005) Breast cancer in sub-Saharan Africa: how does it relate to breast cancer in African-American women? Cancer 103: 1540–1550
Gakwaya A, Kigula-Mugambe JB, Kavuma A, Luwaga A, Fualal J, Jombwe J, Galukande M, Kanyike D (2008) Cancer of the breast: 5-year survival in a tertiary hospital in Uganda. Br J Cancer 99: 63–67
Ginestier C, Hur MH, Charafe-Jauffret E, Monville F, Dutcher J, Brown M, Jacquemier J, Viens P, Kleer CG, Liu S, Schott A, Hayes D, Birnbaum D, Wicha MS, Dontu G (2007) ALDH1 is a marker of normal and malignant human mammary stem cells and a predictor of poor clinical outcome. Cell Stem Cell 1: 555–567
Glinsky GV, Berezovska O, Glinskii AB (2005) Microarray analysis identifies a death-from-cancer signature predicting therapy failure in patients with multiple types of cancer. J Clin Invest 115: 1503–1521
Gondos A, Brenner H, Wabinga HR, Parkin DM (2005) Cancer survival in Kampala, Uganda. Br J Cancer 92: 1808–1812
Hamburger AW, Salmon SE (1977) Primary bioassay of human tumour stem cells. Science 197: 461–463
Honeth G, Bendahl PO, Ringner M, Saal LH, Gruvberger-Saal SK, Lovgren K, Grabau D, Ferno M, Borg A, Hegardt C (2008) The CD44+/CD24− phenotype is enriched in basal-like breast tumours. Breast Cancer Res 10: R53
Ikpatt OF, Kuopio T, Ndoma-Egba R, Collan Y (2002) Breast cancer in Nigeria and Finland: epidemiological, clinical and histological comparison. Anticancer Res 22: 3005–3012
Jones BA, Kasl SV, Howe CL, Lachman M, Dubrow R, Curnen MM, Soler-Vila H, Beeghly A, Duan F, Owens P (2004) African-American/White differences in breast carcinoma: p53 alterations and other tumour characteristics. Cancer 101: 1293–1301
Kim JH, Yoon SY, Jeong SH, Kim SY, Moon SK, Joo JH, Lee Y, Choe IS, Kim JW (2004) Overexpression of Bmi-1 oncoprotein correlates with axillary lymph node metastases in invasive ductal breast cancer. Breast 13: 383–388
Kononen J, Bubendorf L, Kallioniemi A, Barlund M, Schraml P, Leighton S, Torhorst J, Mihatsch MJ, Sauter G, Kallioniemi OP (1998) Tissue microarrays for high-throughput molecular profiling of tumour specimens. Nat Med 4: 844–847
Korkaya H, Paulson A, Iovino F, Wicha MS (2008) HER2 regulates the mammary stem/progenitor cell population driving tumorigenesis and invasion. Oncogene 27: 6120–6130
Li X, Lewis MT, Huang J, Gutierrez C, Osborne CK, Wu MF, Hilsenbeck SG, Pavlick A, Zhang X, Chamness GC, Wong H, Rosen J, Chang JC (2008) Intrinsic resistance of tumourigenic breast cancer cells to chemotherapy. J Natl Cancer Inst 100: 672–679
Liu S, Dontu G, Mantle ID, Patel S, Ahn NS, Jackson KW, Suri P, Wicha MS (2006) Hedgehog signaling and Bmi-1 regulate self-renewal of normal and malignant human mammary stem cells. Cancer Res 66: 6063–6071
Mbonde MP, Amir H, Akslen LA, Kitinya JN (2001) Expression of oestrogen and progesterone receptors, Ki-67, p53 and BCL-2 proteins, cathepsin D, urokinase plasminogen activator and urokinase plasminogen activator-receptors in carcinomas of the female breast in an African population. East Afr Med J 78: 360–365
Morimoto K, Kim SJ, Tanei T, Shimazu K, Tanji Y, Taguchi T, Tamaki Y, Terada N, Noguchi S (2009) Stem cell marker aldehyde dehydrogenase 1-positive breast cancers are characterized by negative estrogen receptor, positive human epidermal growth factor receptor type 2, and high Ki67 expression. Cancer Sci 100: 1062–1068
Morris GJ, Naidu S, Topham AK, Guiles F, Xu Y, McCue P, Schwartz GF, Park PK, Rosenberg AL, Brill K, Mitchell EP (2007) Differences in breast carcinoma characteristics in newly diagnosed African-American and Caucasian patients: a single-institution compilation compared with the National Cancer Institute's Surveillance, Epidemiology, and End Results database. Cancer 110: 876–884
Nalwoga H, Arnes JB, Wabinga H, Akslen LA (2007) Frequency of the basal-like phenotype in African breast cancer. APMIS 115: 1391–1399
Nalwoga H, Arnes JB, Wabinga H, Akslen LA (2008) Expression of EGFR and c-kit is associated with the basal-like phenotype in breast carcinomas of African women. APMIS 116: 515–525
Nalwoga H, Odida M, Wabinga H (2006) c-erbB-2 oncoprotein over-expression in breast cancer and its relationship to histology type and grade in a Uganda population. East Afr Med J 83: 411–415
Nielsen TO, Hsu FD, Jensen K, Cheang M, Karaca G, Hu Z, Hernandez-Boussard T, Livasy C, Cowan D, Dressler L, Akslen LA, Ragaz J, Gown AM, Gilks CB, van de Rijn MV, Perou CM (2004) Immunohistochemical and clinical characterization of the basal-like subtype of invasive breast carcinoma. Clin Cancer Res 10: 5367–5374
Perou CM, Sorlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, Pollack JR, Ross DT, Johnsen H, Akslen LA, Fluge O, Pergamenschikov A, Williams C, Zhu SX, Lonning PE, Borresen-Dale AL, Brown PO, Botstein D (2000) Molecular portraits of human breast tumours. Nature 406: 747–752
Phillips TM, McBride WH, Pajonk F (2006) The response of CD24(−/low)/CD44+ breast cancer-initiating cells to radiation. J Natl Cancer Inst 98: 1777–1785
Population Council (2004) Uganda 2000–2001: results from the Demographic and Health Survey. Stud Fam Plann 35: 70–74
Porter PL, Lund MJ, Lin MG, Yuan X, Liff JM, Flagg EW, Coates RJ, Eley JW (2004) Racial differences in the expression of cell cycle-regulatory proteins in breast carcinoma. Cancer 100: 2533–2542
Rakha EA, Reis-Filho JS, Ellis IO (2008) Basal-like breast cancer: a critical review. J Clin Oncol 26: 2568–2581
Sihto H, Lundin J, Lehtimaki T, Sarlomo-Rikala M, Butzow R, Holli K, Sailas L, Kataja V, Lundin M, Turpeenniemi-Hujanen T, Isola J, Heikkila P, Joensuu H (2008) Molecular subtypes of breast cancers detected in mammography screening and outside of screening. Clin Cancer Res 14: 4103–4110
Silva J, Garcia V, Garcia JM, Pena C, Dominguez G, Diaz R, Lorenzo Y, Hurtado A, Sanchez A, Bonilla F (2007) Circulating Bmi-1 mRNA as a possible prognostic factor for advanced breast cancer patients. Breast Cancer Res 9: R55
Sladek NE, Kollander R, Sreerama L, Kiang DT (2002) Cellular levels of aldehyde dehydrogenases (ALDH1A1 and ALDH3A1) as predictors of therapeutic responses to cyclophosphamide-based chemotherapy of breast cancer: a retrospective study. Rational individualization of oxazaphosphorine-based cancer chemotherapeutic regimens. Cancer Chemother Pharmacol 49: 309–321
Sorlie T, Perou CM, Tibshirani R, Aas T, Geisler S, Johnsen H, Hastie T, Eisen MB, van de Rijn M, Jeffrey SS, Thorsen T, Quist H, Matese JC, Brown PO, Botstein D, Lonning PE, Borresen-Dale AL (2001) Gene expression patterns of breast carcinomas distinguish tumour subclasses with clinical implications. Proc Natl Acad Sci USA 98: 10869–10874
Sorlie T, Tibshirani R, Parker J, Hastie T, Marron JS, Nobel A, Deng S, Johnsen H, Pesich R, Geisler S, Demeter J, Perou CM, Lonning PE, Brown PO, Borresen-Dale AL, Botstein D (2003) Repeated observation of breast tumour subtypes in independent gene expression data sets. Proc Natl Acad Sci USA 100: 8418–8423
Sreerama L, Sladek NE (1997) Cellular levels of class 1 and class 3 aldehyde dehydrogenases and certain other drug-metabolizing enzymes in human breast malignancies. Clin Cancer Res 3: 1901–1914
Stefansson IM, Salvesen HB, Akslen LA (2006) Loss of p63 and cytokeratin 5/6 expression is associated with more aggressive tumours in endometrial carcinoma patients. Int J Cancer 118: 1227–1233
Tanei T, Morimoto K, Shimazu K, Kim SJ, Tanji Y, Taguchi T, Tamaki Y, Noguchi S (2009) Association of breast cancer stem cells identified by aldehyde dehydrogenase 1 expression with resistance to sequential Paclitaxel and epirubicin-based chemotherapy for breast cancers. Clin Cancer Res 15: 4234–4241
Tavassoli FA, Devilee P (2003) World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of the Breast and Female Genital Organs. IARC Press: Lyon
Tischkowitz M, Brunet JS, Begin LR, Huntsman DG, Cheang MC, Akslen LA, Nielsen TO, Foulkes WD (2007) Use of immunohistochemical markers can refine prognosis in triple negative breast cancer. BMC Cancer 7: 134
Wabinga HR, Parkin DM, Wabwire-Mangen F, Mugerwa JW (1993) Cancer in Kampala, Uganda, in 1989–91: changes in incidence in the era of AIDS. Int J Cancer 54: 26–36
Wojcik BE, Spinks MK, Optenberg SA (1998) Breast carcinoma survival analysis for African American and white women in an equal-access health care system. Cancer 82: 1310–1318
Yang XR, Sherman ME, Rimm DL, Lissowska J, Brinton LA, Peplonska B, Hewitt SM, Anderson WF, Szeszenia-Dabrowska N, Bardin-Mikolajczak A, Zatonski W, Cartun R, Mandich D, Rymkiewicz G, Ligaj M, Lukaszek S, Kordek R, Garcia-Closas M (2007) Differences in risk factors for breast cancer molecular subtypes in a population-based study. Cancer Epidemiol Biomarkers Prev 16: 439–443
Acknowledgements
We acknowledge the Norwegian government (NUFU) for funding this study. We also acknowledge the University of Bergen and Makerere University for establishing the collaboration through which the study was funded. We thank the Department of Pathology at the Makerere University College of Health Sciences for allowing us to use the archival tissue and the Kampala Cancer Registry for providing us with supporting data. We acknowledge Arie P Otte for providing the BMI-1 antibody. We also acknowledge the Centre for Disease Control and Prevention for computerising the database at the department. We appreciate the excellent technical support offered by Gerd Lillian Hallseth, Dorothy Lynn Nabbale, Ruth Nakigudde, Bendik Nordanger and Randi Nygaard. We also extend our thanks to all the staff of The Gade Institute for the support they offered during the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Nalwoga, H., Arnes, J., Wabinga, H. et al. Expression of aldehyde dehydrogenase 1 (ALDH1) is associated with basal-like markers and features of aggressive tumours in African breast cancer. Br J Cancer 102, 369–375 (2010). https://doi.org/10.1038/sj.bjc.6605488
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6605488
Keywords
This article is cited by
-
Radiomic signatures from T2W and DWI MRI are predictive of tumour hypoxia in colorectal liver metastases
Insights into Imaging (2023)
-
Ancestry-associated transcriptomic profiles of breast cancer in patients of African, Arab, and European ancestry
npj Breast Cancer (2021)
-
Multiethnic PDX models predict a possible immune signature associated with TNBC of African ancestry
Breast Cancer Research and Treatment (2021)
-
The prognostic significance of BMI1 expression in invasive breast cancer is dependent on its molecular subtypes
Breast Cancer Research and Treatment (2020)
-
DSPP-MMP20 gene silencing downregulates cancer stem cell markers in human oral cancer cells
Cellular & Molecular Biology Letters (2018)