Abstract
Background:
Malignant gliomas are the most prevalent type of primary brain tumours but the therapeutic armamentarium for these tumours is limited. Platelet-derived growth factor (PDGF) signalling has been shown to be a key regulator of glioma development. Clinical trials evaluating the efficacy of anti-PDGFRA therapies on gliomas are ongoing. In this study, we intended to analyse the expression of PDGFA and its receptor PDGFRA, as well as the underlying genetic (mutations and amplification) mechanisms driving their expression in a large series of human gliomas.
Methods:
PDGFA and PDGFRA expression was evaluated by immunohistochemistry in a series of 160 gliomas of distinct World Health Organization (WHO) malignancy grade. PDGFRA-activating gene mutations (exons 12, 18 and 23) were assessed in a subset of 86 cases by PCR—single-strand conformational polymorphism (PCR-SSCP), followed by direct sequencing. PDGFRA gene amplification analysis was performed in 57 cases by quantitative real-time PCR (QPCR) and further validated in a subset of cases by chromogenic in situ hybridisation (CISH) and microarray-based comparative genomic hybridisation (aCGH).
Results:
PDGFA and PDGFRA expression was found in 81.2% (130 out of 160) and 29.6% (48 out of 160) of gliomas, respectively. Its expression was significantly correlated with histological type of the tumours; however, no significant association between the expression of the ligand and its receptor was observed. The absence of PDGFA expression was significantly associated with the age of patients and with poor prognosis. Although PDGFRA gene-activating mutations were not found, PDGFRA gene amplification was observed in 21.1% (12 out of 57) of gliomas. No association was found between the presence of PDGFRA gene amplification and expression, excepting for grade II diffuse astrocytomas.
Conclusion:
The concurrent expression of PDGFA and PDGFRA in different subtypes of gliomas, reinforce the recognised significance of this signalling pathway in gliomas. PDGFRA gene amplification rather than gene mutation may be the underlying genetic mechanism driving PDGFRA overexpression in a portion of gliomas. Taken together, our results could provide in the future a molecular basis for PDGFRA-targeted therapies in gliomas.
Similar content being viewed by others
Main
Malignant gliomas are highly heterogeneous and invasive tumours and account for approximately 70% of all primary brain tumours (Louis et al, 2007). Histologically, gliomas are classified into several entities, with astrocytic tumours being the most prevalent type, followed by oligodendroglial and mixed oligoastrocytic tumours, and less frequently ependymomas (Louis et al, 2007). According to the World Health Organisation (WHO), tumours are classified into four grades of malignancy: grade I generally behave in a benign fashion, whereas grade II–IV are biologically malignant, diffusely infiltrating the adjacent brain tissues and ultimately progressing to glioblastoma (WHO grade IV) (Louis et al, 2007). Although relatively uncommon, malignant gliomas are associated with disproportionately high morbidity and mortality, with a median survival time of 12 to 15 months for glioblastomas and 24 to 60 months for patients with anaplastic gliomas (Lacroix et al, 2001). Despite advances in understanding glioma molecular pathogenesis and treatment improvements, little is known about the cause of this disease and strategies which may result in effective treatment (Louis, 2006; Wen and Kesari, 2008). Therefore, further investigation of the molecular basis of gliomagenesis is essential for the identification of new therapeutic targets for these tumours.
The platelet-derived growth factor receptor A (PDGFRA) is a transmembrane protein with five immunoglobulin-like repeats in the extracellular domain and with a split intracellular tyrosine kinase domain. PDGFRA belongs to class III family of receptor tyrosine kinases (RTKs) that also includes PDGFRB, KIT, the macrophage colony-stimulating-factor receptor and Fl cytokine receptor (Blume-Jensen and Hunter, 2001). Ligand-activated receptors trigger downstream signal transduction pathways, including MAP kinase, PI3-kinase/AKT and JAK/STAT and have pivotal roles in proliferation, differentiation, invasion and survival (Blume-Jensen and Hunter, 2001). PDGFRA and its main ligand PDGFA are key regulators of glial cells proliferation, mainly oligodendrocytes, and have an important role in normal development of the central nervous system (Richardson et al, 1988).
Platelet-derived growth factor (PDGF) has also been implicated in cancer, including central nervous system tumours (Shih and Holland, 2006). PDGF and PDGF receptors are commonly coexpressed in gliomas, suggesting that autocrine PDGF receptor stimulation may contribute to their growth (Hermanson et al, 1992; Westermark et al, 1995). Glioma-like tumours can be induced in mice after overproduction of PDGF in mouse brain (Uhrbom et al, 1998). Taken together, these findings provide strong circumstantial evidence to suggest that PDGFR signalling may be a driver of gliomagenesis. Given that PDGFRA is a transmembrane tyrosine kinase receptor and that these receptors have been shown to be amenable to exploitation as therapeutic targets, it seems reasonable to hypothesise that PDGFRA may constitute a potential target for anticancer therapy in gliomas.
The interest in PDGFR as a cancer drug target has increased with the availability of clinically useful small-molecule inhibitors, such as imatinib mesylate (Glivec) and sunitinib (Sutent) (Pietras et al, 2003). Imatinib is an orally available RTK inhibitor, which, in addition to PDGFRs, also inhibits KIT, c-Abl, Bcr–Abl and Arg (Capdeville et al, 2002). The clinical efficacy of imatinib is well demonstrated in chronic myeloid leukaemia and in gastrointestinal stromal tumours (GISTs), which are driven by activated forms of BCR–ABL and mutated KIT or PDGFRA genes, respectively (Druker et al, 2001; Demetri et al, 2002). In addition, clinical trials are ongoing using imatinib for the treatment of recurrent glioblastoma patients (Reardon et al, 2005; Raymond et al, 2008). However, the molecular alterations underlying PDGF overexpression and response to PDGFR antagonists in gliomas remain poorly understood. Thus, the aim of this study was to define the frequency of PDGFRA and PDGFA expression in a large series of gliomas and to determine whether expression of PDGFRA is driven by PDGFRA gene mutations and/ or amplification.
Materials and methods
Tissue samples
Representative formalin-fixed paraffin-embedded blocks from one hundred and sixty consecutive craniotomies for gliomas were retrieved from pathology archives of the Department of Pathology of Hospital S João, Porto and of Hospital S Marcos, Braga, Portugal. Cases were classified according to the WHO criteria (Louis et al, 2007). This series (Table 1) includes 83 astrocytic, 68 oligodendroglial and 9 oligoastrocytic tumours. The mean age of patients at diagnosis was 45.9±17.6 (range, 2–79 years), with a female/male ratio of 0.93. Follow-up data were available in 108 patients (range: 0–210 months, mean: 38.4±42.1 months). The procedures followed in the present study were in accordance with the institutional ethical committees. All the samples enrolled in this study were completely anonymised after retrieval of follow up information.
PDGFA and PDGFRA immunohistochemistry
Representative 3-μm thick sections were cut from formalin-fixed and paraffin-embedded samples and subjected to immunohistochemical analysis. Immunohistochemistry was carried out using a LabVision Autostainer (LabVision Corporation, Fremont, CA, USA) and the streptavidin—biotin–peroxidase complex technique, with rabbit polyclonal antibodies raised against human PDGFA (clone N-30, dilution 1:80; Santa Cruz Biotechnology, Santa Cruz, USA), and PDGFRA (dilution 1:175; LabVision Corporation) as previously described (Carvalho et al, 2005; Reis et al, 2005). In brief, deparaffinised and rehydrated sections used to study PDGFA expression were pre-treated by microwaving in 10 mM citrate buffer (pH 6.0) three times for 5 min at 600 W. The sections used for PDGFRA expression were submitted to heat-induced antigen retrieval with 10 mM citrate buffer (pH 6.0) for 20 min in a water bath. After incubation of PDGFA and PDGFRA primary antibody at room temperature for 30 min, the secondary biotinylated goat anti-polyvalent antibody was applied for 10 min followed by incubation with streptavidin–peroxidase complex. The immune reaction was visualised by DAB as a chromogen (Ultravision Detection System Anti-polyvalent, HRP/DAB; LabVision Corporation). Appropriated positive and negative controls were included in each run: for PDGFA and PDGFRA, cutaneous-mucosa transition of the anal region, namely medium calibre vessels with a muscular layer were used as positive controls. For negative controls, primary antibodies were omitted. All sections were counterstained with Gill-2 haematoxylin. As previously described (Reis et al, 2005), both the distribution and intense immunoreactivity were semi-quantitatively scored by JML and ALF independently with the observers blinded to the clinical information and results of the other molecular tests as follows: (−) (negative), (+) (⩽5%), (++) (5–50%), and (+++) (>50%). Samples with scores (−) and (+) were considered negative, and those with scores (++) and (+++) were considered positive.
DNA isolation
Serial 10 μm unstained section of paraffin blocks were cut, and one adjacent haematoxylin and eosin-stained (H&E) section was taken for identification and selection of the tumour tissue. Selected areas containing at least 85% of tumour were marked and macroscopically dissected using a sterile needle (Neolus, 25G–0.5 mm). Tissue was placed into a microfuge tube and DNA isolation was performed using QIAamp DNA Micro Kit (Qiagen, Hilden, Germany) as previously described (Basto et al, 2005).
PDGFRA mutations
Pre-screening for mutations in exons 12, 18 and 23 of the PDGFRA gene was carried out by PCR-single-strand conformational polymorphism (PCR–SSCP) followed by direct DNA sequencing of samples that showed a mobility shift in the PCR–SSCP analysis, as previously described (Reis et al, 2005). Briefly, PCR was carried out in a total volume of 25 μl, consisting of 1–2 μl of DNA solution, 0.5 μ M of both sense and anti-sense primers, 200 μ M of dNTPs (Fermentas Inc., Glen Burnie, MD, USA), 1.5–2 mM of MgCl2 (Bioron GmbH, Ludwigshafen, Germany), 1 × Taq Buffer Incomplete (Bioron GmbH) and 1U of Taq Superhot DNA Polymerase (Bioron GmbH). The reaction consisted of an initial denaturation at 96 °C for 10 min, followed by 40 cycles with denaturation at 96 °C for 45 s, annealing at 56–60 °C for 45 s and extension at 72 °C for 45 s, followed by a final extension for 10 min at 72 °C, in a Thermocycler (BioRad, Hercules, CA, USA). Primer sequences for exons 12 and 18 were previously reported (Reis et al, 2005), and for exon 23 were 5′-GCTCTTCTCTCCCTCCTCCA-3′ (sense) and 5′-TTTCTGAACGGGATCCAGAG-3′ (antisense). PCR products were mixed with an equivalent volume of the denaturing loading buffer (98% formamide, 0.05% xylene cyanol and bromophenol blue). After denaturation at 98 °C for 10 min and quenching on ice, 20 μl of the mixture were loaded onto a gel containing 0.8 × MDE (Cambrex Corporation, East Rutherford, NJ, USA) for exons 12 and 18 and 1 × MDE for exon 23, and 0–3% Glycerol (0% for exon 12 and 3% for exons 18 and 23). The gels were run for 20 h at 4 °C for exons 12 and 18 and 20 °C for exon 23. After the run, the gel was stained with Sybr Gold (Invitrogen Ltd., Paisley, UK) and visualised under ultraviolet light in a UV transilluminator.
Samples showing a mobility shift in the PCR–SSCP analysis different from the normal pattern were directly sequenced (Stab Vida, Investigation and Services in Biological Sciences Lda, Oeiras, Portugal) as previously described (Gomes et al, 2007). All positive cases were confirmed twice with a new and independent PCR amplification, followed by direct sequencing.
Analysis of PDGFRA gene copy number status
Quantitative real-time PCR
Quantitative real-time PCR (QPCR) was performed with LightCycler (Roche Molecular Biochemicals, Mannheim, Germany), using fluorescent hybridisation probes and fluorescence resonance energy transfer for the detection of PCR amplification product, following the manufacturer's instructions. Briefly, primers and probes were designed to amplify a 124 bp (exon 18 from PDGFRA gene), and a 147 bp (18S gene) specific PCR product, where 18S was used as reference gene. PCR amplification was performed in a 10 μl reaction volume, under the following conditions: 1 × reaction master mix (Lightcycler FastStart DNA Master Hybridisation Probes kit, Roche Molecular Biochemicals); 0.2 μ M Probes (Roche Molecular Biochemicals); 0.5 μ M primers; 4 mM MgCl2 (Roche Molecular Biochemicals) and 1 μl (20 ng μl−1) of DNA. The reaction was initiated by a denaturation step for 10 min at 95 °C, followed by 45 cycles with the following profile of amplification: incubation for 10 s at 94 °C, specific annealing temperature (57 °C for both genes) for 10 s and extension at 72 °C for an amplicon dependent time (7 s for 18S and 5 s for PDGFRA), immediately followed by a cooling step for 2 min at 40 °C. Primers and probes for 18S gene were previously described (Gomes et al, 2007), for PDGFRA were as follow: 5′-TCAGCTACAGATGGCTTGATCC-3′ (forward primer), 5′-GCCAAAGTCACAGATCTTCACAAT-3′ (reverse primer), 5′-TGTGTCCACCGTGATCTGGCTGC-FL (donator probe), LC640-CGCAACGTCCTCCTGGCACAAGG-3′ (acceptor probe). The PCR was performed in duplicate for each studied sample. A series of 10 normal DNA from healthy individuals was investigated to determine the confidence interval and the s.d. of the calculated ratios for reference and target gene. Evaluation of data was carried out using the ΔΔCt method: ΔΔCt=ΔCt Tumour DNA – ΔCt Normal blood DNA. ΔCt (threshold cycles) is the Ct of the reference gene minus the Ct of the target gene. Fold increase of the target gene PDGFRA was calculated by 2(ΔΔCt) and values >2 and <5 were defined as aneuploidy and values ⩾5 were considered as gene amplification.
Chromogenic in situ hybridisation
The presence of PDGFRA gene amplification was also assessed by means of chromogenic in situ hybridisation (CISH) with an in-house generated probe made up with three contiguous, FISH-mapped and end-sequence verified bacterial artificial chromosomes (BACs) (RP11-626H04, RP11-231C18 and RP11-545H22), which map to the PDGFRA locus on 4q12 according to Ensembl V39—June 2006 build of the genome (http://www.ensembl.org/Homo_sapiens/index.html). The in-house probe was generated, biotin-labelled and used in hybridisations as previously described (Lambros et al, 2006; Gomes et al, 2007). Briefly, heat pre-treatment of deparaffinised sections were incubated for 15 min at 98 °C in CISH pre-treatment buffer (SPOT-light tissue pre-treatment kit, Zymed Laboratories, San Francisco, CA, USA) and digested with pepsin for 6 min at room temperature according to the manufacturer's instructions. CISH experiments were analysed by three of the authors on a multi-headed microscope. Only unequivocal signals were counted. Signals were evaluated at × 400 and × 630 and 60 morphologically unequivocal neoplastic cells were counted for the presence of the gene probe signals. Amplification was defined as >5 signals per nucleus in more than 50% of tumour cells, or when large gene copy clusters were seen (Lambros et al, 2006; Gomes et al, 2007). CISH hybridisations were evaluated with observers blinded to the clinical information and results of immunohistochemical and QPCR analysis.
Microarray-based comparative genomic hybridisation
The aCGH platform used for this study was constructed at the Breakthrough Breast Cancer Research Centre and comprises >16 000 BAC clones tiled across the genome (Arriola et al, 2007). This type of BAC array platform has been shown to be as robust as high-density oligonucleotide arrays (Coe et al, 2007; Gunnarsson et al, 2008) and its actual resolution is approximately 100 kb for >98% of the genome (Arriola et al, 2007, 2008; Marchiò et al, 2008a). Labelling, hybridisation, washes, image acquisition and data normalisation were carried out as previously described (Arriola et al, 2007, 2008; Huang et al, 2007; Marchiò et al, 2008a, 2008b). Polymorphic BACs identified in an analysis of 50 male/female and female/female hybridisations were filtered out. This left a final dataset of 13711 clones with unambiguous mapping information according to the March 2006 build (hg18) of the human genome (http://www.ensembl.org). Data were smoothed using the adaptive weight smoothing (aws) algorithm (Mackay et al, 2009). A categorical analysis was applied to the BACs after classifying them as representing gain, loss, or no-change according to their smoothed Log2 ratio values Threshold values were chosen to correspond to three s.d. of the normal ratios obtained from the filtered clones mapping to chromosomes 1–22, assessed in multiple hybridisations between DNA extracted from a pool of male and female blood donors as previously described (Arriola et al, 2008; Reis-Filho et al, 2008) (Log2 ratio of ±0.08). Low level gain was defined as a smoothed Log2 ratio of between 0.12 and 0.40, corresponding to approximately 3–5 copies of the locus, whereas gene amplification was defined as having a Log2 ratio >0.40, corresponding to more than 5 copies (Arriola et al, 2008). These figures were obtained by comparison with interphase FISH data for markers at different chromosomal locations (Reis-Filho et al, 2008). Data processing and analysis were carried out in R 2.0.1 (http://www.r-project.org/) and BioConductor 1.5 (http://www.bioconductor.org/), making extensive use of modified versions of the packages aCGH, marray and aws in particular.
Statistical analysis
Correlations between categorical variables were performed using the χ2-test. Cumulative survival probabilities were calculated using the Kaplan–Meier method. Differences between survival rates were tested with the log-rank test. Two-tailed P-values <0.05 were considered significant. All statistical analysis was performed using SPSS software for Windows, version 14.0.
Results
PDGFA and PDGFRA expression
PDGFA and PDGFRA expression was found in 81.2% (130 out of 160) and 29.6% (48 out of 160) of gliomas, respectively. Immunohistochemical analysis showed that tumour cells express PDGFA in the cytoplasm (Figure 1A), whereas PDGFRA was preferentially observed in the cytoplasmic compartment and rarely on membranes (Figure 1B). PDGFA expression was also observed in tumour-associated endothelial cells and in basal membrane of blood vessels in approximately 12% (19 out of 160) of the cases (Figure 1C). Representative PDGFRA-negative staining is shown in Figure 1D. Twenty five percent (40 out of 160) of gliomas coexpressed PDGFA and their receptor PDGFRA; however, no statistically significant association between the expression of the ligand and its receptor was observed (P>0.05). When the presence or absence of PDGFA/PDGFRA overexpression (+++) was defined according to histological type, a trend for PDGFA and PDGFRA coexpression in glioblastomas was found (P=0.069).
Immunohistochemistry analysis of PDGFA and PDGFRA in gliomas; (A) Glioblastoma with (+++) score for PDGFA expression ( × 200); (B) Glioblastoma with (+++) score for PDGFRA expression ( × 200). (C) Glioblastoma with (−) score for PDGFA expression in tumour cells and positive in endothelial cells ( × 200). (D) Glioblastoma with (+) score for PDGFRA expression ( × 200).
PDGFA and PDGFRA expression was significantly correlated with histological type (P=0.004 and 0.0001, respectively) (Table 1). When tumours were classified into the three major groups according to their histogenesis (astrocytic, oligodendroglial and mixed), only PDGFRA expression was statistically significantly correlated with astrocytic lineage (P<0.001) (Table 1).
In 22 cases, it was possible to analyse PDGFA and PDGFRA expression in both primary and recurrent tumours (Table 2). Overall, the results were concordant; however, we observed loss or gain of PDGFA and PDGFRA in recurrent tumours of some patients (Table 2).
No statistically significant correlations were found between PDGFRA expression and clinical–pathological parameters including age, gender, WHO histological grade and prognosis (Table 1). However, the absence of PDGFA expression was significantly associated (P=0.023) with age (>45 years) and with a poor prognosis in glioma patients (P=0.026) (Table 1 and Figure 2).
PDGFRA gene mutations
PCR–SSCP analysis for PDGFRA gene mutations in exons 12, 18 and 23 produced optimal results in 86 cases, 30 of which were PDGFRA-positive tumours. No activating mutations were found. However, four silent mutations and an intronic insertion were identified in 45.3% (39 out of 86) of glioma patients (Table 3). Five patients showed the simultaneous presence of two different mutations. No association was found between the presence of PDGFRA gene mutations and PDGFRA expression (P>0.05).
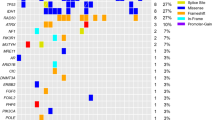
PDGFRA gene amplification
Analysis of PDGFRA gene copy number status as defined by QPCR was successfully performed in 57 gliomas. PDGFRA copy number changes (ratio >2) were observed in 52.6% (30 out of 57) of glioma patients: 18 displayed ratios <5 and were considered representative of aneuploidy/aneusomy and 12 (21.1%) harboured ratios ⩾5 and were considered amplified (Table 1). No statistically significant associations were found between the PDGFRA amplification and PDGFRA expression. However, a borderline association (P=0.058) was observed between amplification and overexpression (+++). In addition, a statistically significant association (P=0.038) was found between PDGFRA amplification and overexpression in grade II diffuse astrocytomas (Table 4). After statistical analysis, no significant correlations were found between the PDGFRA gene amplification and clinical–pathological features (P>0.05) (Table 1).
In 12 cases, data on PDGFRA amplification status in both the primary and recurrent tumours were available (Table 2). In all but one case (tumours 110 and 111) primary and recurrent tumours displayed identical PDGFRA copy number status. Interestingly acquisition of PDGFRA amplification was observed in the recurrent tumour 111; however, this was not associated with expression of PDGFRA.
To validate QPCR results we performed CISH in six cases, three with and three without PDGFRA amplification as defined by QPCR. CISH analysis of cases defined as harbouring PDGFRA gene amplification by QPCR revealed clusters of PDGFRA signals in the nuclei of neoplastic cells (Figure 3A), confirming gene amplification. In normal cases, only one-to-two PDGFRA gene signals per nucleus were found in neoplastic cells (Figure 3B). To further validate the results of the QPCR analysis, we performed microarray-based comparative genomic hybridisation in two cases, one with and one without PDGFRA amplification as defined by QPCR. The case without PDGFRA gene amplification by QPCR showed no changes on chromosome 4 (Figure 4A). In the case with amplification, the peak of the amplicon on 4q was restricted to 4q12, encompassing a genomic region of 3.7 Mb (Figure 4B), flanked by the BACs RP11-654K2 (54025,329 kb) and RP11-284L3 (57933,681 kb), including the genes: LNX1, CHIC2, GSH2, PDGFRA, KIT, KDR, SRD5A2 L, TMEM165, CLOCK, PDCL2, NMU, EXOC1, CEP135, AASDH, PPAT, PAICS, SRP72, ARL9, HOP, SPINK2, REST, C4orf14, POLR2B, and IGFBP7. Taken together, the above CISH and aCGH findings provide a robust validation for the results obtained with QPCR.
Ideogram and microarray CGH chromosome plots of chromosome 4, in which PDGFRA gene is located, for a case without (A) and other with (B) PDGFRA amplification as defined by QPCR. Log2 ratios are plotted on the x axis against each clone according to genomic location on the y axis. The centromere is represented by a horizontal dotted line. Vertical dashed lines correspond to log2 ratios of 0.12 (green) and −0.12 (red). Grey dots: Log2 ratios; Blue dots: aws-smoothed Log2 ratios. The colour reproduction of this figure is available on the html full text version of the article.
Discussion
The PDGF pathway is one of the most consistently altered cellular signalling system in glial tumourigenesis (Shih and Holland, 2006; Fomchenko and Holland, 2007). PDGF and PDGFRs have both been found to be overexpressed in glial tumour cell lines and tumour surgical samples (Nister et al, 1988, 1991; Hermanson et al, 1992; Black et al, 1996; Di Rocco et al, 1998; Varela et al, 2004). PDGFRA and PDGFA have been shown to be expressed in tumour cells, whereas PDGFB and PDGFRB have been found in glioma-associated endothelial cells (Hermansson et al, 1988; Hermanson et al, 1992; Plate et al, 1992). Furthermore, studies on the PDGFC and D ligands, also demonstrate their expression in gliomas; however, the clinical and biological significance of their expression remain to be determined (Lokker et al, 2002). Importantly, the function of PDGF signalling in gliomagenesis has been enlightened by its potential role in cancer stem cell hypothesis of gliomagenesis. It has been suggested that activation of PDGFRA signalling, directly or indirectly through creating a favourable microenvironment niche, can contribute to the transformation of neural stem/progenitor cells into glioma tumours (Jackson et al, 2006; Fomchenko and Holland, 2007; Siebzehnrubl et al, 2008).
Clinical trials evaluating the efficacy of anti-PDGFRA drugs in patients with glioblastomas are ongoing (Reardon et al, 2005; Wen et al, 2006; Desjardins et al, 2007; Newton, 2007; Raymond et al, 2008). Despite the positive response, none of the new targeted therapies has shown significant clinical activity as a single agent in phase II studies (Brandsma and van den Bent, 2007; Raymond et al, 2008). Currently, combination of anti-PDGFRA drugs with chemotherapy agents is being evaluated (Reardon et al, 2008). However, the molecular alterations underlying glioma patients’ response to PDGFRA antagonists are unknown. One study analysed the prevalence of PDGFRA mutations in patients enrolled in a phase I/II study of imatinib mesylate in recurrent malignant gliomas; however, no activating mutations were observed (Wen et al, 2006). The in vitro studies using PDGFR-targeted drugs (e.g., imatinib) have provided conflicting information about the molecular underpinning of sensitivity to those agents. Although some suggested that sensitivity to targeted agents is associated with overall PDGFR activation; others point to the putative role of PDGFRB or failed to show any association between PDGFR status and response to imatinib (Gross et al, 2006; Hägerstrand et al, 2006; Servidei et al, 2006).
Here, we observed PDGFA expression in 81.2% of gliomas. Overall, PDGFA was highly expressed in all histological types of gliomas. Previous studies on PDGFA mRNA expression reported high levels of PDGFA in gliomas (Maxwell et al, 1990; Mapstone, 1991; Hermanson et al, 1992; Di Rocco et al, 1998). It should be noted, however, that there is a paucity of data on prevalence of PDGFA protein expression in primary glioma specimens. We have previously shown that 100% of gliosarcomas express PDGFA (Reis et al, 2005). PDGFRA expression was detected in 29.6% of gliomas, and more frequently expressed in 45–60% of malignant astrocytic tumours. These frequencies are in agreement with previous studies, where approximately 50% for malignant astrocytomas were reported to express this receptor (Nister et al, 1988, 1991; Hermanson et al, 1992; Black et al, 1996; Di Rocco et al, 1998; Ribom et al, 2002; Varela et al, 2004; Liang et al, 2008; Takei et al, 2008; Thorarinsdottir et al, 2008). A previous study showed PDGFRA expression in approximately 50% of gliomas and a correlation with poor prognosis in low-grade gliomas (Varela et al, 2004). However, in a report of 40 patients with grade II astrocytomas and oligoastrocytomas, there was an association between high PDGFRA expression and a favourable patient outcome (Ribom et al, 2002). Recently, Liang et al, (2008) in a paediatric high-grade glioma series failed to find any significant impact of PDGFRA expression on survival. In our series, PDGFRA expression was not correlated with patients’ survival. Interestingly, we found that the absence of PDGFA expression is significantly associated with age and poor prognosis in patients with glioma. Given the retrospective nature of our study, further analysis of the prognostic impact of PDGFA and PDGFRA expression in gliomas is warranted.
Overexpression of RTKs in cancer has been shown to be driven by underlying genetic events in a substantial proportion of cases (Gschwind et al, 2004). For instance, KIT overexpression in GISTs is driven by activating KIT mutations (Gomes et al, 2008), whereas HER2 overexpression in breast cancer is driven by HER2 gene amplification (Arriola et al, 2008). Here, we investigated the prevalence of PDGFRA-activating mutations and gene amplification in gliomas. In agreement with previous studies (Hartmann et al, 2004; Rand et al, 2005; Reis et al, 2005; Sihto et al, 2005; Wen et al, 2006; McLendon et al, 2008; Parsons et al, 2008), no PDGFRA-activating mutations were found. However, four silent mutations and an intronic insertion were identified. Apart from two silent mutations in PDGFRA exon 12, the other mutations have been previously described and considered to be genetic polymorphisms (http://www.ncbi.nlm.nih.gov/projects/SNP/; Carvalho et al, 2005; Reis et al, 2005; Wen et al, 2006). The impact of these genetic polymorphisms in PDGFRA function remains to be elucidated.
PDGFRA gene amplification analysis revealed PDGFRA amplification in 21.1% (12 out of 57) of gliomas, a frequency similar to that described in previous studies (Fleming et al, 1992; Kumabe et al, 1992; Smith et al, 2000; Alonso et al, 2005; Arjona et al, 2005; Puputti et al, 2006; Beroukhim et al, 2007; McLendon et al, 2008). We have further shown by aCGH that the amplicon encompasses a region of 3.6 Mb, which, in addition to PDGFRA, also includes KIT and KDR oncogenes. Co-amplification of these three oncogenes has already been detected with other methodologies in gliomas (Joensuu et al, 2005; Puputti et al, 2006; Holtkamp et al, 2007). A statistically significant association between PDGFRA amplification and overexpression was found only in diffuse astrocytomas (grade II). Given that PDGFRA overexpression appears to be an early event in gliomagenesis (Hermanson et al, 1996), our results provide support to the contention that gene amplification may be one of the underlying mechanisms at this stage. In a way akin to other oncogenes, such as EGFR, overexpression of PDGFRA was more pervasive than gene amplification. It should be noted, however, that there were ∼42% of cases with PDGFRA amplification that lacked PDGFRA protein expression, suggesting that in some cases the target of 4q12 amplification may be a gene other than PDGFRA.
In conclusion, here we show that PDGFA is expressed in different types of gliomas and its absence is associated with a poor prognosis. PDGFRA is significantly highly expressed in malignant astrocytic tumours. Based on the concurrent expression of PDGFA and PDGFRA in glioblastomas, it could be hypothesised that autocrine/paracrine loops may be present in these tumours, corroborating the importance of this signalling pathway in gliomas (Nister et al, 1991; Guha et al, 1995; Fomchenko and Holland, 2007). PDGFRA gene amplification may be the underlying genetic mechanism driving PDGFRA overexpression in gliomas. However, ∼42% of cases with amplification of PDGFRA did not display PDGFRA protein expression, suggesting that a gene other than PDGFRA may be the driver of this amplicon. Further studies are needed to correlate these molecular alterations and response to anti-PDGFRA drugs and to investigate the alternative drivers of the 4q12 amplicon. However, our results provide a step forward in the identification of a molecular basis for tailoring the therapies for specific subgroups of glioma patients.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Alonso ME, Bello MJ, Arjona D, Martinez-Glez V, de Campos JM, Isla A, Kusak E, Vaquero J, Gutierrez M, Sarasa JL, Rey JA (2005) Real-time quantitative PCR analysis of gene dosages reveals gene amplification in low-grade oligodendrogliomas. Am J Clin Pathol 123: 900–906
Arjona D, Bello MJ, Alonso ME, Isla A, de Campos JM, Vaquero J, Sarasa JL, Gutierrez M, Rey JA (2005) Real-time quantitative PCR analysis of regions involved in gene amplification reveals gene overdose in low-grade astrocytic gliomas. Diagn Mol Pathol 14: 224–229
Arriola E, Lambros MBK, Jones C, Dexter T, Mackay A, Tan DSP, Tamber N, Fenwick K, Ashworth A, Dowsett M, Reis JS (2007) Evaluation of Phi29-based whole-genome amplification for microarray-based comparative genomic hybridisation. Lab Invest 87: 75–83
Arriola E, Marchiò C, Tan DS, Drury SC, Lambros MB, Natrajan R, Rodriguez-Pinilla SM, Mackay A, Tamber N, Fenwick K, Jones C, Dowsett M, Ashworth A, Reis-Filho JS (2008) Genomic analysis of the HER2/TOP2A amplicon in breast cancer and breast cancer cell lines. Lab Invest 88: 491–503
Basto D, Trovisco V, Lopes JM, Martins A, Pardal F, Soares P, Reis RM (2005) Mutation analysis of B-RAF gene in human gliomas. Acta Neuropathol (Berlin) 109: 207–210
Beroukhim R, Getz G, Nghiemphu L, Barretina J, Hsueh T, Linhart D, Vivanco I, Lee JC, Huang JH, Alexander S, Du J, Kau T, Thomas RK, Shah K, Soto H, Perner S, Prensner J, DeBiasi RM, Demichelis F, Hatton C, Rubin MA, Garraway LA, Nelson SF, Liau L, Mischel PS, Cloughesy TF, Meyerson M, Golub TA, Lander ES, Mellinghoff IK, Sellers WR (2007) Assessing the significance of chromosomal aberrations in cancer: methodology and application to glioma. Proc Natl Acad Sci USA 104: 20007–20012
Black P, Carroll R, Glowacka D (1996) Expression of platelet-derived growth factor transcripts in medulloblastomas and ependymomas. Pediatr Neurosurg 24 (2): 74–78
Blume-Jensen P, Hunter T (2001) Oncogenic kinase signalling. Nature 411: 355–365
Brandsma D, van den Bent MJ (2007) Molecular targeted therapies and chemotherapy in malignant gliomas. Curr Opin Oncol 19: 598–605
Capdeville R, Buchdunger E, Zimmermann J, Matter A (2002) Glivec (STI571, imatinib), a rationally developed, targeted anticancer drug. Nat Rev Drug Discov 1: 493–502
Carvalho I, Milanezi F, Martins A, Reis RM, Schmitt F (2005) Overexpression of platelet-derived growth factor receptor alpha in breast cancer is associated with tumour progression. Breast Cancer Res 7: R788–R795
Coe BP, Ylstra B, Carvalho B, Meijer GA, Macaulay C, Lam WL (2007) Resolving the resolution of array CGH. Genomics 89: 647–653
Demetri GD, von Mehren M, Blanke CD, Van den Abbeele AD, Eisenberg B, Roberts PJ, Heinrich MC, Tuveson DA, Singer S, Janicek M, Fletcher JA, Silverman SG, Silberman SL, Capdeville R, Kiese B, Peng B, Dimitrijevic S, Druker BJ, Corless C, Fletcher CD, Joensuu H (2002) Efficacy and safety of imatinib mesylate in advanced gastrointestinal stromal tumors. N Engl J Med 347: 472–480
Desjardins A, Quinn JA, Vredenburgh JJ, Sathornsumetee S, Friedman AH, Herndon JE, McLendon RE, Provenzale JM, Rich JN, Sampson JH, Gururangan S, Dowell JM, Salvado A, Friedman HS, Reardon DA (2007) Phase II study of imatinib mesylate and hydroxyurea for recurrent grade III malignant gliomas. J Neuro Oncol 83: 53–60
Di Rocco F, Carroll RS, Zhang J, Black PM (1998) Platelet-derived growth factor and its receptor expression in human oligodendrogliomas. Neurosurgery 42: 341–346
Druker BJ, Sawyers CL, Kantarjian H, Resta DJ, Reese SF, Ford JM, Capdeville R, Talpaz M (2001) Activity of a specific inhibitor of the BCR-ABL tyrosine kinase in the blast crisis of chronic myeloid leukemia and acute lymphoblastic leukemia with the Philadelphia chromosome. N Engl J Med 344: 1038–1042
Fleming TP, Saxena A, Clark WC, Robertson JT, Oldfield EH, Aaronson SA, Ali IU (1992) Amplification and/or overexpression of platelet-derived growth factor receptors and epidermal growth factor receptor in human glial tumors. Cancer Res 52: 4550–4553
Fomchenko EI, Holland EC (2007) Platelet-derived growth factor-mediated gliomagenesis and brain tumor recruitment. Neurosurg Clin N Am 18: 39–58
Gomes AL, Gouveia A, Capelinha AF, de la CD, Silva P, Reis RM, Pimenta A, Lopes JM (2008) Molecular alterations of KIT and PDGFRA in GISTs: evaluation of a Portuguese series. J Clin Pathol 61: 203–208
Gomes AL, Reis-Filho JS, Lopes JM, Martinho O, Lambros MB, Martins A, Schmitt F, Pardal F, Reis RM (2007) Molecular alterations of KIT oncogene in gliomas. Cell Oncol 29: 399–408
Gross D, Bernhardt G, Buschauer A (2006) Platelet-derived growth factor receptor independent proliferation of human glioblastoma cells: selective tyrosine kinase inhibitors lack antiproliferative activity. J Cancer Res Clin Oncol 132: 589–599
Gschwind A, Fischer OM, Ullrich A (2004) Timeline—The discovery of receptor tyrosine kinases: targets for cancer therapy. Nat Rev Cancer 4: 361–370
Guha A, Dashner K, Black PM, Wagner JA, Stiles CD (1995) Expression of PDGF and PDGF receptors in human astrocytoma operation specimens supports the existence of an autocrine loop. Int J Cancer 60: 168–173
Gunnarsson R, Staaf J, Jansson M, Ottesen AM, Goransson H, Liljedahl U, Ralfkiaer U, Mansouri M, Buhl AM, Smedby KE, Hjalgrim H, Syvanen AC, Borg A, Isaksson A, Jurlander J, Juliusson G, Rosenquist R (2008) Screening for copy-number alterations and loss of heterozygosity in chronic lymphocytic leukemia--a comparative study of four differently designed, high resolution microarray platforms. Genes Chromosomes Cancer 47: 697–711
Hägerstrand D, Hesselager G, Achterberg S, Wickenberg Bolin U, Kowanetz M, Kastemar M, Heldin CH, Isaksson A, Nistér M, Ostman A (2006) Characterization of an imatinib-sensitive subset of high-grade human glioma cultures. Oncogene 25: 4913–4922
Hartmann C, Xu X, Bartels G, Holtkamp N, Gonzales IA, Tallen G, von Deimling A (2004) Pdgfr-alpha in 1p/19q LOH oligodendrogliomas. Int J Cancer 112: 1081–1082
Hermanson M, Funa K, Hartman M, Claesson Welsh L, Heldin CH, Westermark B, Nister M (1992) Platelet-derived growth factor and its receptors in human glioma tissue: expression of messenger RNA and protein suggests the presence of autocrine and paracrine loops. Cancer Res 52: 3213–3219
Hermanson M, Funa K, Koopmann J, Maintz D, Waha A, Westermark B, Heldin CH, Wiestler OD, Louis DN, von Deimling A, Nister M (1996) Association of loss of heterozygosity on chromosome 17p with high platelet-derived growth factor alpha receptor expression in human malignant gliomas. Cancer Res 56: 164–171
Hermansson M, Nister M, Betsholtz C, Heldin CH, Westermark B, Funa K (1988) Endothelial cell hyperplasia in human glioblastoma: coexpression of mRNA for platelet-derived growth factor (PDGF) B chain and PDGF receptor suggests autocrine growth stimulation. Proc Natl Acad Sci USA 85: 7748–7752
Holtkamp N, Ziegenhagen N, Malzer E, Hartmann C, Giese A, von Deimling A (2007) Characterization of the amplicon on chromosomal segment 4q12 in glioblastoma multiforme. Neuro Oncol 9: 291–297
Huang J, Gusnanto A, O′Sullivan K, Staaf J, Borg A, Pawitan Y (2007) Robust smooth segmentation approach for array CGH data analysis. Bioinformatics 23: 2463–2469
Jackson EL, Garcia-Verdugo JM, Gil-Perotin S, Roy M, Quinones-Hinojosa A, VandenBerg S, Alvarez-Buylla A (2006) PDGFR alpha-positive B cells are neural stem cells in the adult SVZ that form glioma-like growths in response to increased PDGF signaling. Neuron 51: 187–199
Joensuu H, Puputti M, Sihto H, Tynninen O, Nupponen NN (2005) Amplification of genes encoding KIT, PDGFRalpha and VEGFR2 receptor tyrosine kinases is frequent in glioblastoma multiforme. J Pathol 207: 224–231
Kumabe T, Sohma Y, Kayama T, Yoshimoto T, Yamamoto T (1992) Amplification of alpha-platelet-derived growth factor receptor gene lacking an exon coding for a portion of the extracellular region in a primary brain tumor of glial origin. Oncogene 7: 627–633
Lacroix M, Abi-Said D, Fourney DR, Gokaslan ZL, Shi W, DeMonte F, Lang FF, McCutcheon IE, Hassenbusch SJ, Holland E, Hess K, Michael C, Miller D, Sawaya R (2001) A multivariate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival. J Neurosurg 95: 190–198
Lambros MB, Simpson PT, Jones C, Natrajan R, Westbury C, Steele D, Savage K, Mackay A, Schmitt FC, Ashworth A, Reis-Filho JS (2006) Unlocking pathology archives for molecular genetic studies: a reliable method to generate probes for chromogenic and fluorescent in situ hybridization. Lab Invest 86: 398–408
Liang ML, Ma J, Ho M, Solomon L, Bouffet E, Rutka JT, Hawkins C (2008) Tyrosine kinase expression in pediatric high grade astrocytoma. J Neuro Oncol 87: 247–253
Lokker NA, Sullivan CM, Hollenbach SJ, Israel MA, Giese NA (2002) Platelet-derived growth factor (PDGF) autocrine signaling regulates survival and mitogenic pathways in glioblastoma cells: evidence that the novel PDGF-C and PDGF-D ligands may play a role in the development of brain tumors. Cancer Res 62: 3729–3735
Louis DN (2006) Molecular pathology of malignant gliomas. Annu Rev Pathol 1: 97–117
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, Scheithauer BW, Kleihues P (2007) The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathologica 114: 97–109
Mapstone TB (1991) Expression of platelet-derived growth factor and transforming growth factor and their correlation with cellular morphology in glial tumors. J Neurosurg 75: 447–451
Marchiò C, Iravani M, Natrajan R, Lambros MB, Savage K, Tamber N, Fenwick K, Mackay A, Senetta R, Di PS, Schmitt FC, Bussolati G, Ellis LO, Ashworth A, Sapino A, Reis-Filho JS (2008a) Genomic and immunophenotypical characterization of pure micropapillary carcinomas of the breast. J Pathol 215: 398–410
Marchiò C, Natrajan R, Shiu KK, Lambros MB, Rodriguez-Pinilla SM, Tan DS, Lord CJ, Hungermann D, Fenwick K, Tamber N, Mackay A, Palacios J, Sapino A, Buerger H, Ashworth A, Reis-Filho JS (2008b) The genomic profile of HER2-amplified breast cancers: the influence of ER status. J Pathol 216: 399–407
Mackay A, Tamber N, Fenwick K, Iravani M, Grigoriadis A, Dexter T, Lord CJ, Reis-Filho JS, Ashworth A (2009) A high-resolution integrated analysis of genetic and expression profiles of breast cancer cell lines. Breast Cancer Res Treat (e-pub ahead of print 24 January 2009)
Maxwell M, Naber SP, Wolfe HJ, Galanopoulos T, Hedley-Whyte ET, Black PM, Antoniades HN (1990) Coexpression of platelet-derived growth factor (PDGF) and PDGF-receptor genes by primary human astrocytomas may contribute to their development and maintenance. J Clin Invest 86: 131–140
Newton HB (2007) Small-molecule and antibody approaches to molecular chemotherapy of primary brain tumors. Curr Opin Invest Drugs 8: 1009–1021
Newton HB (2007) Small-molecule and antibody approaches to molecular chemotherapy of primary brain tumors. Curr Opin Invest Drugs 8: 1009–1021
Nister M, Claesson-Welsh L, Eriksson A, Heldin CH, Westermark B (1991) Differential expression of platelet-derived growth factor receptors in human malignant glioma cell lines. J Biol Chem 266: 16755–16763
Nister M, Libermann TA, Betsholtz C, Pettersson M, Claesson Welsh L, Heldin CH, Schlessinger J, Westermark B (1988) Expression of messenger RNAs for platelet-derived growth factor and transforming growth factor-alpha and their receptors in human malignant glioma cell lines. Cancer Res 48: 3910–3918
Parsons DW, Jones S, Zhang X, Lin JC, Leary RJ, Angenendt P, Mankoo P, Carter H, Siu IM, Gallia GL, Olivi A, McLendon R, Rasheed BA, Keir S, Nikolskaya T, Nikolsky Y, Busam DA, Tekleab H, Diaz Jr LA, Hartigan J, Smith DR, Strausberg RL, Marie SK, Shinjo SM, Yan H, Riggins GJ, Bigner DD, Karchin R, Papadopoulos N, Parmigiani G, Vogelstein B, Velculescu VE, Kinzler KW (2008) An integrated genomic analysis of human glioblastoma multiforme. Science 321 (5897): 1807–1812
Pietras K, Sjoblom T, Rubin K, Heldin CH, Ostman A (2003) PDGF receptors as cancer drug targets. Cancer Cell 3: 439–443
Plate KH, Breier G, Farrell CL, Risau W (1992) Platelet-derived growth factor receptor-beta is induced during tumor development and upregulated during tumor progression in endothelial cells in human gliomas. Lab Invest 67: 529–534
Puputti M, Tynninen O, Sihto H, Blom T, Maenpaa H, Isola J, Paetau A, Joensuu H, Nupponen NN (2006) Amplification of KIT, PDGFRA, VEGFR2, and EGFR in gliomas. Mol Cancer Res 4: 927–934
Rand V, Huang J, Stockwell T, Ferriera S, Buzko O, Levy S, Busam D, Li K, Edwards JB, Eberhart C, Murphy KM, Tsiamouri A, Beeson K, Simpson AJ, Venter JC, Riggins GJ, Strausberg RL (2005) Sequence survey of receptor tyrosine kinases reveals mutations in glioblastomas. Proc Natl Acad Sci USA 102: 14344–14349
Raymond E, Brandes AA, Dittrich C, Fumoleau P, Coudert B, Clement PM, Frenay M, Rampling R, Stupp R, Kros JM, Heinrich MC, Gorlia T, Lacombe D, van den Bent MJ, European Organisation for Research and Treatment of Cancer Brain Tumor Group Study (2008) Phase II study of imatinib in patients with recurrent gliomas of various histologies: a European Organisation for Research and Treatment of Cancer Brain Tumor Group Study. J Clin Oncol 26: 4659–4665
Reardon DA, Desjardins A, Vredenburgh JJ, Sathornsumetee S, Rich JN, Quinn JA, Lagattuta TF, Egorin MJ, Gururangan S, McLendon R, Herndon JE, Friedman AH, Salvado AJ, Friedman HS (2008) Safety and pharmacokinetics of dose-intensive imatinib mesylate plus temozolomide: Phase 1 trial in adults with malignant glioma. Neuro Oncol 10: 330–340
Reardon DA, Egorin MJ, Quinn JA, Rich JN, Gururangan S, Vredenburgh JJ, Desjardins A, Sathornsumetee S, Provenzale JM, Herndon JE, Dowell JM, Badruddoja MA, McLendon RE, Lagattuta TF, Kicielinski KP, Dresemann G, Sampson JH, Friedman AH, Salvado AJ, Friedman HS (2005) Phase II study of imatinib mesylate plus hydroxyurea in adults with recurrent glioblastoma multiforme. J Clin Oncol 23: 9359–9368
Reis-Filho JS, Drury S, Lambros MB, Marchio C, Johnson N, Natrajan R, Salter J, Levey P, Fletcher O, Peto J, Ashworth A, Dowsett M (2008) ESR1 gene amplification in breast cancer: a common phenomenon? Nat Genet 40: 809–810
Reis RM, Martins A, Ribeiro SA, Basto D, Longatto-Filho A, Schmitt FC, Lopes JM (2005) Molecular characterization of PDGFR-alpha/PDGF-A and c-KIT/SCF in gliosarcomas. Cell Oncol 27: 319–326
Ribom D, Andrae J, Frielingsdorf M, Hartman M, Nister M, Smits A (2002) Prognostic value of platelet derived growth factor alpha receptor expression in grade 2 astrocytomas and oligoastrocytomas. J Neurol Neurosurg Psychiatry 72: 782–787
Richardson WD, Pringle N, Mosley MJ, Westermark B, Dubois Dalcq M (1988) A role for platelet-derived growth factor in normal gliogenesis in the central nervous system. Cell 53: 309–319
Servidei T, Riccardi A, Sanguinetti M, Dominici C, Riccardi R (2006) Increased sensitivity to the platelet-derived growth factor (PDGF) receptor inhibitor STI571 in chemoresistant glioma cells is associated with enhanced PDGF-BB-mediated signaling and STI571-induced Akt inactivation. J Cell Physiol 208: 220–228
Shih AH, Holland EC (2006) Platelet-derived growth factor (PDGF) and glial tumorigenesis. Cancer Lett 232: 139–147
Siebzehnrubl FA, Jeske I, Müller D, Buslei R, Coras R, Hahnen E, Huttner HB, Corbeil D, Kaesbauer J, Appl T, von Hörsten S, Blümcke I (2008) Spontaneous in vitro transformation of adult neural precursors into stem-like cancer cells. Brain Pathol 19: 399–408
Sihto H, Sarlomo-Rikala M, Tynninen O, Tanner M, Andersson LC, Franssila K, Nupponen NN, Joensuu H (2005) KIT and platelet-derived growth factor receptor alpha tyrosine kinase gene mutations and KIT amplifications in human solid tumors. J Clin Oncol 23: 49–57
Smith JS, Wang XY, Qian J, Hosek SM, Scheithauer BW, Jenkins RB, James CD (2000) Amplification of the platelet-derived growth factor receptor-A (PDGFRA) gene occurs in oligodendrogliomas with grade IV anaplastic features. J Neuropathol Exp Neurol 59: 495–503
Takei H, Yogeswaren ST, Wong KK, Mehta V, Chintagumpala M, Dauser RC, Lau CC, Adesina AM (2008) Expression of oligodendroglial differentiation markers in pilocytic astrocytomas identifies two clinical subsets and shows a significant correlation with proliferation index and progression free survival. J Neuro Oncol 86: 183–190
Thorarinsdottir HK, Santi M, McCarter R, Rushing EJ, Cornelison R, Jales A, MacDonald TJ (2008) Protein expression of platelet-derived growth factor receptor correlates with malignant histology and PTEN with survival in childhood gliomas. Clin Cancer Res 14: 3386–3394
Uhrbom L, Hesselager G, Nister M, Westermark B (1998) Induction of brain tumors in mice using a recombinant platelet-derived growth factor B-chain retrovirus. Cancer Res 58: 5275–5279
Varela M, Ranuncolo SM, Morand A, Lastiri J, De Kier Joffe EB, Puricelli LI, Pallotta MG (2004) EGF-R and PDGF-R, but not bcl-2, overexpression predict overall survival in patients with low-grade astrocytomas. J Surg Oncol 86: 34–40
Wen PY, Kesari S (2008) Malignant gliomas in adults. N Engl J Med 359: 492–507
Wen PY, Yung WKA, Lamborn KR, Dahia PL, Wang YF, Peng B, Abrey LE, Raizer J, Cloughesy TF, Fink K, Gilbert M, Chang S, Junck L, Schiff D, Lieberman F, Fine HA, Mehta M, Robins HI, DeAngelis LM, Groves MD, Puduvalli VK, Levin V, Conrad C, Maher EA, Aldape K, Hayes M, Letvak L, Egorin MJ, Capdeville R, Kaplan R, Murgo AJ, Stiles C, Prados MD (2006) Phase I/II study of imatinib mesylate for recurrent malignant gliomas: North American Brain Tumor Consortium Study 99-08. Clin Cancer Res 12: 4899–4907
Westermark B, Heldin CH, Nister M (1995) Platelet-derived growth factor in human glioma. Glia 15: 257–263
Acknowledgements
OM is a recipient of a PhD fellowship (SFRH/BD/36463/2007) from Fundação para a Ciência e a Tecnologia (FCT), Portugal. JSRF, MBKL, AM, NT, KF and AA are funded by Breakthrough Breast Cancer. This study was supported in part by Pfizer/Sociedade de Ciências Médicas de Lisboa with the prize: ‘Research in oncology diseases, Professor Francisco Gentil’ and Breakthrough Breast Cancer.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Martinho, O., Longatto-Filho, A., Lambros, M. et al. Expression, mutation and copy number analysis of platelet-derived growth factor receptor A (PDGFRA) and its ligand PDGFA in gliomas. Br J Cancer 101, 973–982 (2009). https://doi.org/10.1038/sj.bjc.6605225
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6605225
Keywords
This article is cited by
-
Valtrate, an iridoid compound in Valeriana, elicits anti-glioblastoma activity through inhibition of the PDGFRA/MEK/ERK signaling pathway
Journal of Translational Medicine (2023)
-
Diffuse paediatric cerebellar glioma: two identical imaging phenotypes of an extremely rare entity with disparate pathology
Child's Nervous System (2023)
-
Prognostic stratification for IDH-wild-type lower-grade astrocytoma by Sanger sequencing and copy-number alteration analysis with MLPA
Scientific Reports (2021)
-
Chondroitin sulfate synthase 1 enhances proliferation of glioblastoma by modulating PDGFRA stability
Oncogenesis (2020)
-
Tumor Development and Angiogenesis in Adult Brain Tumor: Glioblastoma
Molecular Neurobiology (2020)