Abstract
A Valine residue at position 105 of the GSTP1 protein results in decreased enzyme activity. As nuclear GSTP1 activity decreases irinotecan cytotoxicity, Val-allele carriers may benefit more from irinotecan chemotherapy. Our aim was to investigate the association of GSTP1 genotype with treatment outcome of irinotecan. Progression-free survival (PFS) and toxicity were determined in 267 metastatic colorectal cancer (MCRC) patients who were treated with first-line capecitabine (CAP) plus irinotecan (CAPIRI), or CAP single agent in a prospective randomised phase III trial (CAIRO). GSTP1 genotype was determined by Pyrosequencing. Patients receiving CAP showed a PFS of 6.6 (Ile/Ile), 6.0 (Ile/Val) and 6.5 months (Val/Val); compared to 7.0 (Ile/Ile), 8.8 (Ile/Val) and 9.2 months (Val/Val) with CAPIRI. Median PFS was 2.7 months longer in Val-allele carriers treated with CAPIRI compared to CAP (P=0.005). Patients with the Ile/Ile genotype showed similar PFS with CAPIRI and CAP (7.0 compared to 6.6 months, P=0.972). Toxicity did not differ significantly among genotypes. GSTP1 codon 105 polymorphism may be predictive for the response to irinotecan-based chemotherapy in patients with MCRC, with the Val-allele being associated with a better outcome. Ile/Ile genotype patients do not appear to benefit from the addition of irinotecan to CAP.
Similar content being viewed by others
Main
The topo-isomerase I inhibitor irinotecan is an effective antitumour agent that is frequently used in the treatment of patients with metastatic colorectal cancer (MCRC) (Punt, 2004). Irinotecan may lead to serious and potentially life-threatening side effects, and not all patients respond to irinotecan. Therefore, pharmacokinetic and pharmacogenomic studies are warranted to predict which patients are most likely to benefit from irinotecan-based chemotherapy (Pander et al, 2007).
The metabolic fate of irinotecan has been extensively studied. Briefly, the (nearly) inactive prodrug irinotecan is metabolised to SN-38 by the carboxylesterases in the liver. SN-38 is highly active and inhibits topo-isomerase I, thereby interfering with DNA replication and ultimately leading to cell death of dividing cells.
The active metabolite SN-38 is glucuronidated to the inactive SN-38-G by uridine diphosphate glucuronosyl transferases (UGTs) (Iyer et al, 1998). An alternative metabolic route leads to the formation of APC (7-ethyl-10-[4-N-(5-aminopentanoic acid)-1-piperidino]-carbonyloxycamptothecin) by CYP3A4 and CYP3A5. Differences in systemic exposure to irinotecan and SN-38 are to some extent explained by genetic variations in UGT1A1 (Paoluzzi et al, 2004) but not CYP3A (de Jong et al, 2006). Several membrane efflux pumps have a function in the bio-distribution of irinotecan and its metabolites, of which ABCB1 and ABCC2 are of particular interest (de Jong et al, 2007; Kweekel et al, 2008). Much effort has also been made to explore associations between polymorphisms in UGTs and either toxicity or antitumour response of irinotecan. Although there is evidence that a decreased glucuronidation (UGT1A1*28 polymorphism) causes an increased risk of neutropenia and neutropenic fever (Mathijssen et al, 2003; Kweekel et al, 2008), data regarding the antitumour effects of irinotecan-based chemotherapy are contradicting. This may be because of the fact that systemic irinotecan levels are different from intratumoural concentrations, and also because of differences in the capacity of a tumour to metabolise or excrete the drug. An elevated expression of UGTs or membrane pumps may prevent or limit irinotecan-induced cell death in cancerous tissue, by causing a resistant phenotype. In this respect, the intratumoural expression of a wide range of proteins has been studied.
One of the proteins with an elevated expression in multidrug-resistant cell lines is glutathione-S-transferase pi (GSTP1) (Tew, 1994). GSTP1 has multiple functions, of which the enzymatic conjugation of glutathione (GSH) to xenobiotics is the most widely known. Irinotecan or SN-38 are not known as substrates for this conjugation reaction, but in vitro experiments show that if nuclear expression of GSTP1 is decreased using a mushroom lectin, colonic HCT8 cells are more sensitive to irinotecan (Goto et al, 2002). Therefore, GSTP1 may have an important function in the clinical efficacy of irinotecan and/or its metabolites. In addition, GSTP1 is a polymorphic gene, and the codon 105 polymorphism (313A>G, or Ile105Val) influences the geometry of the hydrophobic-binding site of GSTP1 enzyme (Zimniak et al, 1994). This results in differences in enzyme specificity and activity (Zimniak et al, 1994; Watson et al, 1998), which may influence irinotecan cytotoxicity. To our knowledge, the association between GSTP1 polymorphisms and clinical outcome in patients treated with irinotecan has not yet been explored in detail. Therefore, the aim of this study was to investigate the associations of GSTP1 Ile105Val with progression-free survival (PFS) of MCRC patients treated with irinotecan-containing chemotherapy.
Patients and methods
Subjects
Blood samples were obtained from patients enrolled in a multicenter phase III trial, the CAIRO study of the Dutch Colorectal Cancer Group (DCCG), of which the results have been published recently (Koopman et al, 2007). We refer to this article for a detailed description of eligibility criteria and response or toxicity evaluation. In summary, patients with MCRC were allocated to sequential (regimen A) or combination treatment (regimen B). Regimen A consisted of first-line capecitabine (1250 mg m−2 day−1 b.i.d. on days 1–14, every 3 weeks: CAP), second-line irinotecan (350 mg m−2 day−1 on day 1 every 3 weeks) and third-line CAP (1000 mg m−2 day−1 b.i.d. on days 1–14 every 3 weeks) plus oxaliplatin (130 mg m−2 on day 1 every 3 weeks). Regimen B consisted of first-line CAP (1000 mg m−2 day−1 b.i.d. on days 1–14, every 3 weeks) plus irinotecan (250 mg m−2 day−1 on day 1 every 3 weeks: CAPIRI), followed by second-line CAP plus oxaliplatin (as described in regimen A).
Dose reductions were performed for CAP in case of grades 2–4 toxicity as described previously (Van Cutsem et al, 2001). An initial irinotecan dose reduction to 80% in cycle 1 was recommended in case of: age >70 years, WHO performance status 2 and/or serum bilirubin 1–1.5 × upper normal limit. If well tolerated, the dose was escalated to 100% in subsequent cycles. In all patients, the irinotecan dose was reduced with 25% relative to the previous cycle in case of any grades 3–4 toxicity with the exception of nausea/vomiting without adequate prophylaxis. If these toxicities recurred despite dose reduction, the dose was reduced to 50% and upon next recurrence the treatment was discontinued. Prophylactic use of haematological growth factors or loperamide was not permitted. The accrual period was from January 2003 to December 2004, and EDTA blood samples for genotyping were collected from December 2003 to March 2005 after a protocol amendment. The objective of this amendment was to perform genetic association studies regarding antitumour response and toxicity. The study protocol and the amendment were approved by the local ethical committees. Written informed consent was obtained from all patients participating in the genetic association study before blood collection. DNA was obtained from 267 patients (regimen B: 141 subjects; regimen A: 126). Tumour evaluation was performed every three cycles according to the RECIST criteria (Therasse et al, 2000), toxicity according to US National Cancer Institute Common Toxicity Criteria, version 2.0. All results were blinded with respect to genotype.
Genotyping
Genomic DNA was isolated from peripheral blood cells (MagnaPure Total Nucleic Acid Isolation Kit I on MagnaPure LC (Roche Diagnostics, Mannheim, Germany)). Chromosomal DNA was quantified using Nanodrop (Isogen, IJsselstein, The Netherlands) and diluted to 10 ng μl−1.
Primers for the GSTP1 Ile105Val polymorphism (rs1695) and pyrosequence materials were obtained from Isogen Life Sciences (IJsselstein, The Netherlands), Sepharose beads from Amersham (Uppsala, Sweden). PCR reactions were performed using Hotstart PCR mastermix (Qiagen, Hilden, Germany) on the MyCycler (Biorad, Veenendaal, The Netherlands). Pyrosequence analysis was performed on a Pyrosequencer 96MA (Biotage, Sweden). PCR reactions were as follows: each reaction contained 10 ng of DNA, and 5 pmol of each PCR primer (forward: 5′-AGGACCTCCGCTGCAAATAC-3′, reverse 5′-CTGGTGCAGATGCTCACATAGTT-3′) in a total of 12 μl. Cycle conditions were as follows: initial denaturation for 15 min at 95°C, 35 cycles of 95°C−55°C−72°C each for 30 s, ended by 10 min at 72°C. The pyrosequence reactions were performed according to the manufacturer's protocol. The sequence to analyse was A/GTCTCCCTCAT using the forward sequence primer 5′-CTCCGCTGCAAATAC-3′.
Statistics
Possible associations of GSTP1 genotype with the incidence of diarrhoea grades 3–4, febrile neutropenia and overall grades 3–4 toxicity according to the genotype were tested with a Fisher's exact test. The PFS was calculated from the date of randomisation to the first observation of disease progression or death from any cause reported after first-line treatment. The PFS curves were estimated using the Kaplan–Meier method and compared using the log-rank test. Multivariate analysis of PFS was performed by means of a Cox proportional hazard model. All tests were two-sided and P-values <0.05 were considered significant. All follow up data received before March 2008 were included in this analysis, representing a median follow up of 41 months. All analyses were performed using SAS 9.1 and S-plus 6.2 software.
Results
Patient characteristics are shown in Table 1. Patient ethnicity was not recorded but the vast majority of patients were of Caucasian descent. Genotyping the Ile105Val polymorphism was successful in all 267 patients (100%). Overall genotype frequencies for the GSTP1 Ile105Val polymorphism were as follows: Ile/Ile 107(40.3%), Ile/Val 129(48.1%) and Val/Val 31(11.6%). The genotype distribution was in Hardy–Weinberg equilibrium and the allele frequencies (Ile 0.64, Val 0.36) were found in concordance with HapMap data of Caucasian individuals published online (http://www.ncbi.nlm.nih.gov/SNP/snp_ref.cgi?rs=1695).
Clinical efficacy
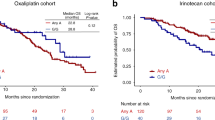
All 267 patients were evaluable for analysis of PFS: 126 patients received first-line chemotherapy with CAP (regimen A), and 141 patients received first-line combination therapy with irinotecan and CAP (CAPIRI, regimen B). For each separate genotype, we compared PFS of patients receiving CAP with patients receiving CAPIRI (Table 2, Figure 1). Overall, median PFS was longer for patients receiving CAPIRI: 8.3 (95% confidence intervals (CI): 7.6–8.8) months compared to 6.3 months (95% CI: 5.8–6.9, CAP). This survival benefit from CAPIRI treatment was observed in patients of the Ile/Val and Val/Val genotypes, but not in patients with the Ile/Ile genotype. The median PFS for the separate genotypes receiving CAP were as follows: 6.6 months (Ile/Ile, n=43), 6.0 months (Ile/Val, n=65) and 6.5 months (Val/Val, n=18), P=0.886. In the CAPIRI regimen, median PFS were 7.0 months (Ile/Ile, n=64), 8.8 months (Ile/Val, n=64) and 9.2 months (Val/Val, n=13), P=0.078. Ile/Ile homozygotes receiving CAP had a similar median PFS compared to Val-allele carriers (median 6.2 months, P=0.647). However, the Ile/Ile genotype receiving CAPIRI had a significantly lower median PFS compared to the other genotypes (median 7.0 months compared to 8.9 months, P=0.037). Multivariate Cox regression analysis reveals that PFS for the Ile/Ile genotype is not significantly different depending on the use of CAP or CAPIRI (P=0.972), which is in contrast to Val-allele carriers (P=0.005). This result suggests that Ile/Ile individuals do not benefit from the addition of irinotecan to CAP.
Kaplan–Meier plot of progression-free survival (PFS). Solid lines: Ile/Ile, dotted lines: Ile/Val+Val/Val. If we compare median PFS of Ile/Ile patients receiving CAP with those receiving CAPIRI, we see a nonsignificant difference (P=0.972), whereas median PFS of Val carriers is significantly better in the CAPIRI regimen (P<0.005). The full-colour version is available online.
Toxicity
As was expected, the overall incidence of grades 3–4 diarrhoea and febrile neutropenia was higher in patients treated with CAPIRI (26.2%) compared to CAP (7.1%, P<0.001).
There were no statistically significant differences between GSTP1 genotypes in the incidence of overall grades 3–4 toxicity or grades 3–4 diarrhoea with CAP (Table 3).
Discussion
This is the largest study to date that investigates a possible association of the GSTP1 codon 105 polymorphism with response and toxicity to irinotecan. We demonstrate that, as opposed to the overall study population, Ile/Ile carriers do not benefit from the addition of irinotecan to CAP. A number of studies have been conducted to investigate the GSTP1 polymorphism with respect to the treatment effects of other chemotherapeutic compounds, such as busulfan (Zwaveling et al, 2008), melphalan (Kuhne et al, 2008), cyclophosphamide (Zhong et al, 2006), oxaliplatin (Stoehlmacher et al, 2002; Ruzzo et al, 2007) and cisplatin (Goekkurt et al, 2006). In vitro data (Goto et al, 2002) have shown that the presence of GSTP1 in the cell nucleus protects the cell from irinotecan-induced apoptosis. As irinotecan or its active metabolites are not known to be substrates of the GSTP1 enzyme, we hypothesise that GSH conjugation of reactive oxygen species originating from irinotecan exposure may contribute to this effect. The enzymatic activity of GSTP1 Val105 was found to be lower compared to GSTP1 Ile105 (Watson et al, 1998), and patients with Val/Val and Ile/Val may therefore benefit more from irinotecan-induced oxidative damage, compared to the Ile/Ile genotype. Our findings now for the first time suggest a possible relationship between the GSTP1 genotype and irinotecan efficacy in cancer patients.
Based on the results of this study, one may question the use of irinotecan in MCRC patients with the Ile/Ile genotype, as no benefit in median PFS was observed while the incidence of irinotecan-associated toxicity was unchanged.
A recent (FOCUS) study reports a multimarker analysis of, among others, GSTP1 codon 105, in a large set of patients newly presenting with MCRC (Braun et al, 2008). Patient characteristics seem comparable with this study, but instead of CAP, 5-fluorouracil (5-FU) was used. The GSTP1 genotype distribution in the FOCUS study was different from this study (with a remarkable 43% of patients being of the homozygote mutant, GG, genotype). Although the authors do not provide a detailed description of GSTP1 associations with time to first-line treatment failure, it is suggested that this genotype is not associated with differences in response between 5-FU plus irinotecan treatment and 5-FU alone. This finding is in contrast to the current results, but may be related to the use of 5-FU instead of CAP (Seymour et al, 2007). In addition, both studies report different toxicity patterns and –incidence relating to irinotecan (Koopman et al, 2006). The same unknown mechanisms underlying these differences may also affect the association between GSTP1 genotypes and PFS.
A possible limitation to this study is the fact that samples were obtained at a median of 5 months after inclusion, that is, most patients who donated a sample were either in first- or second-line therapy. The overall genotype distribution is not different from data on Caucasians with colorectal carcinoma (Ile/Ile 47, Ile/Val 46 and Val/Val 6%) (Skjelbred et al, 2007). A similar distribution is also found in CAPIRI patients, but not in those receiving CAP. This may be a sign of selection bias; however, the genotype distributions in both regimens are in Hardy–Weinberg equilibrium, and the baseline characteristics of the patients randomised to CAP do not differ significantly from the overall patient characteristics of the complete cohort of the original study (P>0.2 for all characteristics, data not shown) (Koopman et al, 2007). In addition, a recent study found no association of GSTP1 genotype with overall survival or PFS in MCRC patients (Le Morvan et al, 2007), indicating that GSTP1 is not a prognostic marker. Therefore, selection bias seems unlikely.
In summary, the results of this study suggest that patients with the Ile/Ile genotype do not benefit, in terms of PFS, from the addition of irinotecan to CAP, in contrast to the Ile/Val and Val/Val genotype. This is the first study reporting an association of the GSTP1 codon 105 variants with the clinical efficacy of irinotecan. If confirmed, this observation has important implications for the selection of MCRC patients who are eligible for treatment with irinotecan.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Braun MS, Richman SD, Quirke P, Daly C, Adlard JW, Elliott F, Barrett JH, Selby P, Meade AM, Stephens RJ, Parmar MK, Seymour MT (2008) Predictive biomarkers of chemotherapy efficacy in colorectal cancer: results from the UK MRC FOCUS trial. J Clin Oncol 26: 2690–2698
de Jong FA, de Jonge MJ, Verweij J, Mathijssen RH (2006) Role of pharmacogenetics in irinotecan therapy. Cancer Lett 234: 90–106
de Jong FA, Scott-Horton TJ, Kroetz DL, McLeod HL, Friberg LE, Mathijssen RH, Verweij J, Marsh S, Sparreboom A (2007) Irinotecan-induced diarrhea: functional significance of the polymorphic ABCC2 transporter protein. Clin Pharmacol Ther 81: 42–49
Goekkurt E, Hoehn S, Wolschke C, Wittmer C, Stueber C, Hossfeld DK, Stoehlmacher J (2006) Polymorphisms of glutathione S-transferases (GST) and thymidylate synthase (TS)--novel predictors for response and survival in gastric cancer patients. Br J Cancer 94: 281–286
Goto S, Kamada K, Soh Y, Ihara Y, Kondo T (2002) Significance of nuclear glutathione S-transferase pi in resistance to anti-cancer drugs. Jpn J Cancer Res 93: 1047–1056
Iyer L, King CD, Whitington PF, Green MD, Roy SK, Tephly TR, Coffman BL, Ratain MJ (1998) Genetic predisposition to the metabolism of irinotecan (CPT-11). Role of uridine diphosphate glucuronosyltransferase isoform 1A1 in the glucuronidation of its active metabolite (SN-38) in human liver microsomes. J Clin Invest 101: 847–854
Koopman M, Antonini NF, Douma J, Wals J, Honkoop AH, Erdkamp FL, de Jong RS, Rodenburg CJ, Vreugdenhil G, kkermans-Vogelaar JM, Punt CJ (2006) Randomised study of sequential vs combination chemotherapy with capecitabine, irinotecan and oxaliplatin in advanced colorectal cancer, an interim safety analysis. A Dutch Colorectal Cancer Group (DCCG) phase III study. Ann Oncol 17: 1523–1528
Koopman M, Antonini NF, Douma J, Wals J, Honkoop AH, Erdkamp FL, de Jong RS, Rodenburg CJ, Vreugdenhil G, Loosveld OJ, van BA, Sinnige HA, Creemers GJ, Tesselaar ME, Slee PH, Werter MJ, Mol L, Dalesio O, Punt CJ (2007) Sequential vs combination chemotherapy with capecitabine, irinotecan, and oxaliplatin in advanced colorectal cancer (CAIRO): a phase III randomised controlled trial. Lancet 370: 135–142
Kuhne A, Sezer O, Heider U, Meineke I, Muhlke S, Niere W, Overbeck T, Hohloch K, Trumper L, Brockmoller J, Kaiser R (2008) Population pharmacokinetics of melphalan and glutathione S-transferase polymorphisms in relation to side effects. Clin Pharmacol Ther 83: 749–757
Kweekel DM, Gelderblom H, Straaten van der T, Antonini NF, Punt CJ, Guchelaar H-J (2008) UGT1A1*28 genotype irinotecan dosage in patients with metastatic colorectal cancer-a DCCG study. Br J Cancer 99: 275–282
Le Morvan V, Smith D, Laurand A, Brouste V, Bellott R, Soubeyran I, Mathoulin-Pelissier S, Robert J (2007) Determination of ERCC2 Lys751Gln and GSTP1 Ile105Val gene polymorphisms in colorectal cancer patients: relationships with treatment outcome. Pharmacogenomics 8: 1693–1703
Mathijssen RH, Marsh S, Karlsson MO, Xie R, Baker SD, Verweij J, Sparreboom A, McLeod HL (2003) Irinotecan pathway genotype analysis to predict pharmacokinetics. Clin Cancer Res 9: 3246–3253
Pander J, Gelderblom H, Guchelaar HJ (2007) Insights into the role of heritable genetic variation in the pharmacokinetics and pharmacodynamics of anticancer drugs. Expert Opin Pharmacother 8: 1197–1210
Paoluzzi L, Singh AS, Price DK, Danesi R, Mathijssen RH, Verweij J, Figg WD, Sparreboom A (2004) Influence of genetic variants in UGT1A1 and UGT1A9 on the in vivo glucuronidation of SN-38. J Clin Pharmacol 44: 854–860
Punt CJ (2004) New options and old dilemmas in the treatment of patients with advanced colorectal cancer. Ann Oncol 15: 1453–1459
Ruzzo A, Graziano F, Loupakis F, Rulli E, Canestrari E, Santini D, Catalano V, Ficarelli R, Maltese P, Bisonni R, Masi G, Schiavon G, Giordani P, Giustini L, Falcone A, Tonini G, Silva R, Mattioli R, Floriani I, Magnani M (2007) Pharmacogenetic profiling in patients with advanced colorectal cancer treated with first-line FOLFOX-4 chemotherapy. J Clin Oncol 25: 1247–1254
Seymour MT, Maughan TS, Ledermann JA, Topham C, James R, Gwyther SJ, Smith DB, Shepherd S, Maraveyas A, Ferry DR, Meade AM, Thompson L, Griffiths GO, Parmar MK, Stephens RJ (2007) Different strategies of sequential and combination chemotherapy for patients with poor prognosis advanced colorectal cancer (MRC FOCUS): a randomised controlled trial. Lancet 370: 143–152
Skjelbred CF, Saebo M, Hjartaker A, Grotmol T, Hansteen IL, Tveit KM, Hoff G, Kure EH (2007) Meat, vegetables and genetic polymorphisms and the risk of colorectal carcinomas and adenomas. BMC Cancer 7: 228
Stoehlmacher J, Park DJ, Zhang W, Groshen S, Tsao-Wei DD, Yu MC, Lenz HJ (2002) Association between glutathione S-transferase P1, T1, and M1 genetic polymorphism and survival of patients with metastatic colorectal cancer. J Natl Cancer Inst 94: 936–942
Tew KD (1994) Glutathione-associated enzymes in anticancer drug resistance. Cancer Res 54: 4313–4320
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van GM, van Oosterom AT, Christian MC, Gwyther SG (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92: 205–216
Van Cutsem E, Twelves C, Cassidy J, Allman D, Bajetta E, Boyer M, Bugat R, Findlay M, Frings S, Jahn M, McKendrick J, Osterwalder B, Perez-Manga G, Rosso R, Rougier P, Schmiegel WH, Seitz JF, Thompson P, Vieitez JM, Weitzel C, Harper P (2001) Oral capecitabine compared with intravenous fluorouracil plus leucovorin in patients with metastatic colorectal cancer: results of a large phase III study. J Clin Oncol 19: 4097–4106
Watson MA, Stewart RK, Smith GB, Massey TE, Bell DA (1998) Human glutathione S-transferase P1 polymorphisms: relationship to lung tissue enzyme activity and population frequency distribution. Carcinogenesis 19: 275–280
Zhong S, Huang M, Yang X, Liang L, Wang Y, Romkes M, Duan W, Chan E, Zhou SF (2006) Relationship of glutathione S-transferase genotypes with side-effects of pulsed cyclophosphamide therapy in patients with systemic lupus erythematosus. Br J Clin Pharmacol 62: 457–472
Zimniak P, Nanduri B, Pikula S, Bandorowicz-Pikula J, Singhal SS, Srivastava SK, Awasthi S, Awasthi YC (1994) Naturally occurring human glutathione S-transferase GSTP1-1 isoforms with isoleucine and valine in position 104 differ in enzymic properties. Eur J Biochem 224: 893–899
Zwaveling J, Press RR, Bredius RGM, Van der Straaten RJHM, Den Hartigh J, Bartelink IH, Boelens JJ, Guchelaar HJ (2008) Glutathione S-transferase polymorphisms are not associated with population pharmacokinetic parameters of busulfan in pediatric patients. Ther Drug Monit 30: 504–510
Acknowledgements
The Dutch Colorectal Cancer Group (DCCG) CAIRO study was supported by the CKTO (Grant 2002-07) and by unrestricted scientific grants from Roche, Sanofi-Aventis and Pfizer. We thank the following CAIRO team members for participating in the pharmacogenetic side study: J van der Hoeven-Amstelveen; D Richel, B de Valk-Amsterdam; J Douma-Arnhem; P Nieboer-Assen; F Valster-Bergen op Zoom; G Ras, O Loosveld-Breda; D Kehrer-Capelle a/d IJssel; M Bos-Delft; H Sinnige, C Knibbeler-Den Bosch; W Van Deijk, H Sleeboom-Den Haag; E Muller-Doetinchem; E Balk-Ede; G Creemers-Eindhoven; R de Jong-Groningen; P Zoon-Harderwijk; J Wals-Heerlen; M Polee-Leeuwarden; M Tesselaar-Leiden; R Brouwer-Leidschendam; P de Jong, P Slee-Nieuwegein; C Punt, H Oosten-Nijmegen; M Kuper-Oss; M den Boer-Roermond; F de Jongh-Rotterdam; G Veldhuis-Sneek; D ten Bokkel Huinink-Utrecht; A van Bochove-Zaandam.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Kweekel, D., Koopman, M., Antonini, N. et al. GSTP1 Ile105Val polymorphism correlates with progression-free survival in MCRC patients treated with or without irinotecan: a study of the Dutch Colorectal Cancer Group. Br J Cancer 99, 1316–1321 (2008). https://doi.org/10.1038/sj.bjc.6604654
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6604654
Keywords
This article is cited by
-
Relation between GSTP1 polymorphism and oxidative stress in patients with hepatocellular carcinoma
Journal of the Egyptian National Cancer Institute (2020)
-
Predictive value of GSTP1 Ile105Val polymorphism in clinical outcomes of chemotherapy in gastric and colorectal cancers: a systematic review and meta-analysis
Cancer Chemotherapy and Pharmacology (2016)
-
Genetic Polymorphisms of Cytochrome P4501A1 (CYP1A1) and Glutathione S-Transferase P1 (GSTP1) and Risk of Hepatocellular Carcinoma Among Chronic Hepatitis C Patients in Egypt
Biochemical Genetics (2016)
-
Pharmacogenomics and personalized medicine: a review focused on their application in the Chinese population
Acta Pharmacologica Sinica (2015)
-
Glutathione S-transferase Pi expression predicts response to adjuvant chemotherapy for stage C colon cancer: a matched historical control study
BMC Cancer (2012)