Abstract
The relationship between tumour stage, grade (Fuhrman), performance status (ECOG), a combined score (UCLA Integrated Staging System, UISS), systemic inflammatory response (elevated C-reactive protein concentration), and cancer-specific survival was examined in patients undergoing potentially curative resection for renal clear cell cancer (n=100). On univariate survival analysis, sex (P=0.050), tumour stage (P=0.001), Fuhrman grade (P<0.001), UISS (P<0.001), C-reactive protein (P=0.002) were significant predictors of survival. On multivariate analysis with sex, UISS and C-reactive protein entered as covariates, only UISS (HR 2.70, 95% CI 1.00–7.30, P=0.050) and C-reactive protein (HR 4.00, 95% CI 1.21–13.31, P=0.024) were significant independent predictors of survival. The presence of a preoperative systemic inflammatory response predicts poor cancer-specific survival in patients who have undergone potentially curative resection for renal clear cell cancer.
Similar content being viewed by others
Main
Renal cell cancer, although the twelfth most common cause of cancer death is one of the most lethal urological cancers. Each year in the UK, there are approximately 3500 new cases and approximately 30% of patients present with metastases. Overall survival is poor; even in those who undergo potentially curative resection, only approximately half survive 5 years (Cancerstats, www.cancerresearchuk.org).
The ideal prognostic score for patients undergoing potentially curative resection of a primary renal cancer should clearly distinguish those who will eventually succumb to the disease from those who are cured. While TNM stage has been widely used, it fails to provide clear separation between these groups. This has lead to the development of a number of cumulative prognostic scores including TNM stage. TNM stage has been combined with tumour grade and performance status to form the UCLA Integrated Staging System (UISS, Zisman et al, 2002).
It is recognised that in addition to tumour stage and proliferative activity, disease progression is dependent on a complex interaction of the tumour and host inflammatory response (Balkwill and Mantovani, 2001; Coussens and Werb, 2002; Vakkila and Lotze, 2004). Recently, the systemic inflammatory response, as evidenced by elevated circulating concentrations of C-reactive protein, has been shown to be a stage independent prognostic factor in patients undergoing potentially curative resection for colorectal cancer (McMillan et al, 2003), pancreatic cancer (Jamieson et al, 2005) and urinary bladder cancer (Hilmy et al, 2005).
The aim of the present study was to examine the prognostic value of the systemic inflammatory response in patients undergoing potentially curative resection for renal cancer.
Patients and methods
Patients with renal clear cell cancer, who, on the basis of surgical findings and preoperative computed tomography of chest abdomen and pelvis underwent potentially curative resection between August 1996 and November 2004 in the West of Scotland, were included in the study. No patient had metastatic disease and the tumour confined to the kidney. In the case of T3/T4 tumours all macroscopic tumour was removed with clear resection margins.
Patients were staged pathologically according to the 1997 UICC TNM classification of renal tumours (Sobin and Wittekind, 1997). Tumours were graded according to criteria set out by Fuhrman et al (1982). Tumour stage, grade and ECOG-ps were collated into the UISS (Zisman et al, 2002, Table 1).
Data for 1996–2000 (n=57) were collected retrospectively and that for 2001–2004 (n=43) prospectively. Clinical stage and performance status (Eastern Cooperative Oncology Group, ECOG-ps) were recorded prior to surgery. Also, routine laboratory measurement of C-reactive protein was carried out.
The Research Ethics Committee of North Glasgow NHS Trust approved the study.
Routine laboratory measurement of patient's serum for C-reactive protein concentration was performed. The limit of detection of the assay was a C-reactive protein concentration lower than 6 mg l−1. The coefficient of variation, over the range of measurement, was less than 5% as established by routine quality control procedures. C-reactive protein measurement of greater than 10 mg l−1 was considered to indicate the presence of systemic inflammatory response (O'Gorman et al, 2000).
Statistics
Comparisons between groups of patients were carried out using contingency table analysis (X2) as appropriate. Survival analysis was performed using the Cox's proportional-hazards model. Deaths up to the end of October 2005 were included in the analysis. Multivariate survival analysis was performed using a stepwise backward procedure to derive a final model of the variables that had a significant independent relationship with survival. To remove a variable from the model, the corresponding P-value had to be greater than 0.10. Analysis was performed using SPSS software (SPSS Inc., Chicago, IL, USA).
Results
The characteristics of patients with renal cancer who underwent potentially curative resection (n=100) are shown in Table 2. The majority was male, over the age of 60 years, had good performance status, low T stage (median tumour volume 178 cm3) and were defined as UISS intermediate risk. Approximately, 40% had an elevated C-reactive protein concentration (>10 mg l−1).
The minimum follow-up was 12 months; the median follow-up of the survivors was 59 months. During this period 25 patients died; 18 patients of their cancer and seven of intercurrent disease. On univariate survival analysis, sex (P=0.050), tumour stage (P⩽0.001), Fuhrman grade (P<0.001), UISS (P<0.001) and C-reactive protein (P<0.01) were significant predictors of cancer-specific survival.
On multivariate analysis with sex, tumour stage, Fuhrman grade, performance status and C-reactive protein entered as covariates, only sex (HR 0.25, 95% CI 0.06–0.99, P=0.048), Fuhrman grade (HR 2.91, 95% CI 1.29–6.56, P=0.010) and C-reactive protein (HR 7.67, 95% CI 1.64–35.84, P=0.010) were significant independent predictors of cancer-specific survival.
On multivariate analysis with sex, UISS and C-reactive protein entered as covariates, only UISS (HR 2.70, 95% CI 1.00–7.30, P=0.050) and C-reactive protein (HR 4.00, 95% CI 1.21–13.31, P=0.024) were significant independent predictors of cancer-specific survival. A greater proportion of females compared with males had Fuhrman grade I tumours (10 vs 29%, P=0.030, Fisher's exact test).
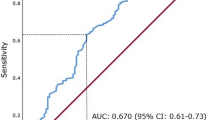
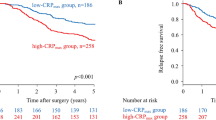
The relationship between the systemic inflammatory response and the clinicopathological characteristics are shown in Table 3. There was no significant difference in age or sex between the inflammatory and noninflammatory groups. An elevated C-reactive protein was associated with a greater number of patients with advanced tumour stage (P<0.01), increased grade (P<0.05), poorer performance status (P<0.01) and consequently a high UISS (P<0.01). Those patients with an elevated preoperative C-reactive protein concentration (>10 mg l−1) had a mean cancer-specific survival of 71 months compared with 96 months (P<0.001) in those patients with a C-reactive protein concentration in the normal range (⩽10 mg l−1).
In those patients with a UISS risk classified as ‘low’ or ‘intermediate’ (n=91) an elevated C-reactive protein concentration was associated with a decrease in cancer-specific survival (P=0.008, Figure 1).
Discussion
Surgical resection remains the only prospect for long-term survival in patients with renal clear cell cancer. Currently, in patients undergoing surgery prognosis is based on tumour stage and grade and performances status (UISS, Zisman et al, 2002). In the present study, the preoperative measurement of C-reactive protein provided additional prognostic information.
To our knowledge this is only the second study to examine the role C-reactive in predicting survival following potentially curative resection for renal cancer. Masuda et al (1998) in a retrospective study of 111 patients reported that C-reactive protein was a prognostic factor independent of tumour stage and grade. However, performance status was not considered and thresholds for C-reactive protein were not defined in the survival analysis.
Few studies have identified factors which give prognostic information in addition to the UISS criteria, namely T stage, Fuhrman grade and ECOG-ps, in patients undergoing potentially curative resection for renal cancer. Recently, Shvarts et al (2005) reported that tumour p53 expression was related to Fuhrman grade and displaced it in multivariate analysis. Similarly, Lam et al (2005) reported that tumour Ki-67, unlike carbonic anhydrase, was related to the degree of necrosis and had independent prognostic value. Further studies are required to determine whether an elevated C-reactive protein has prognostic value independent of these other biological factors, in particular Ki-67.
It has been previously shown that, in patients undergoing potentially curative surgery for colorectal and pancreatic cancer, approximately one-third and one-half respectively, of patients had elevated circulating concentration of C-reactive protein preoperatively and that these patients had a significantly lower cancer-specific survival (McMillan et al, 2003; Jamieson et al, 2005). It was of interest that, in the present study, the proportion of patients with an elevated preoperative C-reactive protein concentration was similar and that these patients also had a poorer outcome.
It may be that because C-reactive protein concentration has prognostic value independent of UISS criteria, it might be added to these criteria to improve the prediction outcome, in particular the large group of ‘low or intermediate risk’ patients with renal cancer. Indeed, this approach has recently been used to improve the prediction of outcome in patients who underwent potentially curative resection for colorectal cancer (Canna et al, 2004).
An elevated circulating C-reactive protein concentration is also an established poor prognostic factor in patients with metastatic renal cancer (Atzpodien et al, 2003; Bromwich et al, 2004; Casamassima et al, 2005). In our previous study of patients with metastatic renal cancer (Bromwich et al, 2004), approximately 70% had an elevated C-reactive protein (>10 mg l−1) compared with approximately 40% in the present study of primary operable disease. This is consistent with previous observations that the systemic inflammatory response increases with advancing disease (Mahmoud and Rivera, 2002). However, the basis of the independent relationship between an elevated C-reactive protein concentration and poor survival in renal cancer is not clear. There are a number of possible explanations. Firstly, that an elevated C-reactive protein identifies tumours capable of producing significant amounts of proinflammatory cytokines, in particular interleukin-6 (Kinoshita et al, 1999; McKeown et al, 2004) and therefore with the potential for more rapid growth of tumour cells (Jee et al, 2001; Trikha et al, 2003). Also, that an elevated C-reactive protein identifies those patients with T-lymphocyte impairment (Maccio et al, 1998; Canna et al, 2005) or patients with a proangiogenic environment (Kofler et al, 2005; Xavier et al, 2006) allowing unrestrained tumour growth and dissemination. Clearly, both these tumour and host mechanisms may be related and required for the greater malignant potential associated with an elevated C-reactive protein concentration.
This is a relatively small, partially retrospective study and requires verification in larger prospective cohorts. However, if an elevated C-reactive protein concentration is shown to offer prognostic value in addition to the current UISS criteria it would improve our staging of these patients. Moreover, C-reactive protein may offer a useful preoperative therapeutic target in patients undergoing potentially curative surgery for renal clear cell cancer.
In summary, the presence of a preoperative systemic inflammatory response predicts poor cancer-specific survival in patients who have undergone potentially curative resection for renal clear cell cancer.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Atzpodien J, Royston P, Wandert T, Reitz M, DGCIN – German Cooperative Renal Carcinoma Chemo-Immunotherapy Trials Group (2003) Metastatic renal carcinoma comprehensive prognostic system. Br J Cancer 88: 348–353
Balkwill F, Mantovani A (2001) Inflammation and cancer: back to Virchow? Lancet 357 (9255): 539–545
Bromwich E, McMillan DC, Lamb GW, Vasey PA, Aitchison M (2004) The systemic inflammatory response, performance status and survival in patients undergoing alpha-interferon treatment for advanced renal cancer. Br J Cancer 91: 1236–1238
Canna K, McArdle PA, McMillan DC, McNicol AM, Smith GW, McKee RF, McArdle CS (2005) The relationship between tumour T-lymphocyte infiltration, the systemic inflammatory response and survival in patients undergoing curative resection for colorectal cancer. Br J Cancer. 92: 651–654
Canna K, McMillan DC, McKee RF, McNicol AM, Horgan PG, McArdle CS (2004) Evaluation of a cumulative prognostic score based on the systemic inflammatory response in patients undergoing potentially curative surgery for colorectal cancer. Br J Cancer 90: 1707–1709
Casamassima A, Picciariello M, Quaranta M, Berardino R, Ranieri C, Paradiso A, Lorusso V, Guida M (2005) C-reactive protein: a biomarker of survival in patients with metastatic renal cell carcinoma treated with subcutaneous interleukin-2 based immunotherapy. J Urol 173: 52–55
Coussens LM, Werb Z (2002) Inflammation and cancer. Nature 420 (6917): 860–867
Fuhrman SA, Lasky LC, Limas C (1982) Prognostic significance of morphologic parameters in renal cell carcinoma. Am J Surg Pathol 6: 655–663
Hilmy M, Bartlett JM, Underwood MA, McMillan DC (2005) The relationship between the systemic inflammatory response and survival in patients with transitional cell carcinoma of the urinary bladder. Br J Cancer 92: 625–627
Jamieson NB, Glen P, McMillan DC, McKay CJ, Foulis AK, Carter R, Imrie CW (2005) Systemic inflammatory response predicts outcome in patients undergoing resection for ductal adenocarcinoma head of pancreas. Br J Cancer 92: 21–23
Jee SH, Shen SC, Chiu HC, Tsai WL, Kuo ML (2001) Overexpression of interleukin-6 in human basal cell carcinoma cell lines increases anti-apoptotic activity and tumorigenic potency. Oncogene 20: 198–208
Kinoshita T, Ito H, Miki C (1999) Serum interleukin-6 level reflects the tumor proliferative activity in patients with colorectal carcinoma. Cancer 85: 2526–2531
Kofler S, Nickel T, Weis M (2005) Role of cytokines in cardiovascular diseases: a focus on endothelial responses to inflammation. Clin Sci (London) 108: 205–213
Lam JS, Shvarts O, Said JW, Pantuck AJ, Seligson DB, Aldridge ME, Bui MH, Liu X, Horvath S, Figlin RA, Belldegrun AS (2005) Clinicopathologic and molecular correlations of necrosis in the primary tumor of patients with renal cell carcinoma. Cancer 103: 2517–2525
Maccio A, Lai P, Santona MC, Pagliara L, Melis GB, Mantovani G (1998) High serum levels of soluble IL-2 receptor, cytokines, and C reactive protein correlate with impairment of T cell response in patients with advanced epithelial ovarian cancer. Gynecol Oncol 69: 248–252
Mahmoud FA, Rivera NI (2002) The role of C-reactive protein as a prognostic indicator in advanced cancer. Curr Oncol Rep 4: 250–255
Masuda H, Kurita Y, Fukuta K, Mugiya S, Suzuki K, Fujita K (1998) Significant prognostic factors for 5-year survival after curative resection of renal cell carcinoma. Int J Urol 5: 418–422
McKeown DJ, Brown DJ, Kelly A, Wallace AM, McMillan DC (2004) The relationship between circulating concentrations of C-reactive protein, inflammatory cytokines and cytokine receptors in patients with non-small-cell lung cancer. Br J Cancer 91: 1993–1995
McMillan DC, Canna K, McArdle CS (2003) Systemic inflammatory response predicts survival following curative resection of colorectal cancer. Br J Surg 90: 215–219
O'Gorman P, McMillan DC, McArdle CS (2000) Prognostic factors in advanced gastrointestinal cancer patients with weight loss. Nutr Cancer 37: 36–40
Shvarts O, Seligson D, Lam J, Shi T, Horvath S, Figlin R, Belldegrun A, Pantuck AJ (2005) p53 is an independent predictor of tumor recurrence and progression after nephrectomy in patients with localized renal cell carcinoma. J Urol 173: 725–728
Sobin L, Wittekind C (1997) International Union Against Cancer (UICC): TNM Classification of Malignant Tumors 5th edn, pp 180–182. New York: Wiley-Liss
Trikha M, Corringham R, Klein B, Rossi JF (2003) Targeted anti-interleukin-6 monoclonal antibody therapy for cancer: a review of the rationale and clinical evidence. Clin Cancer Res 9: 4653–4665
Vakkila J, Lotze MT (2004) Inflammation and necrosis promote tumour growth. Nat Rev Immunol 4: 641–648
Xavier P, Belo L, Beires J, Rebelo I, Martinez-de-Oliveira J, Lunet N, Barros H (2006) Serum levels of VEGF and TNF-alpha and their association with C-reactive protein in patients with endometriosis. Arch Gynecol Obstet 273: 227–231
Zisman A, Pantuck AJ, Wieder J, Chao DH, Dorey F, Said JW, deKernion JB, Figlin RA, Belldegrun AS (2002) Risk group assessment and clinical outcome algorithm to predict the natural history of patients with surgically resected renal cell carcinoma. J Clin Oncol 20: 4559–4566
Acknowledgements
We gratefully acknowledge the funding provided by the ‘Fischer Foundation’, a charitable organisation dedicated to research in renal cancer. We also acknowledge the assistance of Mohamed Hadada and Emma Bromwich.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Lamb, G., McMillan, D., Ramsey, S. et al. The relationship between the preoperative systemic inflammatory response and cancer-specific survival in patients undergoing potentially curative resection for renal clear cell cancer. Br J Cancer 94, 781–784 (2006). https://doi.org/10.1038/sj.bjc.6603034
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6603034
Keywords
This article is cited by
-
The pretreatment erythrocyte sedimentation rate predicts survival outcomes after surgery and adjuvant radiotherapy for extremity soft tissue sarcoma
Radiation Oncology (2019)
-
Validation of the prognostic relevance of plasma C-reactive protein levels in soft-tissue sarcoma patients
British Journal of Cancer (2013)
-
Management of colorectal cancer patients after resection of liver metastases: can we offer a tailored treatment?
Clinical and Translational Oncology (2012)
-
C-reactive protein as a biomarker for urological cancers
Nature Reviews Urology (2011)
-
Prognostic significance of CD45RO+ memory T cells in renal cell carcinoma
British Journal of Cancer (2011)