Abstract
Activation of the endothelin A receptor (ETA) by endothelin-1 (ET-1) mediates events that regulate mitogenesis, apoptosis, angiogenesis and metastasis in tumours. Specific blockade of ETA may have anticancer effects, while retaining beneficial endothelin B receptor (ETB)-mediated effects such as apoptosis and clearance of ET-1. ZD4054 is an orally active, specific ETA antagonist in clinical development. In receptor-binding studies, ZD4054 specifically bound to ETA with high affinity; no binding was detected at ETB. In a randomised placebo-controlled trial in eight healthy volunteers, a single oral dose of ZD4054 reduced forearm vasoconstriction in response to brachial artery infusion of ET-1, thus providing clinical evidence of ETA blockade. ETB blockade was assessed in an ascending, single-dose, placebo-controlled trial in 28 volunteers. For all doses of ZD4054, mean plasma ET-1 concentrations measured at 4 and 24 h were within the placebo reference range (a rise in ET-1 would indicate ETB blockade) and there was no evidence of dose-related changes. These data confirm the specificity of ZD4054 for ETA, with no activity at ETB in a clinical or preclinical setting. As a result of this specificity, ZD4054 has the potential to block multiple ETA-induced pathological processes, while allowing beneficial ETB-mediated processes to continue, which may, in turn, lead to an effective cancer therapy.
Similar content being viewed by others
Main
There is accumulating evidence to suggest that endothelins, particularly endothelin-1 (ET-1), have a role in regulating the growth and proliferation of tumours (Nelson et al, 2003). ET-1, produced by tumour cells, exerts its effects primarily by binding to G-protein-coupled receptors on the cell surface (endothelin A receptor (ETA) and B receptor (ETB)) (Nelson et al, 2003) and modifying the effects of other growth factors (Nelson et al, 1995).
Binding of ET-1 to ETA and ETB causes distinct and opposing effects on cell growth and survival. In most cells, activation of ETA promotes cell growth (Nelson et al, 2003), whereas activation of ETB induces cell death via apoptosis (Okazawa et al, 1998). In addition, binding of ET-1 to ETB results in clearance of ET-1 from the circulation. Overexpression of ETA has been reported in a variety of human tumours and human cancer cell lines, including the prostate, ovary, lung, colon, kidney, cervix and bone (Nelson et al, 2003). Conversely, ETB expression is reduced in the majority of solid tumours, but is still evident (Nelson et al, 2003). The balance of ETA and ETB activation in tumour cells appears to be important in progression of most cancers (Nelson et al, 2003), especially prostate cancer (Kopetz et al, 2002). Increased expression of ETA relative to ETB could contribute to increased tumour cell survival and growth.
Activation of ETA by ET-1 is reported to result in a number of events involved in the malignant process, including regulating mitogenesis, apoptosis, angiogenesis and tumour metastasis. It triggers a signalling cascade involving growth factors such as epidermal growth factor and insulin-like growth factor-1 (Pirtskhalaishvili and Nelson, 2000), kinases including protein kinase C and mitogen-activated protein kinase (Bagnato et al, 1997; Bagnato and Catt, 1998), and induction of immediate-early response genes (c-fos, c-jun and c-myc) that promote cell growth and mitogenesis (Battistini et al, 1993). Additionally, apoptosis induced by cytotoxic agents is inhibited (Del Bufalo et al, 2002) and angiogenesis promoted (via a vascular endothelial growth factor (VEGF)-mediated mechanism) by activation of ETA (Spinella et al, 2002; Bagnato and Spinella, 2003). The role of ETA in mediating increased proliferation, resistance to apoptosis and survival of tumour cells, and increased angiogenesis – a process central to tumour growth – makes ETA an attractive target for cancer therapy.
In addition to a role in growth and survival of primary tumours, ETA is an attractive target to prevent the spread and survival of tumour metastases. Activation of ETA induces the expression and activation of tumour proteases (matrix metalloproteinases and urokinase plasminogen activator) that facilitate tumour spread and metastasis (Rosanò et al, 2001). Furthermore, activation of ETA leads to proliferation of osteoblasts, bone remodelling and release of growth factors that stimulate survival and growth of metastatic tumour cells (Nelson et al, 1999) within prostate cancer metastases in bone. These findings have led to extensive research into the endothelin receptors as a target for anticancer therapies.
Specific blockade of ETA may offer an effective cancer therapy, since the anticancer effects of endothelin antagonists appear to be mediated via ETA blockade. In contrast, antagonism of ETB may lead to undesirable effects, such as inhibition of apoptosis and reduced clearance of ET-1. Thus, an agent with activity purely at the ETA (i.e. a specific ETA antagonist) would be desirable in an oncology setting. Atrasentan (Abbott Laboratories) is a selective ETA antagonist currently in development which, while selectively binding to ETA, also exhibits antagonism of ETB (Nelson, 2003), leading to increased plasma ET-1 levels (Carducci et al, 2002; Nelson, 2003). These findings are consistent with the binding affinities reported for atrasentan (0.034 and 63.3 nM for ETA and ETB, respectively). ZD4054 (AstraZeneca) is an orally active ETA antagonist in early clinical development for the treatment of cancer, which has recently been granted fast-track status by the FDA. The synthesis and molecular characterisation of ZD4054, a nonpeptide ETA antagonist, has been described previously (Bradbury et al, 1997). ZD4054 binds to ETA with high affinity and has no detectable affinity for ETB. In preclinical studies, ZD4054 specifically inhibits ETA-mediated antiapoptotic effects, but not ETB-mediated proapoptotic effects in human smooth muscle cells (Curtis et al, 2004; Dreicer et al, 2005), blocks ETA-mediated activation of p44/42 mitogen-activated protein kinase in murine osteoblast cells and inhibits ET-1 induced proliferation of human immature pre-osteoblast cells (Curtis et al, 2005). Importantly, ZD4054 inhibits growth of tumour xenografts in mice and enhances the cytotoxicity of paclitaxel in ovarian carcinoma in vitro and in vivo (Rosanò et al, 2005). This paper reports the results of studies that were conducted to confirm the specificity of ZD4054 for ETA in a clinical setting.
Materials and methods
Receptor-binding assays
The inhibition by ZD4054 (varying concentrations) of 125iodine-ET-1 binding to cloned human ETA and ETB was assessed using standard radioligand-binding techniques. Human recombinant ETA or ETB was expressed in mouse erythroleukaemic cells, and cell membranes prepared for competitive binding studies using 125iodine-ET-1 as the radioligand. Incubations were carried out in triplicate in the presence of ZD4054, 100 pM to 100 μ M in half-log increments, and inhibition of ET-1 binding was expressed as the geometric mean pIC50 value (concentration to inhibit 50% of binding) with a 95% confidence interval (CI). The affinity of ZD4054 for cloned human ETA was also assessed – using the equation of Cheng and Prusoff (1973) to determine the equilibrium dissociation constant (Ki)– in a further receptor-binding screen utilising a greater number of concentration–response curves determined in three separate studies.
Healthy volunteer study of forearm vasoconstriction to assess interaction with ETA
ET-1 causes vasoconstriction predominantly by activation of ETA on vascular smooth muscle (Spratt et al, 2001). Therefore, inhibition of ET-1-induced vasoconstriction, measured by venous occlusion plethysmography (Wilkinson and Webb, 2001), would provide clinical evidence of ETA blockade.
A single-dose, double-blind, placebo-controlled randomised trial was undertaken in eight healthy adult male volunteers to study the effect of ZD4054 on ET-1-mediated forearm vasoconstriction. All volunteers had previously demonstrated a mean 25–75% reduction in forearm blood flow (measured using standard strain gauge venous occlusion plethysmography) in response to a 120-min brachial artery infusion of ET-1. The effects of two oral doses of ZD4054 (10 and 30 mg) on ET-1-induced vasoconstriction were compared with placebo. Over nonconsecutive days, each volunteer received both doses of ZD4054 and placebo. The study was limited to two active doses and placebo due to the invasive nature and high technical difficulty of the brachial artery infusions and forearm vasoconstriction assessment. A 120-min brachial artery infusion of ET-1 (2.5 pmol min−1) was given to resting subjects, commencing 2 h after dosing with ZD4054 or placebo. The degree of forearm vasoconstriction measured between 90 and 120 min of the infusion (at 10-min intervals over a 30-min period) was compared between dose groups. The summary measure for statistical analyses was the percentage change in forearm blood flow. This measure was derived from the change from baseline (immediately prior to ET-1 infusion) in the mean area under the effect curve (forearm blood flow response) from 90 to 120 min (AUEC90−120) relative to the noninfused arm for each volunteer at each dose level vs placebo. Previous studies have shown that AUEC90−120 represents the most sensitive measure of ETA antagonism as ET-1-induced vasoconstriction is usually maximal after 90 min (Strachan et al, 2002). Treatment and dose effects were compared using analysis of variance (ANOVA), fitting effects for subject and dose level.
Healthy volunteer study of plasma ET-1 levels to assess interaction with ETB
A randomised, ascending, single-dose, double-blind, placebo-controlled study was undertaken in 28 healthy adult male volunteers. Oral doses of ZD4054 evaluated were 2.5, 10, 20, 30, 60, 120, 150 and 240 mg, with dose escalation continued based on tolerability until the maximum tolerated dose had been defined. The planned dose escalation sequence was from 120 to 240 mg ZD4054. However, the 240 mg dose was not tolerated; so the dose of 150 mg ZD4054 was investigated to further define the maximum tolerated dose. Volunteers were randomised approximately 3 : 1 to ZD4054 or placebo on each study day. Each cohort of volunteers was dosed consecutively on three separate study days, with a minimum of 14 days between doses in the same group. Doses of ZD4054 given were: group 1 (n=9) 2.5, 60 and 150 mg; group 2 (n=9) 10, 20 and 120 mg; group 3 (n=10) 30 and 240 mg. Blood samples were collected for measurement of plasma ET-1 (and its precursor, Big-ET-1), at baseline and at 4 and 24 h post-dose. An increase in ET-1 was taken as evidence of ETB blockade. ET-1 and big ET were extracted from plasma using an acetic acid extraction technique described by Rolinski et al (1994). Concentrations of ET-1 and big ET-1 in the extract were determined by radioimmunoassay using a methodology based on commercially available assay kits (Peninsula Laboratories Inc., San Carlos, CA, USA). Briefly, 100 μl of standard, sample or control was incubated with the appropriate antibody overnight. Samples were incubated with a known concentration of radio-labelled ET-1 or big ET-1 for a further 16 h and the immune complexes were precipitated with Amerlex™ (Amersham Plc, Amersham, UK) donkey anti-rabbit antibody. The sensitivities of the assays, defined as two standard deviations above the zero binding, were 0.25 pg ml−1 for ET-1 and 1 pg ml−1 for big ET-1.
Both clinical studies were approved by an Independent Ethics Committee and all subjects gave written informed consent. The study was performed in accordance with ethical principles originating in the Declaration of Helsinki and consistent with ICH/Good Clinical Practice, applicable regulatory requirements and AstraZeneca's policy on bioethics.
Results
Receptor-binding assays
ZD4054 potently inhibited the binding of 125iodine-ET-1 to cloned human ETA expressed in mouse erythroleukaemic cells, showing that ZD4054 has high affinity for ETA. The pIC50 for ZD4054 at the ETA (geometric mean) was 8.27 nM (95% CI: 8.23, 8.32 nM) (n=4). Displacement curves were normal, with slopes close to unity. In the multi-receptor binding screen, pIC50 values for ZD4054 at ETA were 22, 27 and 13 nM (mean value 21 nM) (Table 1). The Ki values measured in the same studies were 13, 17 and 8 nM (mean value 13 nM).
In contrast, ZD4054 had no measurable affinity for cloned human ETB, with a mean displacement of only 1.2±0.7% (n=3) of 125iodine-ET-1 at a concentration of 100 μ M ZD4054. This level of displacement is within the background range and is likely to be caused by assay variability. In the multi-receptor-binding screen, ZD4054 was inactive at ETB at a concentration of 10 μ M (Table 1).
These data show that ZD4054 is a high-affinity ligand for ETA, with no measurable affinity for ETB.
Healthy volunteer study of forearm vasoconstriction to assess interaction with ETA
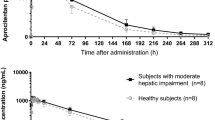
In volunteers given placebo, forearm blood flow was reduced by approximately 40% in response to brachial artery infusion of ET-1. ZD4054 inhibited this response to ET-1 (Figure 1A). The mean AUEC(90−120 min) corresponding to the forearm blood flow for each dose and placebo is shown in Table 2 and the AUEC(90−120 min) for individual patients at each dose level is shown in Figure 1B to illustrate the variability between individual volunteers. Administration of ZD4054 (10 or 30 mg; combined data) produced a statistically significant absolute reduction in vasoconstriction of 18.8% (P=0.021) when compared to placebo. Pairwise comparison showed that administration of ZD4054 (30 mg) produced a statistically significant absolute reduction in vasoconstriction of 23.7% (P=0.0125), representing a 63% decrease in vasoconstriction relative to placebo. ZD4054 (10 mg) resulted in a numerical decrease in vasoconstriction compared with placebo, which did not reach statistical significance (P=0.10). Peak plasma concentrations were reached by 1.75 and 2.5 h post-dosing and the mean plasma half-life of ZD4054 was 9.10 and 9.65 h for the 10 and 30 mg doses, respectively.
These results provide evidence that ZD4054 is an ETA antagonist in healthy volunteers.
Healthy volunteer study of plasma ET-1 levels to assess interaction with ETB
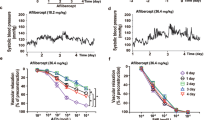
Following administration of ZD4054 (2.5–240 mg), mean values for plasma ET-1 were within the placebo range at both 4 and 24 h post-dose (Figures 2A and B). The placebo range was defined by the 2.5 and 97.5% percentiles of the pre-dose and placebo (drug naïve) samples. Within this study, ZD4054 was well-tolerated at single doses up to and including 120 mg; dose escalation was limited by headache, nausea and vomiting. Based on a rise in mean ET-1 values (Figures 2A and B) or percentage change from baseline (data not shown), there was no evidence of a dose-related response across the 2.5–240 mg (twice the maximum well-tolerated dose) dose range tested. Since peak plasma concentrations of ZD4054 were reached by approximately 2 h post-dose, any impact on ET-1 clearance and plasma concentration of ET-1 can be expected to be detectable at 4 h post-dose. However, no consistent profile was observed when comparing the 4- and 24-h time points at each dose (Figures 2A or B). Similarly, there was no evidence of an increase in levels of Big ET-1, the precursor for ET-1 (data not shown).
These data, showing the inability of ZD4054 to alter plasma concentrations of ET-1 (a biomarker of ETB blockade in vivo (Strachan et al, 1999)) in healthy volunteers, demonstrate the specificity of ZD4054 for ETA in a clinical setting.
Discussion
Studies have shown that activation of ETA by ET-1 results in a number of events that promote cell growth and mitogenesis (Battistini et al, 1993; Bagnato et al, 1997; Bagnato and Catt, 1998; Pirtskhalaishvili and Nelson, 2000), inhibit apoptosis induced by cytotoxic agents (Del Bufalo et al, 2002) and facilitate angiogenesis (Spinella et al, 2002; Bagnato and Spinella, 2003). Activation of ETA by ET-1 also induces tumour proteases that facilitate tumour metastasis (Rosanò et al, 2001), and causes proliferation of osteoblasts, bone remodelling and release of growth factors that stimulate survival and growth of metastatic tumour cells (Nelson et al, 1999). As a result, ETA is an attractive target for cancer therapy. Specific blockade of ETA has the potential to mediate anticancer effects, while allowing beneficial effects such as apoptosis and clearance of ET-1 that are mediated by ETB to proceed.
Results of the in vitro binding studies presented here show ZD4054 to be a potent and specific ETA antagonist, exhibiting high-affinity binding to ETA, with no measurable affinity for ETB at a concentration of 10 μ M. These results are consistent with previously reported molecular characterisation (Bradbury et al, 1997), and the results of functional assays showing that ZD4054 specifically inhibited ETA-mediated antiapoptotic effects, but not ETB-mediated proapoptotic effects, in human and rat smooth muscle cells (Curtis et al, 2004; Dreicer et al, 2005).
The experimental forearm vasoconstriction model is currently accepted as a standard technique for the investigation of vascular pharmacology and the impact of intra-arterial drug infusion in man (Wilkinson and Webb, 2001). Results using this model show ZD4054 to be a pharmacologically active ETA antagonist, acting in a dose-related manner to reduce ET-1-induced vasoconstriction. This vasoconstriction is mediated primarily by ET-1 selective, vascular smooth muscle ETA (Spratt et al, 2001). Although these results clearly demonstrate ETA antagonism in vivo, they do not give any information regarding the affinity of ZD4054 for ETB. Thus, a further volunteer study was undertaken to explore the specificity of ZD4054 for ETA.
In healthy volunteers, the concentration of circulating ET-1 has been established as a biomarker of ETB blockade in vivo (Strachan et al, 1999). In this setting, a rise in plasma ET-1, particularly without an accompanying rise in Big ET-1, indicates ETB inhibition. In the healthy volunteer study reported here, no evidence of ZD4054-induced ETB inhibition was detected; mean plasma levels of ET-1, at all doses of ZD4054, were within the placebo range at 4 and 24 h post-dose. No clinically significant rise in plasma ET-1 was observed when ZD4054 was given at doses up to 240 mg (twice the maximum tolerated dose). Furthermore, there was no evidence of a dose-related response based on a rise in mean ET-1 or percentage change from baseline. These data provide evidence that single doses of the ETA antagonist ZD4054 do not inhibit clearance of ET-1, and therefore that ZD4054 does not inhibit ETB in man. Through its specificity for ETA, ZD4054 may offer advantages over other less specific ETA antagonists in the oncology setting. Any degree of binding to ETB has the potential to reduce the efficacy of ETA blockade strategies, both directly through inhibition of ETB-mediated apoptosis and indirectly by reduction of ET-1 clearance, leading to a rise in levels of the ETA ligand, ET-1. Treatment with the selective ETA antagonist atrasentan (10 mg once daily for 28 days) resulted in a significant increase in plasma ET-1 levels in a study of patients with refractory adenocarcinomas (Carducci et al, 2002). Plasma levels of ET-1 rose linearly with increasing dose of atrasentan (dose range evaluated, 10–75 mg). This increase in plasma levels of ET-1 suggests reduced clearance of ET-1, an effect that could impair the efficacy of any ETA-blocking strategy. The authors hypothesised that the rise in plasma ET-1 reported with atrasentan was the result of direct ETA blockade (Carducci et al, 2002). Although it is difficult to extrapolate between patients and healthy volunteers, evidence from the present study shows that blockade of ETA by ZD4054, which has no detectable affinity for ETB (at a concentration of 10 μ M), does not result in elevated plasma levels of ET-1. Furthermore, the ability of atrasentan to increase plasma levels of ET-1 has been attributed to blockade of ETB (Nelson, 2003) and suggests that the system is highly sensitive to ETB blockade. To our knowledge, ZD4054 is the only endothelin receptor antagonist in clinical development that targets ETA and does not inhibit ETB at doses under clinical investigation.
In conclusion, volunteer studies and pre-clinical receptor-binding studies confirm that ZD4054 is a potent antagonist of ETA, with no evidence of ETB blockade at doses upto 240 mg in volunteers and at 10 μ M in vitro. This lack of affinity for ETB suggests that ZD4054 has the potential to block the multiple pathological processes in malignancy that are mediated by ETA, while allowing the beneficial processes mediated by ETB, such as apoptosis and clearance of ET-1, to proceed. Further studies to assess the clinical impact of specific ETA inhibition by ZD4054 in patients with cancer are ongoing.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Bagnato A, Catt KJ (1998) Endothelins as autocrine regulators of tumor cell growth. Trends Endocrinol Metab 9: 378–383
Bagnato A, Spinella F (2003) Emerging role of endothelin-1 in tumor angiogenesis. Trends Endocrinol Metab 14: 44–50
Bagnato A, Tecce R, Di Castro V, Catt KJ (1997) Activation of mitogenic signaling by endothelin 1 in ovarian carcinoma cells. Cancer Res 57: 1306–1311
Battistini B, Chailler P, D’Orleans-Juste P, Briere N, Sirois P (1993) Growth regulatory properties of endothelins. Peptides 14: 385–399
Bradbury RH, Bath C, Butlin RJ, Dennis M, Heys C, Hunt SJ, James R, Mortlock AA, Summer NF, Tang EK, Telford B, Whiting E, Wilson C (1997) New non-peptide endothelin-A receptor antagonists: synthesis, biological properties, and structure–activity relationships of 5-(dimethylamino)-N-pyridyl-, -N-pyrimidinyl, -N-pyridazinyl-, and -N-pyrazinyl-1-naphthalenesulfonamides. J Med Chem 40: 996–1004
Carducci MA, Nelson JB, Bowling MK, Rogers T, Eisenberger MA, Sinibaldi V, Donehower R, Leahy TL, Carr RA, Isaacson JD, Janus TJ, Andre A, Hosmane BS, Padley RJ (2002) Atrasentan, an endothelin-receptor antagonist for refractory adenocarcinomas: safety and pharmacokinetics. J Clin Oncol 20: 2171–2180
Cheng Y, Prusoff WH (1973) Relationship between the inhibition constant (Ki) and the concentration of inhibitor which causes 50 percent inhibition (IC50) of an enzymatic reaction. Biochem Pharmacol 22: 3099–3108
Curtis N, Anderson E, Brooks N, Curwen J (2005) ZD4054 blocks ET-1-stimulated phosphorylation of p44/42 mitogen-activated protein kinase and proliferation of osteoblast cells. Proc Am Assoc Cancer Res 46: 354 (abstract 1512)
Curtis N, Howard Z, Brooks N, Curwen J (2004) ZD4054 specifically inhibits endothelin A receptor-mediated anti-apoptotic effects, but not endothelin B receptor-mediated pro-apoptotic effects. Eur J Cancer Suppl 2: 27 (abstract 78)
Del Bufalo D, Di Castro V, Biroccio A, Varmi M, Salani D, Rosanò L, Trisciuoglio D, Spinella F, Bagnato A (2002) Endothelin-1 protects ovarian carcinoma cells against paclitaxel-induced apoptosis: requirement for Akt activation. Mol Pharmacol 61: 524–532
Dreicer R, Curtis N, Morris C, Wilson D, Hughes A, Le Maulf F, Howard Z, Brooks N, Curwen J (2005) ZD4054 specifically inhibits endothelin A receptor-mediated effects but not endothelin B receptor-mediated effects. Proc ASCO Multidisciplinary Prostate Cancer Sympos 153: 153 (abstract 237)
Kopetz ES, Nelson JB, Carducci MA (2002) Endothelin-1 as a target for therapeutic intervention in prostate cancer. Invest New Drugs 20: 173–182
Nelson JB (2003) Endothelin inhibition: novel therapy for prostate cancer. J Urol 170: S65–S68
Nelson J, Bagnato A, Battistini B, Nisen P (2003) The endothelin axis: emerging role in cancer. Nat Rev Cancer 3: 110–116
Nelson JB, Hedican SP, George DJ, Reddi AH, Piantadosi S, Eisenberger MA, Simons JW (1995) Identification of endothelin-1 in the pathophysiology of metastatic adenocarcinoma of the prostate. Nat Med 1: 944–949
Nelson JB, Nguyen SH, Wu-Wong JR, Opgenorth TJ, Dixon DB, Chung LW, Inoue N (1999) New bone formation in an osteoblastic tumor model is increased by endothelin-1 overexpression and decreased by endothelin A receptor blockade. Urology 53: 1063–1069
Okazawa M, Shiraki T, Ninomiya H, Kobayashi S, Masaki T (1998) Endothelin-induced apoptosis of A375 human melanoma cells. J Biol Chem 273: 12584–12592
Pirtskhalaishvili G, Nelson JB (2000) Endothelium-derived factors as paracrine mediators of prostate cancer progression. Prostate 44: 77–87
Rolinski B, Geier SA, Sadri I, Klauss V, Bogner JR, Ehrenreich H, Goebel FD (1994) Endothelin-1 immunoreactivity in plasma is elevated in HIV-1 infected patients with retinal microangiopathic syndrome. Clin Investig 72: 288–293
Rosanò L, Di Castro V, Spinella F, Natali PG, Bagnato A (2005) ZD4054, a specific antagonist of the endothelin A receptor, inhibits tumor growth and enhances cytotoxicity of paclitaxel in human ovarian carcinoma in vitro and in vivo. Proc Am Assoc Cancer Res 46: 1372 (abstract 5830)
Rosanò L, Varmi M, Salani D, Di Castro V, Spinella F, Natali PG, Bagnato A (2001) Endothelin-1 induces tumor proteinase activation and invasiveness of ovarian carcinoma cells. Cancer Res 61: 8340–8346
Spinella F, Rosano L, Di Castro V, Natali PG, Bagnato A (2002) Endothelin-1 induces vascular endothelial growth factor by increasing hypoxia-inducible factor-1alpha in ovarian carcinoma cells. J Biol Chem 277: 27850–27855
Spratt JC, Goddard J, Patel N, Strachan FE, Rankin AJ, Webb DJ (2001) Systemic ETA receptor antagonism with BQ-123 blocks ET-1 induced forearm vasoconstriction and decreases peripheral vascular resistance in healthy men. Br J Pharmacol 134: 648–654
Strachan FE, Newby DE, Sciberras DG, McCrea JB, Goldberg MR, Webb DJ (2002) Repeatability of local forearm vasoconstriction to endothelin-1 measured by venous occlusion plethysmography. Br J Clin Pharmacol 54: 386–394
Strachan FE, Spratt JC, Wilkinson IB, Johnston NR, Gray GA, Webb DJ (1999) Systemic blockade of the endothelin-B receptor increases peripheral vascular resistance in healthy men. Hypertension 33: 581–585
Wilkinson IB, Webb DJ (2001) Venous occlusion plethysmography in cardiovascular research: methodology and clinical applications. Br J Clin Pharmacol 52: 631–646
Acknowledgements
We thank Susan Hasmall for valued editorial assistance with financial support from AstraZeneca.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Morris, C., Rose, A., Curwen, J. et al. Specific inhibition of the endothelin A receptor with ZD4054: clinical and pre-clinical evidence. Br J Cancer 92, 2148–2152 (2005). https://doi.org/10.1038/sj.bjc.6602676
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6602676
Keywords
This article is cited by
-
Zibotentan in systemic sclerosis-associated chronic kidney disease: a phase II randomised placebo-controlled trial
Arthritis Research & Therapy (2022)
-
Endothelins in cardiovascular biology and therapeutics
Nature Reviews Cardiology (2019)
-
Cerebrovascular disease in ageing and Alzheimer’s disease
Acta Neuropathologica (2016)
-
Endothelin 1 in cancer: biological implications and therapeutic opportunities
Nature Reviews Cancer (2013)
-
Single- and multiple-dose pharmacokinetics, safety and tolerability of zibotentan (ZD4054) in Chinese men with advanced solid tumors
Cancer Chemotherapy and Pharmacology (2012)