Abstract
The 5-year relative survival rates of women diagnosed with breast cancer between 1992 and 1994 were compared among the 99 Health Authorities (1999 boundaries) of England. Substantial variation, with evidence of geographical clustering was observed. Part of this variation was explained by differences in deprivation between Health Authorities, in particular by the percentage of class IV and V households.
Similar content being viewed by others
Main
The chances of surviving a given cancer are not the same for all patients in all regions of England (Yuen et al, 1997; Coleman et al, 1999). Regional differences in survival within the UK have also been reported for several cancers (Silman and Evans, 1981; Chouillet, Bell and Hiscox, 1994; Macleod et al, 1998). In particular, there is evidence that, for most adult cancers, patients from affluent neighbourhoods have better survival than patients from deprived neighbourhoods. Such differentials are most unlikely to be attributable to chance (Kogevinas, 1990; Kogevinas et al, 1991; Schrijvers, 1996; Kidd, 1997; Pollock and Vickers, 1997) or to the extent of disease at the time of diagnosis (Carnon et al, 1994; Schrijvers et al, 1995a, 1995b). For breast cancer patients, these differentials have been associated with variations in diagnostic investigations both in England and Wales and in Scotland, and with departures from treatment guidelines (Gillis and Hole, 1996; Richards et al, 1996; Twelves et al, 1998; Stockton, 2002). Using detailed geographical survival data on breast cancer patients diagnosed in England in 1992–1994, we have compared survival patterns across regions and investigated their variation using demographic and socioeconomic indicators.
Participants and methods
Participants
Incidence data for breast cancer in 1992–1994, submitted to the Office for National Statistics by the nine regional cancer registries in England, were linked to death and emigration data by the National Health Service Central Register (NHSCR). Data were frozen in October 2000, when follow-up was considered acceptable up to 31 December 1999 (Coleman et al, 2000). A total of 93 687 records were included in the analysis. Some (5368) records were declared ineligible as the tumour was either in situ, benign or metastatic, or data were incomplete. Of the 88 319 eligible records, 11% were later excluded from the analysis, mainly for one of three reasons: survival time could not be calculated because only the date of death was known (death certificate only, 5341), a previous primary malignancy (1860), or synchronous tumours (872), or for lack of reliable information from NHSCR about vital status when the data were frozen (812). Details of these and other criteria, which accounted for the remaining 530 exclusions, have been published (Coleman et al, 1999). After exclusions, a total of 78 904 breast cancer patients, with age at diagnosis ranging from 16 to 99 years, were available for analysis.
Statistical analysis
The 5-year relative survival rates were computed separately for each of the 99 Health Authorities (HAs) in England (1999 boundaries). We used the age- and sex-specific England and Wales life-tables for the 1990–1992 pericensal period and adapted a method to estimate relative survival rates (Esteve et al, 1990).
The relative survival rates were plotted using a Geographical Information Systems (GIS) map. To investigate their variation across the nine English regions, several potential covariates were considered, in line with other studies (Quinn and Allen, 1995; Schrijvers et al, 1995; Coleman et al, 1999). These were all defined at the HA level and referred to either summary statistics of patient characteristics (e.g. mean age at diagnosis for each HA) or to summary statistics of enumeration district (ED) characteristics derived from the 1991 Census (e.g. mean percentage of Asians for every HA). They are listed in Table 1.
In descriptive analyses, all variables were grouped into categories defined by the tertiles of their distribution, but in regression models they were left as continuous variables, centred on their means (by subtracting the mean value from each observation) to obtain interpretable baseline rates. Fixed and random effects linear regression models (as used in meta-analyses, Whitehead and Whitehead, 1991) were fitted to quantify the variation in HA-specific relative survival rates and to identify the strongest HA-level covariates. Robust estimates of precision were used with fixed effects models in order to deal with the likely geographical correlation among the individual HAs. By contrast, random effects models directly specify such correlations leading to estimates of between-HA variances (τ2). These are measures of the heterogeneity among HAs that is unaccounted for by the covariates included in a model. Tests of significance and departure from linearity of continuous effects were performed via likelihood ratio tests (Clayton and Hills, 1993). Multivariable fixed effects models were compared using the strategy recommended by Collett (1994: pp 78–85), with P<0.10 as the inclusion criterion. The potential confounding effect of mean age at diagnosis was examined by forcing it into the final model.
Analyses were performed in Stata version 8 (StataCorp, 2003). Geographical Information Systems maps were produced in Arcview (Arcview GIS. v3.1; Environmental Systems Research Institute Inc.,).
Results
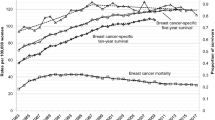
Of the 78 904 women included, 27 532 (35%) died within 5 years of diagnosis. The mean 5-year relative survival rate was 75%, with the HA-specific values ranging from 66 to 85%. There was evidence of some clustering among adjacent HAs, likely to be due to their sharing of a number of characteristics (Figure 1). Random effects meta-analysis without covariates provided evidence of a relatively large and significant between-HA variance (estimated τ2=8.47; P<0.001), thus supporting the visual impression of variability.
The distribution of 5-year relative survival rates by categories of the available covariates is shown in Table 1. There is evidence of geographical similarities among the Northern regions, with the relative survival rates in North West, Trent and Northern and Yorkshire being on average considerably lower than in London and in the Eastern and South East regions. Survival rates also decreased with greater mean age at diagnosis, while it increased with higher mean proportion of younger (aged 15–64 years) women living in the HA, the latter possibly being an indicator of greater affluence. There was some evidence that HAs with a greater mean percentage of Black Afro-Caribbean and Asians had higher relative survival rates. Health Authorities with higher mean proportions of heads of household in lower social classes, or higher mean unemployment rate, or higher deprivation indices showed strong negative trends in survival rates.
Univariable fixed effects regression analyses of these same factors, treated as continuous variables, revealed that the socioeconomic and geographical indicators were the strongest predictors of the 5-year survival rates (all P<0.01; Table 2). This is also shown by the largest reduction in estimated τ2 corresponding to the random effects models that included these variables. None of them showed evidence of departure from the null hypothesis of a linear effect (with the exception of HA mean percentage of black Afro-Caribbean; P=0.03). Multivariable fixed effects models revealed social class and region to be the most important factors (Table 3). The mean age at diagnosis did not confound or modify these effects. Repeating the analyses using random effects models confirmed these results and showed that the between-HA variation was more than halved from 8.47 (corresponding to the data of Figure 1) to 3.87. The intercept in the final random effects model (75.42%, 95% CI, 73.87, 76.96%) represents the estimated 5-year relative survival rate for women diagnosed in a London HA with average percentage (i.e. 17.9%) of class IV and V households. The estimated coefficient (−0.498, 95% CI −0.697, −0.298) instead represents the decrease in 5-year relative survival rates expected in any region for every percentage increase in HA mean percentage of class IV and V households. Similarly, the estimated coefficients for each region represent the increases (or decreases) in rates relative to the rate expected in a London HA, holding percentage of class IV and V households fixed.
Discussion
Our findings show that the significant variation in breast cancer survival between HAs in England can be partly explained by socioeconomic differentials between and within regions. Although the observation of an association between breast cancer survival and deprivation is well documented (Karjalainen, 1991; Schrijvers et al, 1995; Coleman et al, 1999), our findings add quantitative estimates of both accountable and residual variation between HAs.
Our results suffer from several limitations. Firstly, since the measures for deprivation were aggregated at HA level from smaller units (EDs), the results rely on the assumption that all the variables that determine survival rates are uniformly distributed within each HA. If this assumption were incorrect, the estimated effects would be biased, most probably towards the null hypothesis of no effect. This assumption of homogeneous deprivation level within each HA may be more appropriate when the geographical areas are small, but less so when the areas are as large as HAs. Secondly, population figures and socioeconomic indicators were taken from the 1991 decennial census, and therefore may not be accurate in portraying characteristics of the HA population throughout the years covered by this study (1992–1999). More up-to-date administrative data from official sources are becoming available at small-area level (e.g. income support recipients, Carstairs, 2000). Unfortunately, these were not available to us at the time of analysis.
The analyses were carried out at HA level, but HA areas cannot be considered as ‘units of performance’ in terms of breast cancer care. Thus, part of the unexplained geographical variation in survival rates may be due to differences in health care, such as the timing and extent of initial investigation, or type and departures from treatment guidelines (Quinn and Allen, 1995), or to individual level variables, such as the extent of disease at diagnosis (e.g. tumour grade and stage). These variables were not available to us. When more individual and HA-level data become available, our approach should be replicated to monitor improvements in the quality of detection and care of breast cancer patients and to inform local public health interventions.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Arcview GIS. v.3.1 (1998) Environmental Systems Research Institute Inc.
Carnon AG, Ssemwogerere A, Lamont DW, Hole DJ, Mallon E, George WD, Gillis CR (1994) Relation between socioeconomic deprivation and pathological prognostic factors in women with breast cancer. Br Med J 309: 1054–1057
Carstairs V (2000) Socio-economic factors at the area-level and their realtionship with health. In Spatial Epidemiology. Methods and Applications, Ellliot P, Wakefield JC, Best NG, Brigss DJ (eds). pp 51–67. Oxford: Oxford University Press
Chouillet AM, Bell CMJ, Hiscox JG (1994) Management of breast cancer in southeast England. Br Med J 308: 168–171
Clayton D, Hills M (1993) Statistical Models in Epidemiology. Oxford: Oxford University Press
Coleman MP, Babb P, Damiecki P, Grosclaude P, Honjo S, Jones J, Knerer G, Pitaro A, Quinn M, Sloggett A, De Stavola B (1999) Cancer Survival Trends in England and Wales 1971–1995. Deprivation and NHS Region. London: The Stationery Office
Coleman MP, De Stavola B, Romanengo M, Sloggett A, Quin M, Babb P (2000) Cancer survival in Health Authorities of England up to 1999. Patients diagnosed 1992–94 and followed up to 31 December 1999. Report for the National Centre for Health outcomes Development. London: London School of Hygiene and Tropical Medicine
Collett D (1994) Modelling Survival Data in Medical Research. London: Chapman & Hall
Esteve J, Benhamou E, Croasdale M, Raymond L (1990) Relative survival and the estimation of net survival: elements for further discussion. Statist Med 9: 529–538
Gillis CR, Hole DJ (1996) Survival outcome of care by specialist surgeons in breast cancer: a study of 3786 patients in the west of Scotland. Br Med J 312: 145–148
Karjalainen S (1991) Equity and cancer patient survival. Acta Universitatis Tamperensis, Ser A vol 316: 1–87
Kidd J (1997) Socioeconomic Variations in Breast Cancer Incidence, Survival and The Uptake of Screening: a Case Study in Merseyside (dissertation). Liverpool: University of Liverpool
Kogevinas M (1990) Longitudinal Study. Socio-Economic Differences in Cancer Survival. London: ONS
Kogevinas M, Marmot MG, Fox AJ, Goldblatt PO (1991) Socio-economic differences in cancer survival. J Epidemiol Commun Health 45: 216–219
Macleod U, Twelves CJ, Ross S, Gillis C, Watt G (1998) A comparison of the care received by women with breast cancer living in affluent and deprived areas. Br J Cancer 78(043 Suppl 2): 515
Pollock AM, Vickers N (1997) Breast, lung and colorectal cancer incidence and survival in South Thames Region, 1987–1992: the effect of social deprivation. J Public Health Med 19: 288–294
Quinn M, Allen E (1995) Changes in incidence of and mortality from breast cancer in England and Wales since the introduction of screening. Br Med J 311: 1391–1395
Richards MA, Wolfe C, Tilling K, Barton J, Bourne HM, Gregory WM (1996) Variations in the management and survival of women under 50 years with breast cancer in the South East Thames Region. Br J Cancer 19: 751–757
Schrijvers CTM (1996) Socioeconomic Inequalities in Cancer Survival in the Netherlands and Great Britain: Small-Area Based Studies Using Cancer Registry Data (dissertation). Rotterdam: Erasmus University
Schrijvers CTM, Mackenbach JP, Lutz JM, Quin M, Coleman MP (1995a) Deprivation, stage at diagnosis and cancer survival. Int J Cancer 63: 324–329
Schrijvers CTM, Mackenbach JP, Lutz JM, Quinn M, Coleman MP (1995b) Deprivation, stage at diagnosis and cancer survival. Br J Cancer 72: 738–743
Silman AJ, Evans SJ (1981) Regional differences in survival from cancer. Commun Med 3: 291–297
StataCorp (2003) Stata Statistical Software: Release 8.0. College Station. TX: Stata Corporation
Stockton D (2002) Cancer Survival in Scotland: Understanding Social Variations (dissertation). London and Southampton: London School of Hygiene and Tropical Medicine, University of Southampton
Twelves CJ, Thomson CS, Gould A, Dewar JA (1998) Variation in the survival of women with breast cancer in Scotland. Br J Cancer 78: 566–571
Whitehead A, Whitehead JA (1991) A general parametric approach to the meta-analysis of randomised clinical trials. Statist Med 10: 1665–1677
Yuen P, Haybittle J, Machin D (1997) Geographical variation in the standardised years of potential life lost ratio (SYPLR) in women dying from malignancies of the breast in England and Wales. Br J Cancer 75: 1069–1074
Acknowledgements
We are extremely grateful to Chris Frost and Professor Mike Kenward for their advice. Much appreciation is extended to Chris Grundy, for extracting and linking the population and socioeconomic data.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Mullee, M., De Stavola, B., Romanengo, M. et al. Geographical variation in breast cancer survival rates for women diagnosed in England between 1992 and 1994. Br J Cancer 90, 2153–2156 (2004). https://doi.org/10.1038/sj.bjc.6601812
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6601812
Keywords
This article is cited by
-
Geographic variation in health insurance benefits in Qianjiang District, China: a cross-sectional study
International Journal for Equity in Health (2018)
-
Investigation of low 5-year relative survival for breast cancer in a London cancer network
British Journal of Cancer (2010)
-
p53 mutation, deprivation and poor prognosis in primary breast cancer
British Journal of Cancer (2010)
-
Relationship Between Physician Supply and Breast Cancer Survival: A Geographic Approach
Journal of Community Health (2008)