Abstract
Design
This was a randomised controlled trial (RCT).
Intervention
Patients randomised to the treatment group received oral hygiene instruction, full-mouth scaling and root planing performed under local anaesthesia. The control group received no periodontal treatment during the study period, but after completion of the study these patients were given full nonsurgical and supportive periodontal treatment if needed.
Outcome measure
Plaque index (PI), gingival index (GI), probing pocket depth (PPD), gingival recession (GR), and bleeding on probing (BOP) were recorded . Venous blood samples were taken from each patient baseline and at the third month following the periodontal treatment; these were analysed for fasting plasma glucose (FPG), 2-h post-prandial glucose (PPG), glycated haemoglobin (HbA1c), total cholesterol (TC), triglyceride (TG), high-density and low-density lipoprotein cholesterol and microalbuminurea.
Results
A statistically significant effect could be demonstrated for PI, GI, PPD, CAL and BOP for the treatment group. HbA1c levels in the treatment group decreased significantly whereas the control group showed a slight but not statistically significant increase for this parameter.
Conclusions
The results of our study showed that nonsurgical periodontal treatment is associated with improved glycaemic control in type 2 diabetic patients and could be undertaken along with the standard measures for the diabetic patient care.
Similar content being viewed by others
Commentary
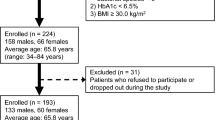
Although the periodontal consequences of diabetes mellitus are well-recognised, the possibility of a causal role for periodontal infection and inflammation on diabetic outcomes remains controversial.1,2 Much attention is therefore being given to testing the hypothesis that periodontitis is a modifiable risk factor for diabetes and to whether a periodontal intervention may result in improved diabetic outcomes. Whereas research on associations between oral and systemic diseases has previously focused on observational epidemiological studies, research in this area is increasingly becoming experimental and interventional. The work here of Kiran and colleagues, a small-scale (N=44), single-centre RCT presents evidence for the beneficial effect of periodontal scaling and root planing on the level of HbA1c in adult diabetics. At 3 months after the periodontal intervention, there was a significant reduction in %HbA1c in the treatment group compared with baseline (mean, 6.51% [95% confidence interval (CI), 6.17–6.85] at 3 months versus a mean of 7.31 [95% CI, 7.00–7.62 at baseline]). In contrast, in the untreated group, there was no improvement [mean, 7.31 (95% CI, 6.98–7.64) at 3 months versus a mean of 7.00 (95% CI, 6.70–7.30) at baseline]. This finding should be interpreted with caution, however, and viewed in the context of other extant evidence.
The recent meta-analysis of Janket et al.,3 in which 456 participants were pooled from 10 intervention studies, found that whereas periodontal treatment was associated with an average decrease in %HbA1c of 0.66% in type 2 diabetic patients (and a 0.71% decrease if antibiotics were given), such changes were not statistically significant.3 Moreover, the results of a recently completed RCT involving 193 adult diabetics found no significant benefits at 4 months following a periodontal intervention.4 Of note, the current article lacks certain essential methodological information that makes it difficult to adequately assess study quality and other characteristics. Unfortunately, such paucity of detail is seen too often in published reports of RCT. Needleman5 has earlier noted the importance of scholarly journals adhering to rigorous and uniform standards for reporting RCT if evidence-based dental practice is to progress.
References
Mealey BL, Oates TW . Diabetes mellitus and periodontal diseases. J Periodontol 2006; 77:1289–1303.
Taylor GW . Bidirectional interrelationships between diabetes and periodontal diseases: an epidemiologic perspective. Ann Periodontol 2001; 6:99–112.
Janket SJ, Wightman A, Baird AE, Van Dyke TE, Jones JA . Does periodontal treatment improve glycemic control in diabetic patients? A meta-analysis of intervention studies. J Dent Res 2005; 84:1154–1159.
Jones JA, Miller DR, Wehler CJ, et al. Does periodontal care improve glycemic control? Department of Veterans Affairs Dental Diabetes Study. J Clin Periodontol 2007; 34:46–52.
Needleman I . Is this good research? Look for CONSORT and QUORUM. Evid based Dent 2000; 2:61–62.
Author information
Authors and Affiliations
Additional information
Address for correspondence: Elif Unsal, Department of Periodontology, Faculty of Dentistry, Ankara University, 06500 Be^evler, Ankara, Turkey. E-mail: elifunsal@hotmail.com
Kiran M, Arpak N, Unsal E, Erdogan MF. The effect of improved periodontal health on metabolic control in type 2 diabetes mellitus. J Clin Periodontol 2005; 32:266–272
Rights and permissions
About this article
Cite this article
Garcia, R. Periodontal treatment associated with improved glycaemic control in type 2 diabetic patients. Evid Based Dent 8, 13 (2007). https://doi.org/10.1038/sj.ebd.6400465
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ebd.6400465