Abstract
Germ-line mutations in the BRCA1 gene cause hereditary predisposition to breast and ovarian cancer. BRCA1 and BRCA2 mutations account for about 40% of high-risk families. Mutation-screening methods generally focus on genomic DNA and are usually PCR based; they enable the detection of sequence alterations such as point mutations and small deletions and insertions. However, they do not allow the detection of partial or entire exon(s) loss, because the presence of the homologous allele results in a positive PCR signal, giving rise to a false-negative result. Identification of unusual haplotypes in patient samples by an expectation maximisation algorithm has recently been suggested as a method for identifying hemizygous regions caused by large intragenic deletions. Using a similar approach, we identified a novel BRCA1 genomic rearrangement in a breast/ovarian cancer family negative at the first mutation screening; we detected a deletion encompassing exons 14–19, probably due to replication slippage between Alu sequences.
Similar content being viewed by others
Main
Germ-line mutations in BRCA1 and BRCA2 genes cause hereditary predisposition to breast and ovarian cancer. BRCA1 and BRCA2 mutations account for about 40% of high-risk families.1 The predisposition to develop cancer is transmitted as an autosomal dominant trait. For such reason, it is very important to detect single-allele inactivation events caused by intragenic deletions leading to hemizygosity. Methods employed for mutation screening usually focus on genomic DNA and are PCR based (ie, direct sequencing, single-strand conformation polymorphism analysis, denaturing gradient gel electrophoresis or heteroduplex analysis). These approaches enable the detection of sequence alterations, such as point mutations, and small deletions and insertions. Depending on the breakpoint location, the loss of partial or entire exon(s) will not be detected by these methods because the presence of the homologous normal allele results in a positive PCR signal. This mechanism is considered as an important cause of false-negative results.2
It has been estimated that not more than the 70% of mutations are detected among the BRCA1-linked families screened by one or the other of the methods described above; this relative low sensitivity can be due to a substantial fraction of BRCA1 mutations occurring outside the coding region and splice sites and also to large deletions.3
The human genome contains up to 1 million copies of interspersed Alu elements (one Alu repeat every 5 kb) that are thought to mediate chromosomal rearrangements and homologous recombination events that result in translocations, duplications, inversions or deletions.4 Analysis of the genomic structure of the BRCA1 gene has revealed an high density of Alu repeats, with 41.5% of the genomic sequence being composed of Alu sequences or one Alu repeat every 0.65 kb.5 At present, 22 different large genomic rearrangements have been characterised, they include both deletions and duplications of one or more exons in BRCA1.6, 7, 8, 9, 10
Only two rearrangements of the BRCA2 gene have been detected to date: a 5 kb deletion leading to exon 3 skipping11 and a 6.2 kb deletion removing exons 12–13.12 Since the BRCA2 genomic sequence contains fewer Alu repeats than BRCA1, it is presumed that genomic rearrangements involving Alu-mediated recombination events are less frequent.
In the present work, the genomic DNAs from 47 individuals belonging to 47 families with a strong history of breast and/or ovarian cancer (33 HBC, one HOC and 13 HBOC) were analysed for point mutation of BRCA1 and BRCA2 genes by direct sequencing of all coding exons and intron–exon boundaries. Seven pathogenic mutations in BRCA1 and four in BRCA2 and several allelic variants were detected. In particular, seven SNPs of the BRCA1 gene were used to build the haplotypes of the entire sample: four were intronic (IVS8−58delT, IVS14−63C/G, IVS16−68A/G, IVS18+72G/A) and three were exonic (2731 C/T in exon 11; 4427 T/C in exon 13; 4956 A/G in exon 16) (Table 1). Three frequent multilocus genotypes were detected as follows: 18 subjects (38.3%) were homozygous for the consensus allele at all loci, 10 (21.3%) were homozygous for the variant allele at all loci and 17 (36.2%) were heterozygous at all loci. In addition, two subjects carried a unique genotype (Table 1); it thus appeared that these SNPs were in strong linkage disequilibrium, confirming previous reports.13, 14 This feature greatly facilitates the construction of haplotypes; in fact, inferring the haplotype composition of the entire sample was straightforward. Only two haplotypes exist at high frequency, the ‘A’ haplotype (‘1111111’) and the ‘B’ haplotype (‘2222222’), respectively, whereas two haplotypes are present once (‘2222221’ and ‘1112222’). We suspected that these unique haplotypes were spurious, being instead the consequence of loss of heterozygosity due to large intragenic deletions. Therefore, we carried out the molecular characterisation by RT-PCR using primer pairs located in the presumed deletion flanking regions of the only sample for which RNA was available. The tested sample showed evidence of rearrangement in BRCA1 gene: as a matter of fact two bands (1.5 kb band corresponding to the wild-type mRNA product and an additional 0.7 kb band of unknown meaning) were detected using a forward primer located in exon 11 and a reverse primer located in exon 24 (Figure 1a). Sequence analysis of a 0.7 kb fragment showed that this alteration encompasses exons 14–19. The same deletion was detected at mRNA level in mother's proband affected by ovarian cancer (data not showed).
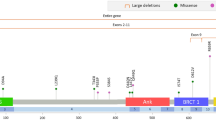
To confirm the novel rearrangement detected and to define the boundaries of the deletion, long-range PCR was performed on genomic DNA using primers located in intron 13 (5′-CCAGAACAAAGCACATCAGAAAAA-3′) and in intron 19/exon 20 (5′-ATGCTGAAAGAAACCAAACACAAC-3′). From the patient's DNA a 5 kb PCR product was observed, whereas the 25 kb expected product was not obtained (Figure 1b.). This 5 kb product was gel extracted and sequenced using various combination of PCR primers in introns 13 and 19 designed to identify the exact localisation of junction on BRCA1 gene. It turned out that a segment of 19 886 bp was deleted starting at nucleotide 51 482 in intron 13 and ending at nucleotide 71 368 in intron 19 (Accession number GenBank L78833). An Alu sequence is located near both positions (Alu Sq in intron 13 and Alu Sx in intron 19), making it likely that the deletion was the consequence of replication slippage (Figure 2).
We also considered whether the inactivation of the wild-type allele in the patient's breast tumour was due to somatic deletion. DNA was extracted from pure neoplastic cells obtained by laser capture microdissection (AS-LMD, Leica, Germany) of paraffin-embedded formalin-fixed tissues and exon 16 (which maps in the deleted region) was amplified. A PCR product compatible with the exon 16 length was obtained, indicating that the total inactivation of the BRCA1 gene was not due to allelic deletion (data not shown).
To date, methods able to identify large genomic rearrangements are Southern blot based and, more recently, QMPSF (quantitative multiplex PCR of short fluorescent fragments)9 and MLPA (multiplex ligation probe amplification) based.13 Identification of unusual haplotypes in patient samples by an expectation maximisation algorithm has recently been suggested as a method to identify hemizygous regions caused by intragenic deletions.14 In fact, the existence of only two major haplotypes segregating at high frequency (0.64 and 0.33, respectively) in the Caucasian population for the entire length of the BRCA1 gene15 makes this approach feasible by simple inspection of the multilocus genotypes at a small number of intragenic SNPs.16 We identified a novel BRCA1 deletion in a breast/ovarian cancer family using this approach, so it results that in our family collection, the 12% (1/8) of BRCA1 mutations may be due to large genomic rearrangements. In conclusion, examining the SNPs, which actually are a pitfall of the gene screening, could instead be useful for the identification of patients harbouring large intragenic deletions; this reading do not need any additional work. A drawback of the method is that it can work for heterozygous individuals only (44.7% in our series), meaning that about 50% of patients carrying large deletions can be diagnosed with this approach; in practice, however, the chance of missing a mutation is higher, because even in heterozygous only those deletions that encompass a polymorphic nucleotide can be detected. Therefore, other methodologies should be considered for detecting deletions in patients who are homozygous and also heterozygous for either haplotypes.
References
Wooster R, Weber B : Breast and ovarian cancer. N Engl J Med 2003; 348: 2339–2347.
Eng C, Brody LC, Wagner TM et al: Steering committee of the breast cancer information core (BIC) consortium. Interpreting epidemiological research: blinded comparison of methods used to estimate the prevalence of inherited mutations in BRCA1. J Med Genet 2001; 38: 824–833.
Ford D, Easton DF, Stratton M et al: Genetic heterogeneity and penetrance analysis of the BRCA1 and BRCA2 genes in breast cancer families. The breast cancer linkage consortium. Am J Hum Genet 1998; 62: 676–689.
Kolomietz E, Meyn MS, Pandita A, Squire JA : The role of Alu repeat clusters as mediators of recurrent chromosomal aberrations in tumors. Genes Chromosomes Cancer 2002; 35: 97–112.
Smith TM, Lee MK, Szabo CI et al: Complete genomic sequence and analysis of 117 kb of human DNA containing the gene BRCA1. Genome Res 1996; 6: 1029–1049.
Petrij-Bosch A, Peelen T, van Vliet M et al: BRCA1 genomic deletions are major founder mutations in Dutch breast cancer patients. Nat Genet 1997; 17: 341–345.
Puget N, Stoppa-Lyonnet D, Sinilnikova OM et al: Screening for germ-line rearrangements and regulatory mutations in BRCA1 led to the identification of four new deletions. Cancer Res 1999; 59: 455–461.
Unger MA, Nathanson KL, Calzone K et al: Screening for genomic rearrangements in families with breast and ovarian cancer identifies BRCA1 mutations previously missed by conformation-sensitive gel electrophoresis or sequencing. Am J Hum Genet 2000; 67: 841–850.
Casilli F, Di Rocco ZC, Gad S et al: Rapid detection of novel BRCA1 rearrangements in high-risk breast-ovarian cancer families using multiplex PCR of short fluorescent fragments. Hum Mutat 2002; 20: 218–226.
Montagna M, Palma MD, Menin C et al: Genomic rearrangements account for more than one-third of the BRCA1 mutations in northern Italian breast/ovarian cancer families. Hum Mol Genet 2003; 12: 1055–1061.
Nordling M, Karlsson P, Wahlstrom J, Engwall Y, Wallgren A, Martinsson T : A large deletion disrupts the exon 3 transcription activation domain of the BRCA2 gene in a breast/ovarian cancer family. Cancer Res 1998; 58: 1372–1375.
Wang T, Lerer I, Gueta Z et al: A deletion/insertion mutation in the BRCA2 gene in a breast cancer family: a possible role of the Alu-polyA tail in the evolution of the deletion. Genes Chromosomes Cancer 2001; 31: 91–95.
Hogervorst FB, Nederlof PM, Gille JJ et al: Large genomic deletions and duplications in the BRCA1 gene identified by a novel quantitative method. Cancer Res 2003; 63: 1449–1453.
Hendrickson BC, Pruss D, Lyon E, Scholl T : Application of haplotype pair analysis for the identification of hemizygous loci. J Med Genet 2003; 40: 346–347.
Liu X, Barker DF : Evidence for effective suppression of recombination in the chromosome 17q21 segment spanning RNU2-BRCA1. Am J Hum Genet 1999; 64: 1427–1439.
Osorio A, de la Hoya M, Rodriguez-Lopez R et al: Over-representation of two specific haplotypes among chromosomes harbouring BRCA1 mutations. Eur J Hum Genet 2003; 11: 489–492.
Acknowledgements
We thank the patients and their family members for cooperation. This work was supported by program grants from AIRC (Italian Association for Cancer Research) and MIUR (Italian Ministry for University and Scientific Research).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tancredi, M., Sensi, E., Cipollini, G. et al. Haplotype analysis of BRCA1 gene reveals a new gene rearrangement: characterization of a 19.9 KBP deletion. Eur J Hum Genet 12, 775–777 (2004). https://doi.org/10.1038/sj.ejhg.5201223
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejhg.5201223
Keywords
This article is cited by
-
Correlations between long inverted repeat (LIR) features, deletion size and distance from breakpoint in human gross gene deletions
Scientific Reports (2015)
-
Large genomic rearrangements of the BRCA1 and BRCA2 genes: review of the literature and report of a novel BRCA1 mutation
Breast Cancer Research and Treatment (2011)
-
Identification of rare complete BRCA1 gene deletion using a combination of SNP haplotype analysis, MLPA and array-CGH techniques
Breast Cancer Research and Treatment (2008)