Abstract
The male proband reported here was born with appropriate anthropometric parameters at term as the second child of healthy nonconsanguineous parents. His only clinical symptom was bilateral congenital cataracts with strabismus at birth, and both lenses were removed surgically at the age of 8 months. The perinatal and infantile period thereafter was clinically uneventful and his psychomotor development appeared almost normal. At the age of 6 years he was hospitalized for slight muscle weakness, minor ptosis, nystagmus and decreased physical activity. Soon after, his general condition worsened, gait ataxia presented, dysphagia and difficulty of speech followed by rapidly progressive generalized ataxia, and myopathy developed. Typical progressive gray matter degeneration with focal necrosis in the basal ganglia characteristic of the Leigh type of neuropathology could be detected by cranial MRI, the muscle histology showed ragged-red fibers. At the age of 7.5 years, unexpected left side hemiparesis with speech disability resembling that seen in MELAS syndrome developed, from which he recovered within 1.5 days. The mtDNA of the patient showed single 6.7 kb large-scale deletion harboring between 7817 and 14 536 bp. This case represents the first report of a verified mtDNA mutation associated with congenital cataracts as the first clinical sign of a later developing progressive neuromuscular disease presented with a combination of Leigh neuropathology, ragged-red fiber histopathology and stroke-like attack.
Similar content being viewed by others
Introduction
Congenital cataract can occur as an isolated abnormality or as an associated feature of several different disorders.1,2,3,4 The prevention of visual impairment because of congenital cataract appears as an international priority. Several trials have been initiated to determine the incidence of cataract in a population, especially in the industrialized countries, and efforts are in progress to determine the proportion of hereditary cataracts, delineate the mode of inheritance, and the clinical presentation.5,6,7,8,9
Albeit during the 14 years of mitochondrial medicine since 1988 more than 100 point mutations and several rearrangements of human mtDNA associated with a wide range of clinical phenotypes have been described,10,11,12,13 further gain of the spectrum of the phenotypes could be predicted.11 While new mutations are still being described on the clinical side of the mtDNA investigations, in the basic research Sligh et al14 have recently produced heteroplasmic mice with sufficiently high levels of the mtDNAs from a partially respiratory-deficient chloramphenicol-resistant (CAPR) cell line, and the chimeric mice developed a variety of ocular abnormalities, including congenital cataracts.
Here we report a patient who was born with bilateral congenital cataracts, and after an uneventful period the characteristic progressive hallmarks of mitochondrial disease developed at the age of 6 years. These included neuropathologic features of Leigh disease, ataxia, stroke-like hemiparesis, ophthalmoplegia and ptosis. Analysis of the mtDNA of the patient revealed a novel type of single 6.7 kb large-scale deletion harboring between 7817 and 14 536 bp location.
Materials and methods
Clinical report and routine laboratory findings
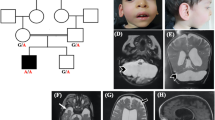
The male patient was the second child born (March 1991) at term with age-appropriate anthropometric parameters to healthy nonconsanguineous parents. Bilateral cataracts were discovered immediately after birth, for which both lenses were removed at the age of 8 months. Possible infectious (rubella, CMV, toxoplasma) and common metabolic origin (galactosemia, hypoparathyroidism) of cata-racts were excluded. Apart from that the perinatal and infantile period was uneventful and his psychomotor development was normal. His first symptoms, including slight muscle weakness and gait ataxia, were presented at the age of 6 years. He had complained about dysphagia and difficulty of speech followed by rapidly progressive generalized ataxia and myopathy thereafter. At the age of 7.5 years he had an episode of a transient hemiparesis from which he recovered almost completely within 1.5 days. At the age of 8 years, the patient had anthropometric parameters below the third centile, microcephaly, ptosis, progressive external ophthalmoplegia, head lag with generalized muscle weakness, decreased muscle mass, no detectable deep tendon reflexes and moderate response to painful stimuli. He was just able to move his arms, but had severe ataxia. He was no more able to sit up, swallow or talk, although he still tried to communicate by moving his eyelids as a response to verbal stimuli. Currently, he is 11 years old, rolling over for toys and fed by a nasogastric tube.
Cranial MRI detected the typical signs of Leigh disease in the basal ganglia with some cortical and significant ponto-cerebellar atrophy at the age of 7 years, and a slight progression was detected in the temporo-cortical degeneration at the age of 8 years. Eye examination, including the examination of the fundus, ophthalmoscopy, VEP and BERA were repeatedly normal. The patient never had clinical symptoms of cardiac involvement, and the ECG and cardiac ultrasound examinations were normal during the follow-up.
Fasting and fed serum lactate were found to be normal on repeated examinations during the 5 years of follow-up. The levels of serum ammonia, pyruvic acid, glucose, amino acids, carnitine levels and urine organic acids were normal. The patient never had anemia (red cell count and morphology, thrombocyte count, hemoglobin, hematocrit and parameters of iron homeostasis were repeatedly normal), and there was no evidence of pancreatic insufficiency. Laboratory studies detected a significantly increased protein level in the cerebrospinal fluid without specific alterations.
Analysis of a muscle biopsy specimen (superficial part of m. quadriceps) performed at the age of 7 years showed the histological hallmarks of ragged-red fibers, staining for cytochrome c oxidase gave a weak signal, and the succinate dehydrogenase staining reaction was normal.
As part of our routine, some known causes of Leigh phenotype (T8993C, T9176C, T9176G and C9537CC point mutations) were excluded in the patient.
Methods
Cytochrome c oxidase, NADH:cytochrome c oxidoreductase, lipoamide dehydrogenase and malate dehydrogenase activities were determined as described previously.15,16 For control pooled specimens (five for each enzyme) from patients of similar age who previously underwent diagnostic muscle biopsy but were declared finally free from primary muscle disease were used.
The search for an mtDNA deletion was begun with Southern blot analysis.16,17 Approximately 10 μg DNA aliquots were digested with several restriction enzymes, and after separation on 0.7% agarose gel the digests were transferred to a nitrocellulose membrane. Full-length mtDNA extracted from human placental mitochondria was [32P]-labeled with an Amersham Megaprime DNA labeling system and was used as the probe.16,17 The percentage of the deletion was quantified by densitometry analysis of the blots using an Advanced American Biotechnology (Fullerton, CA, USA) gel documentation and analysis system.
The exact sites of deletion breakpoints were located by serial conventional or long PCR amplifications.16 Finally, with the appropriate forward (5′-CTTATCTGCTTCC TAGTCCTGTATG-3′) and reverse (5′-CTGTTGAGTGTGGGTTTAGTAATGG-3′) primers, successful amplification could be performed. The reaction was carried out using 1 μl of DNA solution in a final volume of 50 μl, which included 200 μ M of each dNTP, 1 mM MgCl2, 2 U Taq DNA polymerase and PCR buffer (100 mM Tris-HCl, pH 9.0 containing 500 mM KCl, 15 mM MgCl2), and 0.2 μ M of each primer. A total of 30 cycles were run with an MJ Research PTC-200 thermal cycler; the cycling conditions were as follows: predenaturation 2 min at 95°C, denaturation 15 s at 95°C, annealing 10 s at 61°C and primer extension 30 s at 72°C, final extension 5 min at 72°C. The PCR product was sequenced by the fluorescent sequencing method with an automated ABI PRISM 310 Genetic Analyzer (Perkin-Elmer, USA).
Results
The activity of cytochrome c oxidase was dramatically decreased in the patient's muscle specimen (0. 35±0.06 vs 2.97±0.32 μmol/min/g wet weight) as compared with controls (n=6 for controls; results are expressed as means ±SEM of two separate determinations, and are μmol/min/g wet weight throughout). A profound decrease was also found in the activity of NADH:cytochrome c oxidoreductase (0.48±0.04 vs 2.41±0.31). The activity of lipoamide dehydrogenase decreased to approximately 55% of the control value (15.6±2.10 vs 28.4±3.11), while the activity of malate dehydrogenase was similar in the samples of the patient and the controls (156.0±14.0 vs 167.1±15.2 μmol/min/g wet weight).
Several restriction enzymes (including EcoRI, EcoRV, PvuII and XbaI) were tried for identification and probable localization of mtDNA deletion, and representative Southern blots are shown in Figure 1. Digestion with XbaI and PvuII enzymes gave the most informative patterns; for PvuII approximately 10 kb while for XbaI an extra 3 kb digestion fragment was detected, besides the normal digestion products. In DNA extracted from peripheral blood (Figure 1), the extra band corresponded approximately to 52% while in skeletal muscle (not shown) to 64% of the total mtDNA. In the peripheral blood DNA of both the parents and of the healthy older brother, the Southern blot assays gave normal patterns.
Representative Southern blots of blood mtDNA of patient (lanes 2 and 4) and controls (lanes 1 and 3). The DNA was digested with PvuII (lanes 1 and 2) and with XbaI (lanes 3 and 4). The extra bands are shown by bold arrows; approximately 3 kb for XbaI (lower arrow) and 10 kb (upper arrow) for PvuII. For control blood DNA from a healthy subject was used.
Direct sequencing of the PCR product harboring the mtDNA deletion revealed a 6718 bp size deletion between the 7817 and 14 536 end point nucleotide pairs (Figure 2).
Forward and reverse sequencing of the suspected region of mtDNA amplified by primers as described in the Materials and methods. A 6718 bp size deletion between the 7817 and 14 536 bp was detected in both directions, the termini of the deleted sequences (starting at 7818 and ending at 14 535 bp) are in italics.
Discussion
In our patient, the mutation affected nine protein coding regions (cytochrome c oxidase II and III subunits, ATP synthase 6 and 8, NADH dehydrogenase 3, 4, 4L, 5 and 6 subunits) and six tRNA genes (tRNA lysine, glycine, arginine, histidine, serine 2 and leucine 2) of the mtDNA. At least because of the localization, the probably different mitotic segregation of the mutated variants and in association with the tissue-specific degree of heteroplasmy, the phenotype and the clinical course in our patient differed from any known disease, even if the presenting symptoms alone or in combination have already been known in association with mitochondrial disease.
The unique feature of our case is the presence of the bilateral cataracts at birth. While the other symptoms of the complex neuromuscular disease developed later, no sign of an oxidative phosphorylation disease could be seen prior to the school age. Maturity onset cataract has already been presented in the literature in association with mitochondrial disease: retinitis pigmentosa, noncongenital cataracts and glaucoma have been reported in a patient with a disrupted anticodon loop of the tRNALeu(UUR),18 or in a patient with a multiple mtDNA deletions.19 In turn, congenital cataracts as elements of possible mitochondrial diseases have also been presented as clinical descriptions;20,21 however, the underlying mtDNA abnormalities have not been determined. This emphasizes the importance of delineating the precise nature of mutation responsible for patient diagnosis as well as for genetic counseling of maternal lineage relatives.
As a pioneering attempt in mtDNA research, recently Sligh et al14 have been able to transmit mtDNA mutations to succeeding generations and, even more notably, have produced heteroplasmic mice with sufficiently high levels of the CAPR mutation to express phenotypic abnormalities. The CAPR chimeras developed an ocular phenotype including congenital cataracts and functional retinopathy. The authors concluded that these are reminiscent of the defects seen in humans with mtDNA disease.14 It is currently unknown as to why the CAPR mutation or the mutation in our case induces cataract formation. The lens is a highly complex structure consisting of numerous types of crystalline proteins that form the lens sequentially during development.3 As has been suggested, it is possible that an energetic defect alters the development of the lens fibers during the fetal stage of lens development. The CAPR mutation could also result in increased mitochondrial production of reactive oxygen species during the intrauterine development of the early eye altering the lens crystalline proteins, as has been suggested for the formation of cataracts in the elderly.3
Several different types of gene-determined metabolic defects can lead to Leigh disease phenotype or Leigh type of neuropathology.22,23,24 The main pathological finding in the Leigh disease is the gray matter degeneration with foci of necrosis and capillary proliferation in the brain stem, which is generally accepted as a hallmark of the syndrome.23 With the accumulation of clinical and genetic data, several phenotypic variants and genetic subtypes of the disease have been identified.22 Since our case fulfils the radiopathological diagnostic criteria of the syndrome, this disease can also be regarded as a novel variant or subtype of the Leigh disease.
In turn, mtDNA deletion with Leigh-type neuropathology accompained by other mitochondrial features has already been presented in the literature.24 However, mtDNA deletions are more frequently associated with Pearson syndrome, progressive external ophthalmoplegia, and Kearns–Sayre syndrome10,11,25,26,27,28,29,30,31 than with Leigh-like manifestations. In contrast, in our case there was no evidence for the bone marrow–pancreas and cardiac involvement, which clearly differentiates our case from cases already presented.
References
Cassidy L, Taylor D : Congenital cataract and multisystem disorders. Eye 1999; 13 (Part 3b): 464–473.
Francis PJ, Berry V, Moore AT, Bhattacharya S : Lens biology: development and human cataractogenesis. Trends Genet 1999; 15: 191–196.
McAvoy JW, Chamberlain CG, de Iongh RU, Hales AM, Lovicu FJ : Lens development. Eye 1999; 13 (Part 3b): 425–437.
He W, Li S : Congenital cataracts: gene mapping. Hum Genet 2000; 106: 1–13.
Gilbert C, Foster A : Childhood blindness in the context of VISION 2020–the right to sight. Bull World Health Organ 2001; 79: 227–232.
Kocur I, Resnikoff S : Visual impairment and blindness in Europe and their prevention. Br J Ophthalmol 2002; 86: 716–722.
Rahi JS, Botting B : Ascertainment of children with congenital cataract through the National Congenital Anomaly System in England and Wales. Br J Ophthalmol 2001; 85: 1049–1051.
Wirth MG, Russell-Eggitt IM, Craig JE, Elder JE, Mackey DA : Aetiology of congenital and paediatric cataract in an Australian population. Br J Ophthalmol 2002; 86: 782–786.
Rahi JS, Dezateaux C : Measuring and interpreting the incidence of congenital ocular anomalies: lessons from a national study of congenital cataract in the UK. Invest Ophthalmol Vis Sci 2001; 42: 1444–1448.
DiMauro S : Mitochondrial DNA: a genetic Pandora's box. Funct Neurol 2001; 16: 103–116.
DiMauro S, Andreu AL : Mutations in mtDNA: are we scraping the bottom of the barrel? Brain Pathol 2000; 10: 431–441.
DiMauro S : Lessons from mitochondrial DNA mutations. Semin Cell Dev Biol 2001; 12: 397–405.
Zeviani M, Klopstock T : Mitochondrial disorders. Curr Opin Neurol 2001; 14: 553–560.
Sligh JE, Levy SE, Waymire KG et al: Maternal germ-line transmission of mutant mtDNAs from embryonic stem cell-derived chimeric mice. Proc Natl Acad Sci USA 2000; 97: 14461–14466.
Sumegi B, Melegh B, Adamovich K, Trombitas K : Cytochrome oxidase deficiency affecting the structure of the myofibre and the shape of mitochondrial cristae membrane. Clin Chim Acta 1990; 192: 9–18.
Melegh B, Seress L, Bedekovics T et al: Muscle carnitine acetyl-transferase and carnitine deficiency in a case of mitochondrial encephalomyopathy. J Inherit Metab Dis 1999; 22: 827–838.
Melegh B, Bock I, Gati I, Mehes K : Multiple mitochondrial DNA deletions and persistent hyperthermia in a patient with Brachmann–de Lange phenotype. Am J Med Genet 1996; 65: 82–88.
Shoffner JM, Bialer MG, Pavlakis SG et al: Mitochondrial encephalomyopathy associated with a single nucleotide pair deletion in the mitochondrial tRNALeu(UUR) gene. Neurology 1995; 45: 286–292.
Melberg A, Arnell H, Dahl N et al: Anticipation of autosomal dominant progressive external ophthalmoplegia with hypo-gonadism. Muscle Nerve 1996; 19: 1561–1569.
Sengers RC, Trijbels JM, Willems JL, Daniels O, Stadhouders AM : Congenital cataract and mitochondrial myopathy of skeletal and heart muscle associated with lactic acidosis after exercise. J Pediatr 1975; 86: 873–880.
Valsson J, Laxdal T, Jonsson A, Jansson KK, Helgason H : Congenital cardiomyopathy and cataracts with lactic acidosis. Am J Cardiol 1988; 61: 193–194.
Rahman S, Blok RB, Dahl HH et al: Leigh syndrome: clinical features and biochemical and DNA abnormalities. Ann Neurol 1996; 39: 343–351.
Arii J, Tanabe Y : Leigh syndrome: serial MR imaging and clinical follow-up. AJNR Am J Neuroradiol 2000; 21: 1502–1509.
Santorelli FM, Barmada MA, Pons R, Zhang LL, DiMauro S : Leigh-type neuropathology in Pearson syndrome associated with impaired ATP production and a novel mtDNA deletion. Neurology 1996; 47: 1320–1323.
Rotig A, Bourgeron T, Chretien D, Rustin P, Munnich A : Spectrum of mitochondrial DNA rearrangements in the Pearson marrow–pancreas syndrome. Hum Mol Genet 1995; 4: 1327–1330.
Lacbawan F, Tifft CJ, Luban NL et al: Clinical heterogeneity in mitochondrial DNA deletion disorders: a diagnostic challenge of Pearson syndrome. Am J Med Genet 2000; 95: 266–268.
Schroder R, Vielhaber S, Wiedemann FR et al: New insights into the metabolic consequences of large-scale mtDNA deletions: a quantitative analysis of biochemical, morphological, and genetic findings in human skeletal muscle. J Neuropathol Exp Neurol 2000; 59: 353–360.
Muraki K, Nishimura S, Goto Y, Nonaka I, Sakura N, Ueda K : The association between haematological manifestation and mtDNA deletions in Pearson syndrome. J Inherit Metab Dis 1997; 20: 697–703.
Muraki K, Goto Y, Nishino I et al: Severe lactic acidosis and neonatal death in Pearson syndrome. J Inherit Metab Dis 1997; 20: 43–48.
Isashiki Y, Nakagawa M, Ohba N et al: Retinal manifestations in mitochondrial diseases associated with mitochondrial DNA mutation. Acta Ophthalmol Scand 1998; 76: 6–13.
Oldfors A, Fyhr IM, Holme E, Larsson NG, Tulinius M : Neuropathology in Kearns–Sayre syndrome. Acta Neuropathol (Berlin) 1990; 80: 541–546.
Acknowledgements
This work was supported in part from grants of the Hungarian National Science Foundation OTKA T- T 032670, T-035026 and from a grant of the Ministry of Health (ETT 329/2000).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bene, J., Nádasi, E., Kosztolányi, G. et al. Congenital cataract as the first symptom of a neuromuscular disease caused by a novel single large-scale mitochondrial DNA deletion. Eur J Hum Genet 11, 375–379 (2003). https://doi.org/10.1038/sj.ejhg.5200975
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejhg.5200975
Keywords
This article is cited by
-
Maternally inherited deafness and unusual phenotypic manifestations associated with A3243G mitochondrial DNA mutation
Pathology & Oncology Research (2005)