Abstract
The frequency of variant LHβ containing two point mutations (T986–C and T1008–C) and its relationship to reproductive disorders differ widely between ethnic groups. In a Japanese population, variant luteinizing hormone (LH) correlates with ovulatory disorders. Here we examined the relationship between two missense mutations and five silent mutations (C894–T, G1018–C, C1036–A, C1098-T and C1423–T) in the LHβ gene, and ovulatory disorders. We studied 43 patients with ovulatory disorders, 79 patients with normal ovulatory cycles, and 23 healthy men who agreed to join our DNA analysis. PCR-amplified LHβ-subunit gene sequences were compared with a base sequence of wild-type LH reported after direct sequencing. The highest frequency (0.945) of novel allele was observed at the position of the C1036–A transition. No homozygotes for wild-type LHβ (C1036) were identified. The frequency of novel allele in patients with polycystic ovary syndrome, endometriosis, premature ovarian failure and luteal insufficiency was significantly different from that of healthy women. The frequencies of novel alleles (C894–T, C1098–T and C1423–T) in patients with ovulatory disorders were significantly higher than those with normal ovulatory cycles. The mean incidence of point mutation in patients with ovulatory disorders was higher than in those with normal ovulatory cycles. Among patients with variant LH, five silent mutations were identified in 87.5% of patients with ovulatory disorders, whereas only a few silent mutations were identified in patients with normal ovulatory cycles. In a Japanese population, five silent mutations of variant LH could have influenced two missense mutations and/or other unknown missense mutations, causing ovulatory disorders.
Similar content being viewed by others
Introduction
Human luteinizing hormone (LH), a member of the glycoprotein hormone family, plays important roles in the regulation of gonadal function. LH is a ∂/β heterodimer with a common ∂ subunit and a unique β subunit, which confers hormonal specificity. The gene encoding LHβ subunit was cloned and sequenced in 1984,1 and is located on chromosome 19.2 Identification of mutations in key genes that regulate reproduction should explain many cases of infertility with unknown pathogenesis. Three genetic variants of LH were recently discovered. Two were caused by one missense point mutation in the LHβ-subunit gene, resulting in amino-acid alterations: Glu54→Arg54,3 and Ser102→Gly102.4 The other was caused by two missense point mutations in the LHβ-subunit gene, resulting in amino-acid alterations: Trp8→Arg8 and Ile15→Thr15.5,6 Furthermore, six silent polymorphisms in exons and introns of the LHβ-subunit gene have also been reported.4
In general, the variant forms of LH do not correlate with gynaecological diseases, including infertility. However, it is of particular interest to note that the frequency of the variant LHβ containing two missense point mutations differs widely between ethnic groups, varying from 0 to 52%,7 and the homozygotes for variant LH in the Finnish population are apparently healthy with no reported infertility or subfertility, while in the Japanese population variant LH is related to infertility and various menstrual disorders.6,8,9,10 We report here extremely high frequencies of novel allele in Japanese, and the relationship between two missense mutations and five silent mutations in the LHβ gene, and ovulatory disorders in Japanese women.
Methods
Subjects
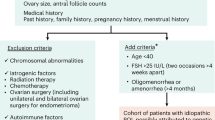
A total of 92 Japanese patients with endocrine disorders and/or gynaecological diseases participated in this study. Their ages ranged from 13 to 49 years (mean, 31.0±6.4 years, ±SD). Based on clinical features and laboratory examinations, 20 women were diagnosed with endo-metriosis; two with uterine leiomyoma, 22 with polycystic ovary syndrome (PCOS), 18 with premature ovarian failure (POF), 21 with luteal insufficiency, two with ovarian tumour; one with amenorrhoea caused by weight loss, one with obesity, one with thyroid disease and four with first-grade hypothalamic amenorrhoea (no menstruation for >6 months). Of these 92 Japanese patients, 43 had ovulatory disorders. Endometriosis, uterine myoma and ovarian tumour were diagnosed by histopathological examination from specimens after operation. Clinical PCOS was evaluated according to the criteria reported previously.11 The criteria involve menstrual disorders, endocrine abnormality (serum LH≥7 mIU/ml and FSH, normal 4–14 mIU/ml) and ultrasound detection of multiple ovarian small cysts (≥10 cysts) bilaterally. POF was defined as secondary amenorrhoea in association with elevated serum FSH (>14 mIU/ml) and LH (>10 mIU/ml) in women less than 40 years of age. Luteal insufficiency was defined based on ultrasound detection of ovulation and mid-luteal serum progesterone <15 ng/ml or out of phase endometrial biopsy. Peripheral blood was taken on the third to sixth day of menstruation or at any time in patients with amenorrhoea.
A total of 30 healthy fertile nonpregnant Japanese women ranging from 26 to 50 years of age (42.9±8.0 years) and 23 healthy fertile adult Japanese men ranging in age from 25 to 51 years (34.0±9.9 years) were studied. Subjects with known endocrinological disorders were excluded from this study. Samples from women were collected randomly during the menstrual cycle. Appropriate university hospital committee permission was obtained for the sample-collection protocol.
DNA amplification and sequencing analysis of LHβ gene
Genomic DNA was isolated from peripheral blood lymphocytes by using Sepa Gene nucleic acid isolation reagents (Sanko Junyaku, Tokyo, Japan) and was used directly as a polymerase chain reaction (PCR) template. A portion of the LHβ gene was amplified with A primer (5′-GGG AAT TCT CTT TGT GGG TGG TGT ACC ACG C-3′) and D primer (5′- GGA GGA TCC GGG TGT CAG GGC TCC A-3′) to span intron 1, exon 2 intron 2 and exon 3 of the LHβ gene.12 Underlines indicate introduced restriction enzyme sites for EcoRI and BamHI, respectively. The 50 μl PCR reaction mixture contained 0.2 mM of dNTPs, 12.5 pmol of a set of primers and 1.25 U of Ex Taq polymerase (Takara, Kyoto, Japan). After an initial denaturation at 97°C for 5 min, 25 cycles of denaturation at 97°C for 1 min, annealing at 62°C for 1 min and extension at 72°C for 2 min were performed, and final extension was carried out at 72°C for 5 min in a GeneAmp PCR system (Model 2400; Perkin-Elmer, Norwalk, CT, USA).
To distinguish between homozygotes and heterozygotes, PCR direct sequencing was performed. The amplified products (∼800 bp) were purified by microspin column (S-400 HR; Pharmacia, Uppsala, Sweden), and the DNA sequence was determined using A or B (5′-GGG TGA AGC AGT GTC CTT GT-3′) and C (5′-GAA GAG GAG GCC TGA GAG TT-3′) or D primers on an automated DNA sequencer (Model 373S; Perkin-Elmer). The 25-cycle profile consisted of denaturation at 96°C for 30 s, annealing at 50°C for 15 s and extension at 60°C for 4 min, except for the first cycle when denaturation at 96°C was extended to 5 min.
Statistical analysis
Data are expressed as mean±SD. Differences between groups were examined for statistical significance using Sheffe's F test or the χ2 test. A P-value <0.05 denoted the presence of a statistically significant difference.
Results
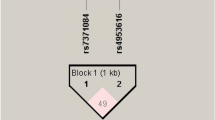
Direct sequencing revealed five polymorphisms in addition to the two reported point mutations (T986–C and T1008–C). The five mutations found in intron 1 occurred at nt 894 (C→T), in exon 2 at nt 1018 (G→C) and nt 1036 (C→A), in intron 2 at nt 1098 (C→T), and in exon 3 at nt 1423 (C→T). These mutations appeared to be silent polymorphisms (Figure 1). In all, 21 different patterns of polymorphisms in the LHβ-subunit gene were identified in all 145 subjects. The most common (32.4%) pattern of polymorphism was T894–T986–T1008–C1018–A1036–T1098–T1423. No homozygotes for wild-type LH occurred at nt 1036 (C) in exon 2. The two reported polymorphisms (T986–C/T1008–C) and two silent polymorphisms (C894–T/C1423–T) were in complete linkage disequilibria, respectively. Of these, 72% of linkage disequilibrium at positions 894 and 1423 was mutant-type (T) (Table 1).
The frequencies of each allele in 145 subjects are listed in Table 2. The highest frequency (0.945) of novel allele was the transition of C→A at nt 1036. The frequency of transitions of C→T at nt 894, nt 1423 and nt 1098 was 0.786, 0.786 and 0.683, respectively. The frequencies of novel allele at all positions in healthy women were not different from those of healthy men. The frequencies of novel allele at nt 1018 in patients with PCOS (0.955) and patients with POF (0.889) were significantly different from those of healthy women (0.700). The frequency of novel allele at nt 1018 in patients with luteal insufficiency (0.952) was significantly higher than in healthy women (0.633), whereas that in patients with endometriosis (0.300) and in patients with POF (0.250) was significantly lower than in healthy women. The frequency of novel allele at nt 1036 in patients with PCOS, patients with POF and patients with luteal insufficiency was all 1.00, with significant differences from those of healthy women (0.883). The frequency of novel allele at nt 1098 in patients with POF (1.000) was significantly higher than in healthy women (0.700), whereas that in patients with endometriosis (0.500) and patients with luteal insufficiency (0.429) was significantly lower than in healthy women. Comparison of the frequency of novel allele between patients with ovulatory disorders and normal ovulatory cycles showed that the frequencies of novel allele at nt 1018, 1098 and 1423 in patients with ovulatory disorders were significantly higher than the respective frequency in patients with normal ovulatory cycles.
The mean incidence of point mutation was 4.3±1.4 (range 1–7) for the entire group of subjects, 4.0±1.6 (range 1–5) for healthy women, 4.3±1.3 (range 1–5) for healthy men, 4.5±0.7 (range 3–5) for patients with PCOS, 3.7±1.4 (range 1–5) for patients with endometriosis, 4.9±1.2 (range 4–7) for patients with POF and 4.3±0.9 (range 1–5) for patients with luteal insufficiency. There were no significant differences in the mean values between the groups. However, the mean incidence of point mutation in patients with ovulatory disorders was 5.0±1.0 (range 4–7), which was significantly (P<0.0001) higher than in patients with normal ovulatory cycles (3.9±1.4; range 1–5). Eight of 14 patients with variant LH who had amino-acid substitution had ovulatory disorders, and seven (87.5%) of them had five silent mutations, the other patient had three silent mutations. On the other hand, six patients with normal ovulatory cycles had only one silent mutation (five patients) and three silent mutations (1 patient), respectively. None of the six women with normal ovulatory cycles has five silent mutations; however, seven of eight women with ovulatory disorders had five silent mutations, showing a statistically significant frequency (P=0.0012). With regard to subjects with three or more silent mutations, all women with ovulatory disorders (eight of eight women, 100%) had significantly high frequency compared with women with normal ovulatory cycles (one of six women, 16.7%) (P=0.0013).
Discussion
The LH variant differs functionally from wild-type LH, and it seems that both men and women who carry the variant are predisposed to mild aberrations of reproductive function.13 While the variant LH appears to have higher in vitro bioactivity compared with wild-type LH,14 it has a shorter circulatory half-life.15 Furthermore, regulation of the variant LH gene differs because of additional changes in the sequence of its promoter.16 Correlations between the occurrence of variant LH and various clinical conditions involving LH function suggest that it represents a biologically less active form of LH and may be related to borderline suppression of gonadal function, including subfertility.17
The frequency of the variant LHβ, which consists of two point missense mutations leading to two amino-acid substitutions (Trp8→Arg8 and Ile15→Thr15),5,6 differs widely between ethnic groups, from 0 to 52%.7 Based on the structure of hCGβ, variant LHβ and wild-type LHβ, it is possible that the variant LHβ appeared through gene conversion within the LHβ/hCGβ gene cluster, which may be predisposed to genetic recombination.1 It is also possible that variant LH represents an ancestral LH form, which is being replaced by wild-type LH.1 This process seems to be at different stages in different populations, as judged from the vast ethnic differences in frequency of allele at the two LHβ subunit.7 The reason for this remains unclear.
We reported previously that the frequency of the LHβ variant was 8.5% of healthy, fertile Japanese women.10 While several investigators have reported the clinical significance of the variant LH in Japanese patients with reproductive disorders including infertility and/or menstrual disorders,6,7,8,9,10,18 Finnish women carrying the variant LH, detected in 28% of the population, were reportedly fertile.15,19 Thus, evidence concerning the clinical significance of the variant with respect to reproductive disorders has been contradictory, and many unclear areas remain unresolved with respect to the physiological and pathophysiological significance of the variant LH. In this study, it is true that we did not find a statistically significant difference between women with ovulatory disorders and women with normal ovulatory cycles regarding frequency of novel allele of position 984 and 1008 of the variant form of LH. Besides, eight of 14 women with variant form of LH (57.1%) had ovulatory disorders, but six of 14 (42.9%) did not show ovulatory disorder. Although the purpose of this study was to investigate the relationship between point mutation (including silent mutation) and ovulatory/reproductive disorders, it is considered necessary to include a greater number of subjects and eliminate any bias, in order to study a relationship between variant LH and ovulatory disorders.
Thus, it is clear that there are two clinical phenotypes of women carrying variant LH (women with ovulatory disorders and women with normal ovulatory cycles). Why is the physiological function of the variant LH that has the same structural abnormality, different in these two phenotypes? In this study, we evaluated five polymor-phisms (C894–T, G1018–C, C1036–A, C1098–T and C1423–T)4 in addition to the two reported missense point mutations (T986–C and T1008–C).5,6 Five silent point mutations of the LHβ subunit identified in our study were the same mutations reported by Roy et al.4 In their study,4 they reported that all silent mutations, with similar coding, were in complete linkage disequilibria, and the frequency of novel allele was 0.612. However, only two silent polymorphisms (C894–T/C1423–T) were in complete linkage disequilibria in our study. The frequencies of novel allele differed between each position of the allele transition, and the highest frequency (0.945) of novel allele was observed at the position of the C1036–A transition. None of the homozygotes for wild-type LHβ subunit (C1036) reported1 was found in the Japanese population. The most common pattern of polymorphism was T894–T986–T1008–C1018–A1036–T1098–T1423 and 32.4% (47 of 145 cases). Although the reason for the different results between ours and Singapore is not clear, it may be suggested to be because of racial difference.
Furthermore, the frequencies of novel alleles (C894–T, C1036–A and C1423–T) in patients with PCOS, those (C894–T, C1036–A, C1098–T and C1423–T) in patients with POF and those (G1018–C and C1036–A) in patients with luteal insufficiency were significantly higher than the frequencies in healthy women, whereas the frequencies of novel alleles (G1018–C and C1098–T) in patients with endometriosis, those (G1018–C) in patients with POF and those (C1098–T) in patients with luteal insufficiency were significantly lower than the frequencies in healthy women. The frequencies of novel allele in intron 1 (C894–T), intron 2 (C1098–T) and exon 3 (C1423–T) in patients with ovulatory disorders were significantly higher than in those with normal ovulatory cycles. The mean incidence of point mutation in patients with ovulatory disorders was higher than in those with normal ovulatory cycles. Among patients with variant LH comprising missense mutations leading to amino-acid substitution, five silent mutations were identified in 87.5% of patients with ovulatory disorders, whereas only a few silent mutations were identified in patients with normal ovulatory cycle.
Thus, the frequencies of each novel allele differ in various ethnic groups. In the Japanese population, the frequency of novel allele of the LHβ subunit in patients with reproductive diseases such as PCOS, endometriosis, POF and luteal insufficiency differed from that in healthy women, and silent mutations at five sites of the LHβ subunit may be considered to have influenced the missense mutation at two sites and/or other unknown missense mutations, which might lead to ovulatory disorders. The reason for this remains unclear, but it is tempting to speculate that variant LH could offer an advantage in specific environmental conditions, based on functional characteristics. Although it is obvious that the silent mutation of the LHβ subunit does not directly influence ovulatory disorders or other reproductive disorders, multiple gene mutations may have existed in a wider range involving other genes, without limiting intron 1, exon 2, intron 2 and exon 3 of the LHβ subunit investigated in this study. Therefore, the silent mutation that we identified, of which the effect has not yet been confirmed, is hoped to be a clue in revealing a novel gene that may be a causal factor for ovulatory disorders or other reproductive disorders. Therefore, it is important for the clinician to be aware of these novel alleles of the LHβ subunit. Direct sequencing analysis of the LHβ subunit gene can be useful in the initial identification of mutant alleles and thus possibly in the diagnosis of LH-related disorders.
References
Talmadge K, Vamvakopoulos NC, Fiddes JC : Evolution of the genes for the beta subunits of human chorionic gonadotropin and luteinizing hormone. Nature 1984; 307: 37–40.
Hollenberg AN, Postoll RG, Albancse C, Boers ME, Jameson JL : Multiple promoter elements in the human chorionic gonadotropin beta subunit genes distinguish their expression from the luteinizing hormone beta gene. Mol Cell Endocrinol 1994; 106: 111–119.
Weiss J, Axelrod L, Whitcomb RW, Harris PE, Crowley WF, Jameson JL : Hypogonadism caused by a single amino acid substitution in the β subunit of luteinizing hormone. N Engl J Med 1992; 326: 179–183.
Roy Ac, Liao WX, Chen Y, Arulkumaran S, Ratnam SS : Identification of seven novel mutations in LHβ-subunit genes by SSCP. Mol Cell Biochem 1996; 165: 151–153.
Pettersson K, Makela MM, Dahlen P, Lamminen T, Huoponen K, Huhtaniemi I : Gene polymorphism found in the LH beta gene of an immunologically anomalous variant of human luteinizing hormone. Eur J Endocrinol 1994; 130 (Suppl. 2): S17.03 (abstract).
Furui K, Suganuma N, Tsukahara S et al: Identification of two point mutation in the gene coding luteinizing hormone (LH) β-subunit, associated with immunologically anomalous LH variant. J Clin Endocrinol Metab 1994; 78: 107–113.
Huhtaniemi I, Jiang M, Nilsson C, Pettersson K : Mutations and polymorphisms in gonadotropin genes. Mol Cell Endocrinol 1999; 151: 89–94.
Suganuma N, Furui K, Furuhashi M, Asada Y, Kikkawa F, Tomoda Y : Screening of the mutations in luteinizing hormone β-subunit in patients with menstrual disorders. Fertil Steril 1995; 63: 989–995.
Takahashi K, Kurioka H, Ozaki T et al: Increased prevalence of luteinizing hormone β-subunit variant in Japanese infertility patients. Hum Reprod 1988; 13: 3338–3344.
Takahashi K, Ozaki T, Okada M, Kurioka H, Kanasaki H, Miyazaki K : Increased prevalence of Luteinizing hormone β-subunit variant in patients with premature ovarian failure. Fertil Steril 1999; 71: 96–101.
Takahashi K, Eda Y, Abu-Musa A, Okada S, Yoshino K, Kitao M : Transvaginal ultrasound imaging, histopathology and endocrinopathy in patients with polycystic ovarian syndrome. Hum Reprod 1994; 9: 1231–1236.
Okuda K, Yamada T, Imoto H, Komatsubara H, Sugimoto O : Antigenic alterations of an anomalous human luteinizing hormone caused by two chorionic gonadotropin-type amino acid substitutions. Biochem Biophys Res Commun 1994; 200: 584–590.
Huhtaniemi IT : Polymorphism of gonadotropin action: clinical implications. Asian J Androl 2000; 2: 241–246.
Suganuma N, Furu K, Kikkawa F, Tomada Y, Furuhashi M : Effect of the mutations (Trp8→Arg and Ile15→Thr) in human luteinizing hormone (LH) β-subunit on LH bioactivity in vitro and in vivo. Endocrinology 1996; 137: 831–838.
Haavisto AM, Pettersson K, Bergendahl M, Virkamaki A, Huhtaniemi I : Occurrence and biological properties of a common genetic variant of luteinizing hormone. J Clin Endocrinol Metab 1995; 80: 1257–1263.
Jiang M, Pakarinen P, Zhang FP et al: A common polymorphic allele of the human luteinizing hormone beta-subunit gene: additional mutations and differential function of the promoter sequence. Hum Mol Genet 1999; 8: 2037–2046.
Lamminen T, Huhtaniemi I : A common genetic variant of luteinizing hormone; relation to normal and aberrant pituitary-gonadal function. Eur J Pharmacol 2001; 414: 1–7.
Okuno A, Komori S, Sakata K et al: Genetic analysis of a variant luteinizing hormone in an infertile woman. Arch Gynecol Obstet 2001; 265: 148–150.
Nilsson C, Pettersson K, Millar RP et al: World frequency of a common genetic variant of luteinizing hormone: an international collaborative research. Fertil Steril 1997; 67: 998–1004.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Takahashi, K., Karino, K., Kanasaki, H. et al. Influence of missense mutation and silent mutation of LHβ-subunit gene in Japanese patients with ovulatory disorders. Eur J Hum Genet 11, 402–408 (2003). https://doi.org/10.1038/sj.ejhg.5200968
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejhg.5200968
Keywords
This article is cited by
-
A brief insight into the etiology, genetics, and immunology of polycystic ovarian syndrome (PCOS)
Journal of Assisted Reproduction and Genetics (2022)