Key Points
-
Unilateral partial dentures are seldom advocated due to the risk of swallowing or inhalation.
-
Hinged or 'swing-lock' arms can improve the retention of partial dentures.
-
Prosthetic flanges can be a useful tool to mask gingival recession.
Abstract
This report describes a unilateral removable partial denture with a hinged arm with magnetic retention and a prosthetic flange component that was provided for a patient with localised periodontal tissue loss. While a unilateral partial denture is not generally advocated because of the risk of swallowing or aspiration, this case illustrates the effective use of such a design.
Similar content being viewed by others
Main
Unilateral partial dentures have been suggested for the restoration of short span, bounded edentulous spaces. This design of prosthesis has some advantages for the patient in that the use of an extensive palatal or lingual major connector is avoided and no preparation of the adjacent teeth is required for the provision of bridgework; for this reason they continue to be requested by patients and clinicians.1,2 However, two drawbacks are that the prosthesis should be removed and cleaned after each meal and the design provides no cross-arch stabilisation, which can result in it being easily dislodged.
If dislodged, a further and very serious complication that has been widely reported is that the denture may be swallowed or aspirated, often resulting in hospitalisation. Perforation of internal organs can occur, particularly when clasps are present, and surgical intervention to retrieve the prosthesis may be needed.3,4,5,6 Due to this potential hazard, the use of a unilateral partial denture is generally not advised and a full denture, bridgework implant-retained restoration is advocated.5,7 The prosthesis provided in this case, however, was well retained by the inclusion of a hinged arm and labial prosthetic flange.
The hinged removable partial denture was first described by Simmons in 1963 as a 'swing-lock denture'.8 The traditional swing-lock design consists of a labial or buccal retaining bar that is hinged at one end and locked by a latch at the other, together with a reciprocating lingual or palatal plate; a specific 'swing-lock' component is required for its manufacture. The denture is made with a path of insertion in one plane with the hinged arm having an arc of opening in another, typically labial, direction. When closed, rigid extensions from the bar or an attached acrylic veneer locks into the undercut areas of the teeth, resulting in excellent retention and stability and making the denture virtually immobile until the bar is released.9,10 Clearly all other principles for partial denture design should be adhered to such as a rigid connector and rests providing tooth support and bracing components.
Numerous indications for the use of a hinged or swing-lock design have been proposed such as: missing key abutment teeth and unilateral abutments; unfavourable tooth and soft and hard tissue contour; reduced bone support; and the presence of certain ablative defects following cancer surgery.10,11,12,13,14 Some contraindications include poor manual dexterity, soft tissue limitations and poor oral hygiene. Care must be taken to ensure that excessive demands are not placed on the abutment teeth due to the rigid nature of the fixing of the denture; however, a carefully designed prosthesis can help to distribute the loads to several teeth rather than just a few vulnerable abutments.9,10
The use of an acrylic flange incorporated onto the bar of the denture in order to mask gingival recession in treated periodontal disease has been reported previously.10,14 This component acts like any form of gingival veneer and improves aesthetics in patients with altered gingival contour, particularly following surgery, by covering and lightly engaging the interdental spaces and disguising them.15
Case report
A thirty-eight year old Caucasian male was referred to Newcastle Dental Hospital in 2000 for treatment of his periodontal disease. The patient presented complaining of occasional bleeding on brushing and some tenderness associated with several teeth. There was a family history of periodontal disease; his mother and sister had received periodontal care in the past. He did not have any relevant medical history and admitted to smoking up to three cigarettes per day.
Subsequent examination revealed generalised bone loss of up to 25% with localised areas of infra-bony pocketing of 7 mm or more in each quadrant. A diagnosis of aggressive periodontitis was made and the patient was managed with a combination of non-surgical management, open flap curettage and the use of adjunctive antimicrobials.
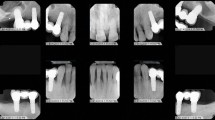
Treatment produced a favourable response with a generalised reduction in probing depth of around 1 to 2 mm. However, significant infra-bony pocketing remained around the upper right canine which measured 10 mm palatally. The tooth had localised gingival recession and had overerupted. It was involved in lateral guidance but there did not appear to be excessive occlusal force and minimal fremitus was detected. A radiograph revealed around 50% bone loss but the root was a considerable length (Fig. 1). Following discussion with the patient, it was decided to manage this localised problem with a combination of pocket elimination surgery palatally and guided tissue regeneration (GTR) using a combination of autogenous bone chips, Bio-Oss® and Bio-Gide® resorbable membrane (Geistlich Biomaterials, Wolhusen, Switzerland) (Fig. 2).
This intervention produced a significant reduction in probing depth from 10 mm to 4 mm palatally. Unfortunately a combination of the periodontal disease and surgery resulted in a significant amount of localised recession that was of concern to the patient, but he expressed even more concern in relation to the sensation of his tongue on the lengthened tooth and widened embrasure spaces (Fig. 3).
On review of the periodontal status and oral hygiene level, it was decided to provide the patient with a removable prosthesis in order to mask the recession labially and close the embrasure spaces palatally. It was also decided to replace the missing 15 and 16 in an effort to improve function for the patient as well as to maximise retention.
A silicone impression was recorded in a special tray using a standard impression technique and a unilateral removable partial denture was made. This denture had a cobalt chrome major connector to engage the embrasure spaces palatally and a prosthetic labial flange that was attached on a hinged arm that fastened onto the major connector by the use of a magnet. A 300 g × 1.5 mm Dyna® magnet was incorporated into the major connector using cold cure acrylic, and a minor connector from the hinge arm was made of Dyna magnetic alloy, soldered to the cobalt chrome framework (Dyna Dental Engineering, Bergen op Zoom, Noord Brabant, Netherlands) (Fig. 4).
Fig. 4b shows the magnet to retain the hinged arm (arrowed)
The magnet is used principally as a stop with enough force to keep the bar closed. The retention of the denture is achieved through the engagement of undercuts by the framework and particularly the acrylic flange, designed as a conventional gingival veneer.15 Indeed, the engagement of undercuts at the most anterior extension of the flange allowed a better aesthetic result to be achieved as it would not have otherwise been possible to extend the acrylic flange as far anteriorly due to the leverage that would have been applied to the magnet.
The patient adapted to the prosthesis very quickly and is delighted with the coverage of the embrasures palatally as well as the improved appearance (Figs 5,6). He is also satisfied with the improved function the denture provides for him due to the replacement of the missing teeth.
Discussion
A unilateral design of partial denture was deemed to be appropriate in this case as the combination of the hinged arm and acrylic flange produced a very retentive and stable prosthesis. In addition to this, the replacement of the missing 15 and 16 resulted in a prosthesis of some considerable size, making swallowing unlikely. The use of a magnet rather than some form of latch or split-pin to secure the hinged arm is another example of the growing use of magnets in restorative dentistry and dentistry in general.16
Although the patient requested that the appearance be improved, it was interesting that the main concern was the sensation of the open embrasure spaces around 13 on contact with his tongue. Other functional concerns that have been reported by patients with wide embrasure spaces such as this include phonetic problems resulting in sibilant speech due to increased airflow through the spaces, and bubbling of saliva.15,17 However, neither was a cause for concern in this case.
Clearly the need for regular review and periodontal maintenance is required. It is known that partial denture wearing in general may result in increased plaque accumulation in the absence of adequate oral hygiene.18,19 With regard to the swing-lock denture in particular, studies have shown that in patients who maintain a good level of oral hygiene, the dentures are very well tolerated and no significant further periodontal breakdown need be seen, even when there is unfavourable periodontal support.20,21 The patient has continued to maintain excellent oral hygiene in the nine months following delivery of the prosthesis and he has been enrolled in a regular maintenance programme. There has been no evidence of further periodontal tissue loss.
References
Curtis D A, Curtis T A, Wagnild G W et al. Incidence of various classes of removable partial dentures. J Prosthet Dent 1992; 67: 664–667.
Owall B E, Taylor R L . A survey of dentitions and removable partial dentures constructed for patients in North America. J Prosthet Dent 1989; 61: 465–470.
Nimmo S S, Nimmo A, Chin G A . Ingestion of a unilateral removable partial denture causing serious complications. Oral Surg Oral Med Oral Pathol 1988; 66: 24–26.
Goodacre C J . A dislodged and swallowed unilateral removable partial denture. J Prosthet Dent 1987; 58: 124–125.
Ganz S D . The replacement of a unilateral partial denture with an implant supported fixed prosthesis: a clinical report. Implant Dent 1998; 7: 159–165.
Dunn J R . Patient swallows removable partial denture: a clinical report. J Prosthet Dent 1996; 76: 571–572.
Bohnenkamp D M . Replacement of a fractured unilateral removable partial denture with a nonrigid fixed prosthesis: a clinical report. J Prosthet Dent 1996; 75: 591–593.
Simmons J I . Swing-lock stabilisation and retention. A preliminary clinical report. Texas Dent J 1963; 81: 10–12.
Becker C M, Bolender C L . Designing swinglock partial dentures. J Prosthet Dent 1981; 46: 126–132.
Chan M F, Adams D, Brudvik J S . The swing-lock removable partial denture in clinical practice. Dent Update 1998; 25: 80–84.
Adams D . A cantilevered swinglock removable partial denture design for the treatment of the partial mandibulectomy patient. J Oral Rehabil 1985; 12: 113–118.
Black W B . Surgical obturation using a gated prosthesis. J Prosthet Dent 1992; 68: 339–342.
Bolender C L, Becker C M . Swinglock removable partial dentures: where and when. J Prosthet Dent 1981; 45: 4–10.
Talbot T R . Review of the Swinglock removable partial denture. Int J Prosthodont 1991; 4: 80–88.
Blair F M, Thomason J M, Smith D G . The flange prosthesis. Dent Update 1996; 23: 196–199.
Riley M A, Walmsley A D, Harris I R . Magnets in prosthetic dentistry. J Prosthet Dent 2001; 86: 137–142.
L'Estrange P R, Strahan J D . The wearing of acrylic periodontal veneers. Br Dent J 1970; 128: 193–194.
Addy M, Bates J F . The effect of partial dentures and chlorhexidine gluconate gel on plaque accumulation in the absence of oral hygiene. J Clin Periodontol 1977; 4: 41–47.
Brill N, Tryde G, Stoltze K et al. Ecologic changes in the oral cavity caused by removable partial dentures. J Prosthet Dent 1977; 38: 138–148.
Schulte J K, Smith D E . Clinical evaluation of swinglock removable partial dentures. J Prosthet Dent 1980; 44: 595–603.
Gomes B C, Renner R P, Antos E W et al. A clinical study of the periodontal status of abutment teeth supporting swinglock removable partial dentures — a pilot study. J Prosthet Dent 1981; 46: 7–13.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Barker, D., Cooper, A. A novel use of a unilateral hinged partial denture. Br Dent J 201, 571–573 (2006). https://doi.org/10.1038/sj.bdj.4814207
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4814207
This article is cited by
-
Unilateral removable partial dentures
British Dental Journal (2017)