Key Points
-
Twelve million adults smoke in the UK, and smoking is responsible for 114,000 deaths each year.
-
Carbon monoxide levels may be a good indicator of the degree of addiction to nicotine.
-
The dental profession has a crucial role to play in smoking cessation counselling, particularly for patients with chronic periodontitis.
-
This study shows that there is great potential for smoking cessation intervention in clinic settings.
Abstract
Background There are limited data on the utility of dental professionals in providing smoking cessation counselling in the UK.
Objectives The purpose of this study was to determine quit rates for smokers with chronic periodontitis who were referred to a dental hospital for treatment.
Materials and methods Forty-nine subjects with chronic periodontitis who smoked cigarettes were recruited. All subjects received periodontal treatment and smoking cessation advice as part of an individual, patient-based programme provided by dental hygienists trained in smoking cessation counselling. Smoking cessation interventions included counselling (all patients), and some patients also received nicotine replacement therapy (NRT) and/or Zyban medication. Smoking cessation advice was given at each visit at which periodontal treatment was undertaken (typically four to six visits) over a period of 10-12 weeks. Smoking cessation advice was also given monthly during the programme of supportive periodontal care over the following nine months. Smoking status was recorded at three, six and 12 months and was confirmed with carbon monoxide (CO) monitors and salivary cotinine assays.
Results Forty-one per cent, 33%, 29% and 25% of patients had stopped smoking at week four, months three, six and 12, respectively. Gender, age, the presence of another smoker in the household, and baseline smoking status (determined using subject-reported pack years of smoking) were not significant predictors of quit success (P < 0.05). Baseline CO levels were significantly associated with quit success, however, and were significantly higher in those subjects who continued to smoke compared to those subjects who were quitters at week four, month three and month six (P < 0.05).
Conclusion Success rates in quitting smoking following smoking cessation advice given as part of a periodontal treatment compared very favourably to national quit rates achieved in specialist smoking cessation clinics. The dental profession has a crucial role to play in smoking cessation counselling, particularly for patients with chronic periodontitis.
Similar content being viewed by others
Introduction
Smoking and tobacco use carry high risks to human health. In the UK, 12 million adults smoke (28% of men and 24% of women).1,2 Smoking is responsible for 114,000 deaths each year1 which represents one in every five deaths in the UK. Most of these deaths are from lung cancer, coronary heart disease and chronic obstructive lung disease,3 the main diseases associated with smoking. It is estimated that about half of all smokers will eventually be killed by their habit.1
From the oral perspective, smoking has been established as causal for oral and pharyngeal cancer and is responsible for more than 75% of deaths caused by these malignancies in the United States. Smoking has also been related to increased risks of implant failure.4 Numerous investigations of the relationship between smoking and periodontal disease have been performed over the last 17 years which provide substantial evidence for the detrimental effects of smoking on the periodontal tissues.5 Smoking is associated with increased rates of alveolar bone loss, attachment loss and pocket formation; in addition it exerts a masking effect on gingival symptoms of inflammation.6 The mechanisms by which smoking affects periodontal tissues appear to be mediated through defects in neutrophil function, impaired serum antibody responses to periodontal pathogens, diminished gingival fibroblast function and effects on vasculature.5,7 The prevalence and severity of periodontal disease in former smokers is decreased compared to current smokers, providing evidence that smoking cessation appears to be beneficial. Furthermore, smokers predominate among 'refractory periodontitis' patients who are resistant to conventional treatment.7 Smoking also impairs the outcome of surgical periodontal therapy, most likely through direct interference with the healing process.8
In view of the potential benefit of quitting smoking for patients with chronic periodontitis, the aim of this project was to evaluate the role of the dental team in providing smoking cessation advice within a secondary care environment to a cohort of patients with periodontal disease.
Materials and methods
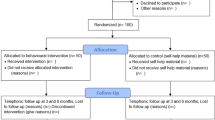
This study was part of a larger clinical trial on the effect of smoking cessation on periodontal treatment outcomes. Briefly, a 12 month, longitudinal clinical trial was designed to assess the response to periodontal treatment in smokers who quit smoking and to compare outcomes to those in smokers who did not quit. Prior to study commencement, ethical approval was granted by the local research ethics committee (LREC) of Newcastle and North Tyneside.
Subjects were recruited from periodontal diagnostic clinics at Newcastle Dental Hospital. All subjects had untreated moderate to severe chronic periodontitis and were smokers with a stated desire to quit the habit. Patients who wished to continue smoking ('contented smokers') were not entered into the study. Any patient with a history of medication that precluded pharmacological smoking cessation intervention was excluded.
Study design
The study encompassed five main time points: the initial visit (baseline), week four, month three, month six and month 12. At the baseline visit, carbon monoxide (CO), salivary cotinine readings and the number of pack years of smoking were recorded. A quit date was set, which was between the first and second treatment visits. Smoking cessation counselling was given to all patients and smoking cessation products were discussed. Conventional periodontal treatment was undertaken between the baseline visit and month three over approximately four to six visits, and supportive periodontal care was provided over the following nine months at three-monthly intervals. In addition to the three-monthly periodontal maintenance appointments, the patient was also seen at monthly intervals for reinforcement of the smoking cessation programme and to obtain CO readings that were used to confirm quit status. Salivary cotinine readings were taken at baseline and at months three and 12, mainly to confirm quit status, but also to use as an ongoing chairside motivational tool.
Smoking cessation strategies
Smoking cessation advice was given at the first periodontal treatment visit by a dental hygienist who had been trained as a smoking cessation counsellor and this advice was subsequently reinforced at each recall visit. A variety of methods were employed to assist smoking cessation according to individual needs:
-
Counselling (provided to all patients, including education about the benefits of quitting smoking and setting a quit date)
-
Nicotine replacement therapy (NRT) in the form of lozenges, chewing gum, inhalers or patches
-
Bupropion hydrochloride sustained-release preparation (Zyban). Prescription of Zyban was undertaken by the consultant with overall responsibility for the patient's care after consultation with the subject's general medical practitioner.
The choice of which smoking cessation methods to use in addition to counselling was made by the patient in consultation with the smoking cessation counsellor (ie the dental hygienist).
Monitoring smoking cessation status
Compliance with reported quit status was assessed by a variety of methods, including:
-
Diaries (self-reporting)
-
CO monitors to measure the content of CO in expired air. CO is absorbed from burning tobacco and competes with oxygen to form carboxy-haemoglobin which is excreted in exhaled breath to be detected by the CO monitor. The monitor shows the amount of CO in parts per million (ppm) in breath which indirectly gives a measure of blood carboxy-haemoglobin
-
Nicotine concentrations in saliva using a disposable, near patient (chair-side), colorimetric test kit at baseline, three and 12 months (Mermaid Diagnostics, UK). Cotinine is a nicotine metabolite and can be identified in saliva of smokers. The test depends on measuring nicotine metabolites, which is a very reliable way of determining smoking status. It is a six minute test, which detects nicotine and all associated breakdown products with a positive sample turning pink/orange in colour.
Statistical analyses
Statistical analyses were based on the assumption that those subjects who withdrew from the study early (failed to return for recall appointments) continued smoking. At each post-baseline time point (week four, months three, six and 12), therefore, subjects were categorised as being either 'quitters' (those subjects who definitely quit smoking, based on subject reporting, CO and salivary cotinine data) or 'non-quitters' (those subjects who definitely continued to smoke, and also those who withdrew early). Point prevalence rather than continuous quit status was recorded as percentage quit rates at each time point.
Data were analysed using SPSS version 10. All tests were two-tailed and the level of significance was set at P = 0.05. Associations between quit method and quit success at week four, and months three, six and 12 were analysed using the Fisher exact test. Determinations of the effects of gender and the presence of another smoker in the subject's household on quit success were also investigated using Fisher's exact test. Regression analyses were undertaken to evaluate whether age or reported history of smoking (baseline pack-years) were significant predictors of quit success. Independent samples t tests were undertaken to identify whether significant differences existed between quitters and non-quitters at each time point with respect to CO and salivary cotinine data. Regression analyses were also used to investigate whether baseline CO and salivary cotinine data were significant predictors of quit success or not.
Results
Forty-nine patients were recruited of whom 18 were males and 31 females. The mean (SD) age of the enrolled subjects was 42.0 (8.7) years and the pack years of smoking ranged from two to 80 with a mean (SD) of 24.5 (13.9) pack years. At week four the quit rate was 41%, and at months three, six and 12, it was 33%, 29% and 25%, respectively. There were 20 withdrawals at month 12 (accounting for 41% of the subjects who were enrolled).
All subjects received smoking cessation counselling during the study, and all were set quit dates. Of the 49 patients enrolled, six were also prescribed Zyban as part of the cessation regimen, 27 patients used nicotine replacement therapy, three used both Zyban and NRT, and 13 received only counselling. CO readings at week four and months three, six and 12 were consistently and significantly lower in the quitters compared to the non-quitters (P < 0.05), as might be expected in patients who quit smoking. Salivary cotinine scores were significantly lower in the quitters compared to the non-quitters only at month 12 (P < 0.05).
No statistically significant differences were identified between quitters and non-quitters with respect to the number of pack years at any time point (P < 0.05), and baseline smoking status as determined by pack years of smoking was not a significant predictor of quit success (P < 0.05). However, when we looked retrospectively at the baseline CO readings, the patients who subsequently were quitters at four weeks, three months or six months were found to have significantly lower baseline CO levels than non-quitters (P < 0.05) (month six data shown in Table 1). Regression analyses found that CO readings at baseline were statistically significant predictors of quit status at week four, month three and six (P < 0.05). Salivary cotinine data at baseline were not found to be significant predictors of quit success (P < 0.05).
Neither age nor gender were found to be related to quit success (P < 0.05). No significant associations were identified between quit success (at any time point) and the method used for quitting smoking (P < 0.05) (data for month 12 are shown in Table 2). However, it should be recognised that the purpose of this study was not to compare the success rates for different quit methods and in any case, the numbers of subjects in each group were too low to allow meaningful comparisons to be made.
Data were only available for 39 individuals with regards to the presence of another smoker in their household. Of those 39 subjects, 22 (56%) had at least one additional smoker in the household. Thirty-five per cent of subjects who had no smokers in the household quit smoking, compared to 36% of those who had another smoker in the household. The presence of another smoker in the household did not significantly influence quit success (P < 0.05). CO readings at week four, and months three, six and 12, and salivary cotinine readings at month three and 12 were not affected by the presence of another smoker in the household (P < 0.05) (data not shown).
Discussion
It has been shown previously in the USA that dental hygienists are effective in providing smoking cessation advice when given the proper training.9 The quit rates in this study compare favourably with previous studies carried out in the UK by dental personnel which showed quit rates of 11 to 18%.10,11 Similar rates of 14-15% have been achieved by general medical practitioners.12 The percentage of quitters tends to fall with time, indicating the difficulty in maintaining continuous abstinence.9
Currently two thirds of smokers in the UK have a desire to stop13 but only about 3% manage to stop permanently each year, with many requiring multiple attempts before succeeding. The strong addiction to smoking is why most of quit attempts end in failure.14,15 Our study was carried out in a hospital setting on patients who had been referred to the periodontal department with chronic periodontitis. There was ample time for the provision of smoking cessation counselling as part of the treatment regimen. Questionnaire studies have shown that dentists believe that obstacles to smoking cessation counselling include lack of time and cost effectiveness.16,17 Studies have also highlighted the importance of training the dental team as the lack of confidence and coordination with smoking cessation services are also viewed as obstacles to providing smoking cessation advice.18,19 With appropriate training and adequate support materials, oral health care professionals can address their patients' smoking habits.9,20
It is notable that the results of this study showed that success in quitting smoking did not appear to be related to the quit method used, a finding at variance with previously reported studies. However, it is very important to note that the present study did not aim to assess the success rates of different quit methods, and certainly was not sufficiently powered to do this. This study aimed primarily to investigate the effectiveness of smoking cessation programmes provided in the dental care setting. Our finding that quit method did not significantly influence quit success may support the concept that the quality of the interaction between the healthcare professional and the patient that occurs during smoking cessation counselling (which was provided to all patients) may be the most important determinant of quit success, but this hypothesis would need to be tested in future studies.
The need to engage the dental team in smoking cessation is considerable and recommendations for brief interventions in dental office settings for smokers published by the National Cancer Institute in the USA and known as the '5A's' (previously the 4 A's21) were shown to be effective. Guidelines were also published for those subjects not ready to make a quit attempt and are known as the '5R's'.22
In the US at least 50 dental organisations have adopted policy statements about tobacco use. Nearly half of dental schools and dental hygiene programs provide clinical tobacco intervention services23 and several US dental schools have established highly structured, individual outpatient smoking cessation programs.24 In the UK, the role of the dental team in smoking cessation needs to be expanded to include intervention in primary care settings, and recently published guidelines emphasise the important role of primary care health professionals in delivering smoking cessation advice and support.25
The number of pack years was found to be a poor predictor for quit success and did not appear to have an impact on the decision by the subjects to use additional methods for smoking cessation. CO readings, however, were good predictors for quit status. For example quitters were found to have significantly lower CO readings at post-baseline time points, which suggests that CO is sensitive and discriminatory in determining smoking status and quit potential. In other words, CO levels may be a good indicator of the degree of addiction to nicotine.
In summary, the results of this study show that there is great potential for smoking cessation intervention in dental clinic settings. The quit rate at week four was 41%, and at 12 months, a quarter of the enrolled subjects had quit smoking (quit rate 25%). As all withdrawals were regarded as non quitters, our quitters number may be an underestimate. These quit rates compare very favourably with those reported previously following smoking cessation counselling in the dental office setting. For example, in a review of studies among dental care providers regarding tobacco cessation programmes,26 it was reported that dentists who implemented smoking cessation in their practices achieved quit rates of 10-15% per year. The 12 month quit rate in our study was approximately twice that reported in these previous studies. We attribute this to the high quality of training in providing smoking cessation counselling that the dental hygienists received, and the frequent contact and close working relationships they had with the patients enrolled in the programme. The results of this study should encourage development of the role of the dental team in smoking cessation. It should be noted that this study was carried out in a secondary care setting and the results may therefore not be directly transferable to the general dental service, however. The next step should be to expand such research into primary dental care.
References
ASH Factsheet January 2005. Smoking statistics. ASH action on smoking and health. www.ash.org.uk.
Smoking kills: A White Paper on Tobacco. London: Secretary of State for Health and Secretaries of State for Scotland, Wales and Northern Ireland, 1998.
Callum C . The UK smoking epidemic: Deaths in 1995. London: Health Education Authority, 1998.
Research Science and Therapy Committee of the American Academy of Periodontology. Position paper: tobacco use and the periodontal patient. J Periodontol 1999; 70: 1419– 1427.
Kinane DF, Chestnutt IG . Smoking and periodontal disease. Crit Rev Oral Biol Med 2000; 11: 356– 365.
Bergstrom J, Preber H . Tobacco use as a risk factor. J Periodontol 1994; 65: 545– 550.
Haber J . Cigarette smoking: a major risk factor for periodontitis. Curr Opin Periodontol 1994; 12– 18.
Preber H, Bergstrom J . Effect of cigarette smoking on periodontal healing following surgical therapy. J Clin Periodontol 1990; 17: 324– 328.
Gordon JS, Severson HH . Tobacco Cessation through dental office settings. J Dent Educ 2001; 65: 354– 363.
Macgregor IDM . Efficacy of dental health advice as an aid to reducing cigarette smoking. Br Dent J 1996; 180: 292– 296.
Smith SE, Warnakulasuriya KA, Feyerabend C et al. A smoking cessation programme conducted through dental practices in the UK. Br Dent J 1998; 185: 299– 303.
Russell MA, Wilson C, Taylor C, Baker CD . Effect of general practitioners' advice against smoking. Br Med J 1979; 2: 231– 235.
Bridgewood ALR, Thomas M . Living in Britain: Results from the 1998 General Household Survey. London: Office of National Statistics, Social Survey division, The Stationery Office, 2000.
West R, Schneider, N . Craving for cigarettes. Br J Addict 1987; 82: 407– 415.
Killen JD, Fortmann SP, Newman B, Varady A . Prospective study of factors influencing the development of craving associated with smoking cessation. Psychopharmacology 1991; 105: 191– 196.
Gerbert B, Coates T, Zahnd E et al. Dentists as smoking cessation counselors. J Am Dent Assoc 1989; 118: 29– 32.
John JH, Yudkin P, Murphy M et al. Smoking cessation interventions for dental patients-attitudes and reported practices of dentists in the oxford region. Br Dent J 1997; 183: 359– 364.
Sverson HH, Eakin EG, Stevens VJ, Lichtenstein E . Dental office practices for tobacco users: independent practice and HMO clinics. Am J Public Health 1990; 80: 1503– 1505.
Campbell HS, Macdonald JM . Tobacco counselling among Alberta dentists. J Can Dent Assoc 1994; 60: 218– 226.
Cohen SJ, Stookey GK, Katz BP et al. Helping smokers quit: a randomised controlled clinical trial with pr ivate practice dentists. J Am Dent Assoc 1989; 118: 41– 45.
Mecklenburg RE, Christen AG et al. How to help your patients stop using tobacco: a National Cancer Institute Manual for the Oral Health Team. Bethesda, MD: National Institutes of Health, National Cancer Institute, 1993.
Fiory MC, Bailey WC, Cohen SJ et al. Treating tobacco use and dependence: Clinical practice guideline. Rockville MD: US Department of Health and Human Services, 2000.
Tomar SL . Dentistry's role in tobacco control. J Am Dent Assoc 2001; 132 Suppl: 30S– 35S.
Christen AG . Tobacco cessation, the dental profession, and the role of dental education. J Dent Educ 2001; 65: 368– 374.
Raw M, McNeill A, West R . Smoking cessation guidelines for health professionals. A guide to effective smoking cessation interventions for the health care system. Health Education Authority. Thorax 2000; 5: 987– 999.
Warnakulasuriya S . Effectiveness of tobacco counseling in the dental office. J Dent Educ 2002; 66: 1079– 1087.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Nasry, H., Preshaw, P., Stacey, F. et al. Smoking cessation advice for patients with chronic periodontitis. Br Dent J 200, 272–275 (2006). https://doi.org/10.1038/sj.bdj.4813307
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4813307
This article is cited by
-
Assessment of smoking behaviour in the dental setting. A study comparing self-reported questionnaire data and exhaled carbon monoxide levels
Clinical Oral Investigations (2012)
-
A pilot study combining individual-based smoking cessation counseling, pharmacotherapy, and dental hygiene intervention
BMC Public Health (2010)
-
Smoking advice for periodontitis patients
British Dental Journal (2006)