Key Points
-
Fifty patients with generalised severe periodontitis were examined to identify which teeth required radiographic assessment.
-
Panoramic radiographs were taken and examined. It was decided that, on average, 4.3 supplementary periapical views would be required for adequate periodontal assessment of all the affected teeth and, if teeth requiring dental radiographic assessment were added, 5.1 supplementary periapical views would be required.
-
This paper demonstrates that the effective radiation dose from a series of periapical radiographs of all the affected teeth would, in most cases, have been less than the dose from the panoramic-plus-periapicals approach.
-
These conclusions are specific for the equipment and exposure factors used with which, therefore, it is difficult to justify the use of panoramic radiography for periodontal assessment.
-
This paper also demonstrates how evidence can be obtained to develop radiographic selection criteria of the periodontal tissues.
Abstract
Objective Radiographic assessment of patients with generalised severe periodontitis may be undertaken with a panoramic view and supplementary periapicals. The purpose of this study was to estimate the effective radiation dose from this form of radiographic assessment, and to compare it with an estimate of the dose from a series of periapicals of all the affected teeth.
Design Cross-sectional observational study.
Setting Departments of Periodontology and Radiology, Glasgow Dental Hospital and School.
Method Fifty consecutive patients [were recruited] with sufficiently widespread advanced periodontitis to require at least seven periapical radiographs. [Following new local guidelines, a panoramic view was taken.] The adequacy of the image of every affected tooth and the number of supplementary periapicals required was determined by a panel of four examiners who also calculated the number of periapicals which would have been taken if panoramic radiography had not been available. An effective dose of 0.001 mSv for one periapical and 0.007 mSv for a panoramic view was assumed.
Results The panoramic-plus-periapicals approach delivered an estimated additional effective dose to 86% of patients, in the order of 0.001 – 0.007 mSv.
Conclusions Within the parameters of this investigation, the anticipated effective radiation dose from a series of periapical radiographs of all selected teeth would, for the great majority of patients, have been less than the dose from a panoramic-plus-periapicals approach.
Similar content being viewed by others
Introduction
For patients with periodontitis, radiographs are used to obtain a visual image of the bone support around affected teeth to determine: the location and extent of marginal bone loss; the amount of remaining bone support; the configuration of angular bone defects; the integrity of crestal lamina dura; the root anatomy and presence of root surface defects such as resorption cavities and cemental tears; the proximity of proximal marginal bone to root bifurcations; the presence and extent of furcation bone loss; the proximity of the lesion to adjacent teeth, sinuses and other anatomical structures; and any association with disease of endodontic origin. This information is sought to confirm the diagnosis, assess the prognosis and determine a treatment plan. A detailed review of this subject has been published recently.1 The only radiographic methods with the potential to fulfill all these requirements are periapical views and panoramic views. Periapical radiography provides better image resolution and precision.2 Panoramic radiography, on the other hand, is a rapid and comparatively simple technique with a low patient radiation dose, relative to the number of teeth which form the image. The drawbacks of panoramic radiography include overlapping of adjacent tooth surfaces, superimposition of other anatomical structures and low contrast. Furthermore, although it has been shown that both radiographic methods together identify fewer than 20% of marginal (angular) bone defects, the detection rate from panoramic radiography was inferior to periapical radiography by a factor of x 3.3 Nonetheless, it has been suggested that a panoramic radiograph, when supplemented by periapical radiographs, is adequate for diagnostic purposes.4,5,6 In this regard Molander et al.7 calculated that the number of additional intraoral radiographs necessary for a comprehensive evaluation of the periapical and periodontal bone status ranged from 6.03 to 8.8 depending on which conventional panoramic unit (6 conventional units were evaluated) had been used to obtain the original radiograph. The Scanora dental panorama programme performed slightly better: only 4.83 additional periapical radiographs, on average, were necessary. However, the aim of that study was to determine how many supplementary periapical radiographs were necessary to evaluate all proximal marginal bone crests and all periapical bone. In routine clinical practice this is rarely necessary. Instead, it is accepted good practice to prescribe radiographs only when a clinical examination has been carried out to determine which, if any, parts of the dentition should be radiographed. Following panoramic radiography, therefore, supplementary periapical radiographs need to be taken only for teeth with both an inadequate panoramic image and which were among those initially judged to require a radiographic assessment.
In 1994, it was reported that, when recommended good practice is followed, the 'effective' patient dose for one periapical radiograph is approximately 0.001 mSv and for one panoramic radiograph is 0.007 mSv.8 On this basis, patients requiring fewer than seven periapicals would automatically receive a dose benefit by having periapical radiographs taken rather than a panoramic examination. Likewise, patients requiring more than seven periapicals might receive a dose benefit from a panoramic survey of the dentition instead, although this would depend on the number of supplementary periapicals which were necessary. The purpose of this study, therefore, was to assess the dose reduction, if any, from panoramic radiography, supplemented by periapical radiographs, for a sample of patients who had been referred for periodontal diagnosis and treatment and who had sufficiently widespread advanced disease, according to predetermined clinical criteria, to require at least seven periapical radiographs for proper radiographic assessment.
In addition, since periodontal healing is impaired by concurrent endodontic disease,9 and since periodontal treatment plans for patients with extensive disease cannot be isolated from their endodontic or restorative treatment needs, a thorough examination of the dentition was also carried out to identify those teeth for which dental radiographic assessment was required. This approach, it was felt, would make the study more authentic and its findings more readily applicable to routine clinical practice.
Methods
The study was carried out in the Periodontal and Radiology Departments of Glasgow Dental Hospital and School. Patients were selected from those who had been referred to, and examined at, a consultant-led periodontal clinic. A thorough clinical examination was carried out and all those who were judged to need a radiographic assessment of their periodontal condition, requiring at least seven periapical views, were included in the study. Recruitment was continued until a sample of 50 consecutive cases had been obtained. To be 'eligible' for radiographic examination, each tooth had to exhibit at least one of the following features:
a. Attachment loss ≥ 4mm and pocket depth ≥ 5mm.
OR
b. Horizontal tooth movement ≥ 1mm.
OR
c. Clinical evidence of furcation disease.
In addition, every tooth in the dentition was assessed clinically for periradicular disease, caries and subgingival restoration margin fit. Thus, a radiographic assessment of the periradicular condition was considered desirable for heavily restored or discolored teeth or for teeth with evidence of, or a history of, soft tissue swelling, pain or discharge. Likewise, proximal surface restorations which extended into an inflamed pocket of any depth were judged to require radiographic assessment unless the clinician was able to satisfy himself by probing that the margin was adequate. Finally, a radiographic assessment of caries was judged to be necessary for the further investigation of suspected carious lesions, pain symptoms, discolouration or a leaking restoration.
A chart was produced for each recruited patient showing all teeth present and those for which a periodontal radiographic assessment was required. In addition, teeth requiring radiographic assessment for periradicular disease were marked on the chart. Likewise, those teeth with restorations requiring a radiographic assessment of proximal marginal fit and those teeth requiring a radiographic assessment for caries were marked separately on the chart. All the patients were examined clinically by one author to determine which teeth required a radiographic assessment and for what purpose.
A single panoramic dental radiograph was taken either by a radiographer, or by a supervised undergraduate dental student, according to standard protocols on a Siemens Orthophos panoramic machine. Programme P2 (excluding the condyles and, thereby, reducing irradiation of the parotid glands) was normally selected, and the exposure factors chosen for each individual patient, according to standard procedures.
All the panoramic radiographs were examined by a panel of four examiners, comprising two specialists in periodontics, one specialist in oral radiology and one superintendent radiographer. Each panoramic radiograph was examined independently by each examiner, and, after identifying those teeth for which a radiographic assessment had been judged necessary, the adequacy of the image of every tooth and its bony investment was determined. The four examiners then compared their findings, and consensus scores for each selected tooth were recorded according to majority opinion: in the event of an equal split in examiner opinion, discussion took place between the divided parties until a majority decision was reached.
The panoramic image of each selected tooth was scored by each examiner for periodontal disease, periradicular disease, marginal fit and caries. The panoramic image was judged to be either adequate or inadequate according to the following criteria:
-
1
For teeth requiring periodontal assessment: the mesial and distal bone margins had to be clearly visible together with the approximate location of the associated apex, and the location of the marginal bone had to be reasonably consistent with the recorded pocket depth. Where the roots of a lower molar were clearly divergent, the point of bifurcation had to be clearly visible.
-
2
For teeth suspected of having periradicular disease: the entire periapical bone of each root and the outline of its apex had to be clearly visible, and, if a radiolucent lesion was observed, its origin and extent had to be obvious. Because of the frequency of root perforations in teeth with post crowns, the radiographs of post-crowned teeth were not considered adequate unless the entire periphery of the root was visible.
-
3
For teeth with a potentially ill-fitting restoration: there had to be an un-obscured view of the restoration-tooth interface so that, if present, an overhanging restoration and/or marginal leakage could be detected.
-
4
For teeth possibly affected by caries: image quality had to be sufficiently good to detect the presence and extent of caries.
If the examiner felt that the panoramic image did not meet the above criteria, the panoramic image of the tooth was judged to be inadequate, but only if a periapical radiograph would have been likely to produce a better image. If the panoramic image yielded all the information necessary for diagnosis and treatment planning, it was judged to be adequate even if better image resolution could have been obtained by periapical radiography.
The following data were also calculated by the panel and recorded:
The minimum number of periapicals which would have been necessary to record periodontal conditions for the chosen teeth, had these been obtained instead of a panoramic image.
The minimum number of periapicals which would have been necessary to record periodontal and dental conditions for the chosen teeth, had these been obtained instead of a panoramic image.
The minimum number of additional periapicals for adequate diagnosis of periodontal conditions, after the adequacy of the panoramic view had been determined.
The minimum number of additional periapicals for adequate diagnosis of periodontal and dental conditions, after the adequacy of the panoramic view had been determined.
Prior to commencing the study, the examiners carried out mock assessments of a number of panoramic radiographs and met to compare their findings. These sessions were used to share their collective knowledge of dental radiographic technique and interpretation, and to confirm that the scoring criteria were understood and correctly followed.
To measure the reproducibility of the assessment process, after all the assessments were completed, five panoramic radiographs were selected at random from the sample of 50 cases, and each examiner carried out a further series of assessments, blind to the original scores.
Results
All teeth selected for radiographic assessment of their periodontal conditions (qualifying teeth) were affected by pockets ≥5 mm deep and attachment loss ≥4 mm. This included all teeth with clinical evidence of furcation disease and all teeth exhibiting horizontal movement ≥1 mm.
Panoramic radiographs were obtained from 50 patients (17 males, 33 females), 27 to 73 years old with an average age of 45 ± 10 (sd) years. Table 1 shows the number of teeth per patient, the number of qualifying teeth per patient and the pocket depths of qualifying teeth.
Table 2 shows that, if intraoral rather than panoramic radiography had been employed, between seven and 12 periapical radiographs per patient would have been the minimum number required for complete diagnosis: a mean of 8.68 periapicals per patient for periodontal diagnosis; and a mean of 8.92 periapicals per patient for complete periodontal and dental diagnosis.
A total of 951 teeth were assessed for periodontal disease, 430 for periradicular disease, 90 for marginal fit of restorations and 165 for caries.
Table 3 shows the extent of inter-examiner agreement. Thus, for periodontal diagnosis all four examiners were in agreement on 453 (47.6%) occasions, three examiners agreed on 369 (38.8%) occasions and there was an equal split on 129 (13.6%) occasions. When considering whether the radiographic image was adequate for diagnosis of periradicular disease, marginal restoration fit and caries, slightly higher levels of agreement were obtained.
Table 4 shows the responses of each examiner, the consensus responses and the proportion of times that each examiner's response matched the consensus response. For example, examiner 1, in judging the adequacy of the panoramic image for periodontal diagnosis, recorded 'Yes' 576 times, and 'No' 375 times making a total of 951 responses of which 86.1% matched the consensus response.
Table 4 also shows that the consensus finding for periodontal diagnosis was 'Yes' 552 times, and 'No' 399 times, giving a percentage adequacy of 60.6%. By comparison, the percentage adequacy of panoramic radiography for diagnosis of periradicular conditions was 61.4% (264Y, 166N), the marginal fit of restorations 55.6% (50Y, 40N) and caries 45.5% (75Y, 90N).
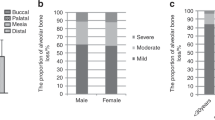
There were marked between-tooth differences in the adequacy of the panoramic image for periodontal diagnosis. Thus Figure 1 shows how often an assessment of the panoramic image was successful (or judged adequate) for periodontal diagnosis of the different tooth types. In the lower jaw, success rates varied from 58.6% for canines to 94.3% for second molars. In the upper jaw, success rates varied from 9.2% for first premolars to 71% for first incisors. Success rates for mandibular teeth were, with one exception, higher than for the corresponding maxillary teeth: the success rate for mandibular first incisors was marginally lower than for the corresponding maxillary tooth.
Figure 2 shows a similar pattern of diagnostic adequacy with respect to peri-radicular conditions with success rates much higher for mandibular teeth (33.3% – 100%) than maxillary teeth (17.5% – 64.4%)
Too few teeth were assessed for caries and marginal fit of restorations for meaningful comparisons to be made between different tooth types.
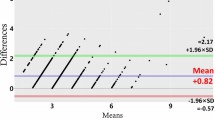
The number of additional periapical radiographs required ranged from 0 to 8 (mean = 4.3 ± 1.7 sd) for periodontal diagnosis, and from 1 to 8 (mean = 5.1 ± 1.5 sd) for dental and periodontal diagnosis. The main purpose of the study was to compare the effective dose from panoramic radiography, supplemented where necessary by periapicals, with the effective dose from periapical radiography of all the selected teeth, had that approach been taken instead. Using the figures published in the 1994 Guidelines,8 the effective doses would be 0.001 mSv from each periapical radiograph and 0.007 mSv from one panoramic radiograph. The dose to each patient was then calculated by adding the dose from the additional periapical exposures to the dose from the panoramic exposure. Thus effective doses ranged from 0.007 mSv for the one patient who did not require any additional periapical exposures to 0.015 mSv for the patients who required eight additional periapical exposures. By also calculating the effective dose to each patient from a series of periapicals of all the selected teeth, it was possible by subtraction to determine which radiographic approach delivered the smaller dose to each patient. These differences are shown in the form of a frequency distribution of patients in Table 5 which demonstrates that the panoramic-plus-periapicals approach, when employed purely for periodontal diagnosis, achieved an effective dose reduction in only three (6%) patients, amounting to 0.001 – 0.002 mSv, and an effective dose equivalent to the periapicals-only approach in a further four (8%) patients. The panoramic-plus-periapicals approach delivered an additional effective dose to the remaining 43 (86%) patients amounting to 0.001 – 0.007 mSv. When employed for periodontal and dental diagnosis, the panoramic-plus-periapicals approach achieved an effective dose advantage of 0.001 mSv for only one patient and an equivalent effective dose for three further patients.
Each examiner carried out a total of 95 repeat periodontal assessments on five panoramic radiographs after which the panel convened to determine its consensus response, reaching the same decision on 86 (90.5%) occasions. Using the same five panoramic radiographs, 45 repeat periradicular assessments were made with 82.2% reproducibility, four marginal fit assessments with 100% reproducibility and six caries assessments also with 100% reproducibility.
Discussion
All the patients included in this study had severe and widespread periodontal disease with at least 11 teeth affected by pockets at least 5 mm deep. All these teeth were scheduled for radiographic assessment for which at least seven periapical exposures would have been necessary had intraoral radiography been the only means available. In confirming the minimum number of periapical radiographs which would have been required for a complete periodontal assessment of all the selected teeth, the panel of examiners had to rely on the panoramic radiographs for evidence of tooth position. The same procedure was applied, after examining the panoramic radiographs to calculate the required minimum number of supplementary periapical exposures. It was acknowledged that the actual number required, both for a periapicals-only and a panoramic-plus-periapicals approach, would, in some cases, inevitably exceed the minimum number estimate.
No attempt was made to 'calibrate' the examiners. However, examiner training was carried out to make sure that the examiners understood and agreed upon the assessment criteria. In spite of this, all four examiners were in unanimous agreement on fewer than half of the 951 periodontal assessments. This reflects the nature of the task — a value judgment on the adequacy of panoramic images to reveal predetermined diagnostic features. The validity of the consensus decisions which were made rests on the fact that the panel was chosen to reflect a wide range of expert opinion both within the specialty of periodontology and the specialty of radiology. In making their independent assessments, three examiners demonstrated 85.7%, 86.1% and 87.3% agreement, respectively, with the consensus decisions. Seventy-five percent of the other examiner's assessments matched the consensus decisions. From Table 4, it can be seen that, among the four examiners, this examiner was more readily satisfied with the panoramic images. The methodology is also vindicated by the high level of reproducibility of consensus decisions: repeat assessments of a random sample of five panoramic radiographs yielding the same outcome for 90.5% of teeth.
The quality of the image produced by panoramic radiography varied in different parts of the dentition, an adequate image being obtained most frequently for mandibular first and second molars and least frequently for maxillary canines and first premolars, which were often affected by overlapping. This pattern is in accordance with previous reports.10,11
In this study, after selecting which teeth required radiographic investigation, the employment of a panoramic exposure, followed by additional periapicals, would have resulted in a lower effective dose for only 6% of the sample and the dose advantage for these patients amounted to only 0.002 mSv or less. Eighty-six per cent of the sample would have received a higher effective dose amounting to 0.001 - 0.007 mSv.
The findings of this study are based on the 'average' effective doses, publicised by the National Radiological Protection Board8 and clearly need to be interpreted on this basis. Furthermore, these doses are applicable only to periapical radiographs taken with a 70 kV set, a 200 mm focal spot to skin distance, with rectangular collimation and E speed film, and only to panoramic radiographs with rare earth intensifying screens. No attempt was made to obtain precise effective doses for the equipment and exposure factors actually used or the parts of the dentition irradiated, since complex calculations would have been required, for which no definitive data were available. A review of experimental work already published reveals a range of dose estimates both for panoramic and periapical radiography. These doses are in the same order of magnitude as the reference doses used in the present study but variations exist according to the specific experimental conditions. For example, Lecomber et al.12 published figures derived from the Siemens Orthophos panoramic machine, having investigated all available programmes. Thus, the programme used in our study, P2, delivered 0.0045 mSv when salivary glands were excluded from the calculation and 0.0074 mSv when included. Recently Gijbels et al.13 demonstrated that the effective dose for one periapical radiograph of the mandibular dentition ranged from 0.0005 – 0.0006 mSv when salivary glands were excluded from the calculation and amounted to 0.0007 mSv within anterior segments, 0.0009 mSv within canine and premolar segments but 0.003 mSv within molar segments when salivary tissue was included. The periapical radiographs were taken according to the good practice principles described above by the National Radiological Protection Board8 (the same variables used in our unit).
In addition to the 951 teeth, affected by severe periodontal disease and subjected to radiographic examination, assessment of periapical condition, marginal restoration fit and caries was judged to be necessary for 430, 90 and 165 teeth respectively. By including the requirement for adequate radiographic images of certain teeth for dental reasons, the number of supplementary periapicals judged necessary increased to a mean of 5.1 from the mean of 4.3 which were required for adequate periodontal diagnosis. Had periapical radiography been the sole means of assessment, a mean of 8.92 radiographs would have been required for complete periodontal and dental diagnosis compared to 8.68 for periodontal diagnosis alone. By adding the requirement for adequate diagnosis of dental conditions of selected teeth to that of periodontal conditions, the panoramic-plus-periapicals approach delivered an apparent dose advantage for only one patient of only 0.001 mSv.
Conclusions
An expert panel has recently acknowledged that there is insufficient evidence from research into radiographic selection criteria of the periodontal tissues to make robust, evidence-based recommendations.4 Nevertheless, the panel expressed the view that, if available, a panoramic radiograph of optimal quality may offer a dose advantage over large numbers of intra-oral radiographs, particularly if there are concurrent problems for which radiography is indicated, citing, as examples, multiple existing crowns/heavily restored teeth and/or multiple endodontically treated teeth: supplementary radiographs to be taken at selected sites where the panoramic radiograph provided insufficient fine detail. The present study demonstrates that contrary to the outcome expected from this guideline, the need to supplement panoramic radiographs with intraoral exposures will nearly always result in a greater radiation dose than that arising from periapical radiography of all the affected teeth. This applies even more to heavily restored and caries prone dentitions.
Although it is much easier and much quicker to take a panoramic radiograph than multiple periapical radiographs, the practice of processing then examining the panoramic image, and then taking the supplementary periapical radiographs, will reduce the time advantage of panoramic radiography over intraoral radiography. Since periapical radiographs also have much better image quality2,4 and will identify three times as many periodontal bone defects,3 it is difficult to justify the use of panoramic radiographs for investigation of periodontal disease. They are even harder to justify when a radiographic assessment of dental conditions is also required.
It should be noted that these observations apply only to conventional radiography. A radiation dose reduction of x 0.25 – 0.5 is considered to be obtainable from intraoral digital radiography compared to conventional intraoral film radiography. The dose resulting from panoramic radiography is reduced only when an extra-oral charge-coupled device (CCD) is used but digital storage phosphor systems give rise to similar doses as conventional films. Thus the panoramic-plus-periapicals approach is likely to become even harder to justify as digital radiography becomes more widely available.
These conclusions are based on the assumption that panoramic and periapical radiographs result in typical effective doses of 0.007 mSv and 0.001 mSv respectively. As referred to in the discussion section above, different machines and programmes may give rise to different doses, which could influence the application of radiographic selection criteria locally. Nevertheless, the study methodology is widely applicable to a variety of radiographic techniques and equipment and could be used to help provide an evidence base for radiographic selection criteria.
References
Tugnait A, Clerehugh V, Hirschmann PN . The usefulness of radiographs in diagnosis and management of periodontal diseases: a review. J Dent 2000; 28: 219–226.
Åkesson L, Håkansson J, Rohlin M . Comparison of panoramic and intraoral radiography and pocket probing for the measurement of alveolar bone level. J Clin Periodontol; 1992 19: 326–232.
Pepelassi E A, Tsiklakis K, Diamanti-Kipioti, A . Radiographic detection and assessment of the periodontal endosseous defects. J Clin Periodontol 2000; 27: 224–230.
Faculty of General Dental Practitioners (UK). Radiographs in periodontal assessment. In Selection criteria for dental radiography. pp42–44. London: Royal College of Surgeons, 1998.
Åkesson L, Rohlin Håkansson, J . Marginal bone in periodontal disease: an evaluation of image quality in panoramic and intraoral radiography. Dentomaxillofacial Radiol 1989; 18: 105–112.
Hirschmann PN . Radiographic interpretation of chronic periodontitis. Int Dent J 1987; 37: 3–7.
Molander B, Ahlqwist M, Gröndahl H-G . Image quality in panoramic radiography. Dentomaxillofacial Radiol 1995; 24: 17–22.
National Radiological Protection Board. Guidelines on radiology standards for primary dental care. London: department of Health, 1994, Doc NRPB 5 (3).
Jansson L, Ehnevid H, Lindskog S, Blomlöf L . Relationship between periapical and periodontal status. A clinical retrospective study. J Clin Periodontol 1993; 20: 117–123.
Bjorn H, Holmberg K . Radiographic determination of periodontal bone destruction in epidemiological research. Odont Revy 1966; 17: 232–250.
Jenkins WMM, Mason WN . Radiographic assessment of periodontitis: a study of 800 unreferred patients. Br Dent J 1984; 156: 170–174.
Lecomber A R, Downes S L, Mokhtari M, Faulkner, K . Optimisation of patient doses in programmable dental panoramic radiography. Dentomaxillofacial Radiol 2000; 29: 107–112.
Gijbels F, Jacobs R, Sandering G, De Smet E, Nowak B, Van Dam J, Van Steenberghe D . A comparison of the effective dose from scanography with periapical radiography. Dentomaxillofacial Radiol 2002; 31: 159–163.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Jenkins, W., Brocklebank, L., Winning, S. et al. A comparison of two radiographic assessment protocols for patients with periodontal disease. Br Dent J 198, 565–569 (2005). https://doi.org/10.1038/sj.bdj.4812304
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4812304