Key Points
-
Within the limits of this investigation, it can be concluded that marginal accuracy of pressed all-ceramic FPD and the conventional MC techniques used are on a similar level.
-
In particular, almost all marginal gap values observed in this study were in the range of 50-100 μm, which is ideal for composite cement and seems to optimise performance.
-
The process of cementation reduces the marginal accuracy of FPD restorations irrespective of the FPD material.
-
After artificial aging marginal degradation of cement films was not significant using a resin-cement and dentine-bonding system for cementing the all-ceramic FPD. Therefore, the investigators judged resin-cements as the most suitable for cementing all-ceramic restorations.
Abstract
Purpose This study compares the marginal accuracy of posterior metal ceramic (MC), all-ceramic IPS Empress®2 and experimental pressed ceramic (EPC-VP 1989/4) three-unit fixed partial dentures (FPD), before and after luting and after thermo-mechanical fatigue in a dual-axis chewing simulator.
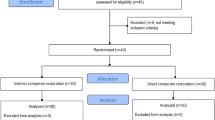
Materials and methods Caries-free human teeth (n=160) were used as abutments for the fabrication of eighty posterior three-unit FPD, divided into two test-groups, IPS Empress®2 and EPC, of 32 samples each and one control group of 16 samples metal ceramic FPD. All FPD were cemented with Variolink®II dual-curing resin cement. Half of the samples in each group were exposed to a dual-axis chewing simulator.
Results The geometric mean marginal gap values (μm, before cementation, after cementation and after thermo-mechanical fatigue) amounted to 53, 63 and 62 for the ceramic metal FPD, 57, 71 and 68 for the Empress®2 FPD and 55, 67 and 68 for the EPC FPD. In all groups a statistically significant increase in marginal gap width was observed after cementation. The effect of functional loading in the chewing simulator on marginal gap was not significant. Marginal gap was lowest in the control group but differences with all-ceramic materials were small in all evaluation stages.
Conclusion Within the limits of this investigation, it can be concluded that marginal gap values of these all-ceramic materials and conventional MC techniques are on a similar level. In particular, almost all marginal gap values observed in this study were within the limits of clinical acceptance.
Similar content being viewed by others
Introduction
The use of all-ceramic materials for fixed restorations has become a key topic in aesthetically oriented dentistry. The effect on pulpal and periodontal tissues, marginal seal, fracture resistance and aesthetics are important criteria for the long-term success of all-ceramic crowns.1 The marginal fit of all-ceramic crowns has been the focus of various investigations.2,3,4,5 The extent of misfit of dental restorations is closely associated with the development of secondary caries and periodontitis.6,7,8 Misfit in all-ceramic crowns can also affect their fracture strength9 and thus reduce longevity. Today there are ceramic systems available (In-Ceram®, Vita Zahnfabrik GmbH; Empress®2, Ivoclar-Vivadent AG; Cerec®, Sirona Dental Systems GmbH; Procera AllCeram®, Nobel Biocare etc.), which allow a single tooth all-ceramic restoration with clinically acceptable marginal accuracy.4,5,10,11 Because of an improved high fracture resistance of these ceramics, even posterior teeth could be restored by all-ceramic single crown restorations. The clinical use of all-ceramic FPD even used in the posterior region is still a challenge in dentistry. Data about the marginal fit of all-ceramic FPD are very rare. In the late 1980s, In-Ceram® was introduced based on the principle of the two 3-dimensionally infiltrating phases, aluminum oxide and a sodium lanthanum glass. A recent study showed that In-Ceram® can be used successfully for anterior FPD.12 The marginal fit of In-Ceram® all-ceramic crowns and FPD were similar to metal-ceramic restorations.10
Empress®2, which was introduced to the market in 1998, is a lithium-silicate based glass ceramic using the hot pressing procedure. It was indicated for three-unit FPD up to the first premolar.13,14 In-vitro, the mean fitting accuracy of Empress®2 all-ceramic posterior crowns amounted to less than 50 μm.15 A glass-infiltrated zirconia/alumina-based ceramic material (In-Ceram Zirconia®, Vita Zahnfabrik GmbH) has been developed for the fabrication of posterior crowns and three-unit FPD. Laboratory investigations could show a mean margin width of 73 μm.15 Machining (CAD/CAM) has become a viable option in the manufacturing of all-ceramic restorations.
Restorations fabricated by the Procera AllCeram® system are composed of a densely sintered, high-purity aluminum oxide coping that is veneered with low-fusing AllCeram® porcelain.16 A 5 to 10.5 years clinical investigation indicated a good prognosis for Procera® all-ceramic crowns.17 An evaluation of the clinical fit of Procera AllCeram® crowns amounted to medians of mean marginal gap widths between 90 μm and 145 μm in posterior teeth.5 The Digitising Computer System (DCS Production AG, Allschil, CH) has been designed for the computer-controlled machining of titanium or ceramic frameworks of ceramic-veneered single crowns and bridge restorations. Tinschert et al.18 evaluated the marginal fit of alumina- and zirconia-based FPD machined by the DCS System and exhibited a mean marginal discrepancy of approximately 65 μm. So far there is no clinical data about the Procera AllCeram® and the DCS all-ceramic FPD available.
Although machining seems to be a trend in constructing all-ceramic restorations, established press ceramic systems have also undergone improvements. On the basis of the Empress®2 lithium glass-ceramic material, the Ivoclar-Vivadent Company developed an experimental pressed ceramic (EPC) system. According to the manufacturer, a different fabrication process of the ceramic ingots leads to improved physical properties, a higher translucency and a higher flexural strength (525 ± 75 (SD) MPa) of EPC.
The aim of the present investigation was to evaluate the marginal discrepancies of all-ceramic three-unit Empress®2 FPD and all-ceramic three-unit EPC FPD before and after luting, and after thermo-mechanical fatigue in a dual axis chewing simulator and to compare the results with metal ceramic (MC) FPD.
Materials and Methods
Eighty caries-free human lower molars and eighty premolars, which were stored in 0.1% thymol solution at room temperature after extraction,19 were used as abutment teeth for three-unit FPD. Calculus deposits and/or soft tissue remnants were removed using a hand scaler. Pairs of premolar and molar teeth were randomly assigned into one control group of sixteen samples and two test groups of 32 samples each. A representative clinical model with a missing first molar was selected. The mesiodistal width of the pontic used in the present study was 11 mm. The selected model was embedded using a silicone putty material (Optosil®, Heraeus-Kulzer, Wehrheim, D). The occlusal table of the model was set parallel to the horizontal plane. Afterwards, a silicone mould of this representative model was fabricated with a polysiloxane impression material (Permagum® Putty Soft, 3M-ESPE, Seefeld, D). This silicone mould was then used as the negative form for fixing all abutment teeth in the sample holder. In order to imitate the physiological tooth mobility, all roots of the abutment teeth were covered with an artificial periodontal membrane made out of gum resin (thickness 0.5 mm) (Anti-Rutsch Lack®, Wenko-Wenselaar, Hilden, D). The natural teeth were fixed into the silicone mould and self-curing polyester resin (Technovit 4000®, Heraeus-Kulzer, Wehrheim, D) was poured into the sample holder. The teeth were embedded until 2 mm below the cemento-enamel junction to simulate the bone level. In order to receive occlusal forces in an axial direction, the teeth were fixed into the resin material without any bucco-lingual and mesio-distal inclination. All abutment teeth were prepared manually to 6° convergence, 6 mm abutment height for premolars, 4.5 mm abutment height for molars, and a 1.2 mm circular 90° butt shoulder with a rounded inner angle. The preparation followed a standardised preparation protocol and was controlled by a siloxane preparation mould. For the preparations, appropriate diamonds were used (No 386.023, No 8368.023, No 837KR.0.12, No 8837KR.0.12, Gebr. Brasseler, Lemgo, D). After being prepared and dried, impressions of the abutment teeth were taken with a polyvinyl-siloxane impression material (Dimension® Garant L and Permagum® Putty Soft, 3M-ESPE, Seefeld, D). A cast of each impression was poured with Fuji® rock-type 4 dental stone (GC, Tokyo, J).
Three groups of three-unit FPD were fabricated on master dies with detachable segments: group A (control) — 16 metal ceramic (MC) FPD, group B (test 1) — 32 Empress®2 FPD, and group C (test 2) — 32 EPC FPD. Both, IPS Empress®2 and the EPC (VP 1989/4) are lithium disilicate glass-ceramics and the chemical basis for the materials is the SiO2–Li2O system. The elongated crystals measuring 0.5 – 4 μm in length represent the main crystal phase of lithium disilicate and lithium orthophosphate. This main crystal phase is developed from the base glass according to the principles of controlled crystallisation. This procedure was used to fabricate the glass-ceramic ingots of Empress®2 and EPC. In addition, the microstructure also contains lithium orthophosphate crystals (Li3PO4).
To form the dental FPD, the Empress®2 and EPC glass-ceramic ingots were processed in the Empress EP 500 hot-press furnace (Ivoclar-Vivadent AG, Schaan, FL) at 920°C. The all-ceramic FPD were fabricated according to the manufacturer's recommendations. The framework connector height amounted to 4 mm, the connector width to 4 mm and wall thickness to 0.8 mm. Two glaze firings were performed in a Programat P 100 furnace (Ivoclar-Vivadent AG, Schaan, FL), using a special glazing paste (Batch A24747) and liquid (Batch B29605). The inner surfaces of the retainers were etched with 4.9% hydrofluoric acid (ceramic etchant, Ivoclar-Vivadent AG, Schaan, FL) for 20 seconds and then silanised with Monobond-S® (Ivoclar-Vivadent AG, Schaan, FL). A high-precious alloy was used for the fabrication of the MC FPD (Metalor V-Classic®, Metaux precieux, Metalor Deutschland GmbH, Stuttgart, D). The thickness of the frameworks was 0.4 mm and the dimensions of the connectors amounted to 3 × 1.5 mm (width × height). The frameworks were veneered with feldspathic porcelain (Vita Omega® Ceramic, Vita Zahnfabrik, Bad Sckingen, D). The FPD were cleaned in an ultrasonic bath for 2 minutes and in 96% alcohol. Their inner surfaces were sandblasted with Rocatec® Pre (3M-ESPE, Seefeld, D) (110 μm aluminium oxide), silicated with silica-modified aluminum oxide (Rocatec® Plus) and then silanised with a silan (3M-ESPE sil®). Before cementation, all abutment teeth were initially etched with 37% phosphoric acid (Total Etch®, Ivoclar-Vivadent AG, Schaan, FL) for 20 seconds (dentine) or 60 seconds (enamel) (total etch technique). Syntac® primer (Ivoclar-Vivadent AG, Schaan, FL) was applied for 15 seconds and subsequently Syntac® adhesive for 10 seconds. The last step consisted of the application of Heliobond® (Ivoclar-Vivadent AG, Schaan, FL) including light-curing. All FPD, test and control group(s) were cemented adhesively with Variolink®II dual-curing resin cement (Ivoclar-Vivadent AG, Schaan, FL) (Fig. 1). This cementation procedure was even used for the MC FPD to produce comparable results.
The FPD were placed on the abutment teeth with maximum pressure of 10 N. Excess cement was removed with soft pellets, and glycerine gel was applied in the marginal area. The margins of the MC FPD and all surfaces of the all-ceramic retainers were light-cured for one minute mesially, distally, lingually, buccally, and occlusally. Excess polymerised composite was removed with a scalpel and a fine finishing diamond. Then, half of the specimens of the three groups were artificially aged in a computer controlled dual axis chewing simulator (Willytec, Munich, D)20 (Fig. 2).
Schematic drawing for one chewing chamber from Kern et al.20
To simulate a long-term service time of 5 years, as was performed in this study, about 1,200,000 'masticatory' cycles had to be performed in the chewing simulator. The effective weight of each antagonistic sample was 5 kg, which corresponds to a loading force of 49 N.21 The load was applied in the centre of the occlusal surface of the bridge pontic using a 6 mm diameter ceramic antagonist ball (Steatit®). The masticator load curve was programmed by the combination of horizontal (0.5 mm) and vertical (6 mm) motion. The computer unit controls the water flow of the cold (5°C) and warm (55°C) water baths for thermal cycling of the samples, each for 60 seconds with an intermediate pause of 12 seconds.
Replicas of all samples representing the marginal areas were fabricated in all three stages (before cementation, after cementation and after artificial aging). Impressions of the samples were therefore taken with a polyvinyl-siloxane impression material (Dimension® Garant L and Permagum® Putty Soft, 3M-ESPE, Seefeld, D) and were poured with an epoxy resin (Epon® 812, Fluka-Chemika, Neu-Ulm, D). The epoxy replicas were mounted on aluminium stubs and coated with 200 Å of gold using vacuum evaporator (SCD 050, Balzers Union, Balzers, FL). The epoxy replicas were analysed with the help of a stereomicroscope (Zeiss, Oberkochen, D). A 3 CCD camera (Sony, Köln, D) was mounted to the microscope and connected to a personal computer. The marginal area of each replica was oriented perpendicularly and orthoradially on the computer monitor. The video image of the marginal gap (× 200 magnification) was examined by using a special evaluation software (Analysis® 3.0, Soft-Imaging Software GmbH, Münster, D). After the first measurements, the replica was moved until the next section of the marginal area came into view. To do so, a special micro mechanical device had to be employed. Areas where the crown margin or the finishing line of the preparation could not be precisely detected were excluded from the evaluation. In total, 250-300 single measurements were performed of a single crown margin circumference.
For each abutment tooth the mean of all single measurements was used for statistical inference. Summary measures were then calculated for assessment of marginal gap of all teeth in each group. The geometric mean was used as a measure of marginal gap separately for each group and for each of the three stages, before cementation, after cementation, and after simulation in the artificial mouth. The geometric mean accounts for skewness in the data and is thus more robust than the ordinary mean of the marginal gap values. Estimates are supplemented with corresponding 95% confidence intervals. To test for differences of marginal accuracy, the t-test was applied to the log-transformed marginal gap values.
Results
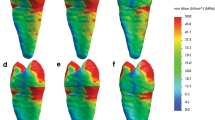
Summary statistics of marginal accuracy in all groups are shown in Table 1. The geometric mean marginal gap values (μm, and associated 95% confidence intervals - CI, before cementation, after cementation and after thermo-mechanical fatigue) amounted to 52.9 [50.1; 55.8], 62.7 [59.0; 66.7] and 61.8 [57.3; 66.7] for the MC FPD, 56.8 [53.9; 59.8], 70.8 [67.5; 74.2] and 67.6 [61.2; 74.6] for the Empress®2 FPD and 54.6 [52.7; 56.6], 67.1 [64.8; 69.5] and 68.3 [64.0; 73.0] for the EPC FPD. Figure 3. shows geometrical means of marginal accuracy together with 95% confidence intervals. The marginal accuracy of the control group was not significantly higher compared with both test groups at the initial stage and after thermo-mechanical fatigue. The marginal gap values of the metal ceramic FDP were significantly lower only in the stage after cementation (MC versus Empress®2 FPD: p=0.003, MC versus EPC: p=0.04).
The marginal accuracy in all groups increased significantly after the cementation procedure (p <0.0001 in all groups). Artificial aging marginal gap values were not clearly distinct from the measurements after cementation (p > 0.05 in all groups).
Discussion
Along with several factors, marginal accuracy is an important criterion of the quality of fixed partial dentures.1,6,8,9,22 Clinical studies are time consuming and in addition, it is often difficult to standardise the test parameters.20 Therefore, long-term results regarding the marginal fit can be obtained by in vitro tests. The results obtained after 240,000 to 250,000 'masticatory' cycles in a chewing simulator corresponded to the results obtained after one year of clinical service.23,24 Thus the number of cycles used in the present study could be proportioned to 5 years of service. A force of 49 N was applied during the aging test, thus reflecting normal occlusion and chewing forces for posterior teeth.25,26
In the present study, natural extracted human mandibular molars and premolars were used as abutments. Natural teeth could show a large variation. A controlled selection of comparable abutment teeth was fundamental for this kind of in vitro study. Several authors have employed artificial dies made of steel3,27,28 or resin2,10,11,22,29,30 to measure the marginal accuracy. However, abutments made of steel or resin give neither real information about the microstructure of the hard tissue of teeth after preparation nor about the micro- and chemo-mechanical adaptation of the luting material to the dentin. The 90° angled shoulder preparation used has been recommended and tested by several authors with successful results.2,27,29,30,31 Most authors agreed that preference should be given to rounded axiogingival line angles.27,32 The main advantage of using artificial abutments is the possibility to make a standardised preparation easier.
The microscopic analysis has been performed with a stereomicroscope (Zeiss, Oberkochen, D) with 200 times magnification. The kind of microscopes and magnifications used by investigators for the evaluation of marginal adaptation varies considerably. Digital microscopes, stereomicroscopes, light microscopes and electron microscopes have been used with various magnifications.2,3,4,5,10,22,27,29,30,33,34,35,36 According to Groten et al.28 approximately 50 measurements along the margin of a crown yield clinically relevant information. A consistent estimate for the gap size with an overall impact on the measurement error was typically in a range of ± 8μm (SD). In the present study 250-300 measurements were made along the complete margin of each abutment. This number is enough to give a consistent estimate for the gap size.28
In the present study the impression replica technique was chosen for the evaluation of marginal accuracy. This method allows long-term studies because sacrificing of samples is not required. However, this technique does not provide any information regarding the disintegration and micro leakage of the cement film.
The marginal fit of different crown systems has been extensively studied.2,3,4,5 Before cementation, the MC FPD presented a marginal discrepancy (geometric mean) of 53 μm, the Empress®2 FPD 57 μm and the EPC FPD 55 μm. Considering a clinically acceptable range for marginal gap of 50 and 100 μm,37,38,39 almost all restorations presented clinically acceptable marginal accuracy. Only few restorations, all of them belonging to the Empress®2 group, showed unacceptable high marginal gap values. However, the 75% of the values of marginal discrepancy in the Empress®2 group were lower than 64 μm before cementation. The geo-mean marginal gap value of 53 μm observed for the MC restorations in the present study is smaller compared with the value of 64 μm obtained by Beschnidt and Strub,4 who also investigated marginal discrepancy of MC crowns before cementation. Belser et al.40 reported a mean gap of 33 μm for MC crowns before cementation. In the present study, the marginal discrepancy of the all-ceramic FPD before cementation has similar marginal fidelity as has been reported by Beschnidt and Strub4 for IPS Empress® crowns layering technique, IPS Empress® crowns staining technique and conventional In-Ceram crowns. According to the latter study, the Celay® feldspathic crowns and the Celay® In-Ceram crowns produce higher values of mean marginal discrepancy.
By minimising the degree of marginal opening, the surface of exposed cement will be decreased, thus reducing the rate of dissolution of cement that occurs in oral fluids.41,42 Marginal degradation of cement films is an often diagnosed clinical drawback. Buchalla et al.43 reported that resin cements are more resistant to wear both in neutral and acidic conditions in relation to carboxylate, glass ionomer, resin modified glass ionomer, polyacid modified resin composite and zinc phosphate cements. When comparing the fracture strength of all-ceramic crowns, between regularly bonded crowns and adhesively luted crowns, other authors34,44 found luted crowns showed more resistance to breakage. Therefore, the investigators judged resin-cements as the most suitable for cementing all-ceramic restorations. For comparable results dual-curing resin cement was used for the adhesive luting of all restorations, with the bond being mediated by the use of a dentin-bonding system and a micro mechanically retentive ceramic or metal surface. The mode of pre-treatment of both the tooth and the restoration surface is an important factor for the marginal seal.45
For resin cements, thicker cement layers produce better bond strength values. Molin et al.37 examined four point bending strength of ceramic-cement-ceramic sandwiches with differing cement layer thickness (20 μm, 50 μm, 100 μm and 200 μm). The cement layers were light cured. The bond strengths were significantly lower in the 20 μm thick films than in the thicker ones. The investigators concluded that taking into account the physical and clinical properties of resin based luting agents, a marginal gap in the scale of 50-100 μm is ideal for composite cement and seems to optimise performance. In the present study all marginal gap values obtained are within the above mentioned limits.
The paired t-test showed a significant increase of the marginal discrepancies in all test groups after cementation. The increase of marginal discrepancy observed after cementation can be explained by the film thickness of the cement used.
Some researchers focused on investigating the film thickness of the various available cements. Belser et al.40 reported increases in marginal discrepancy between 12 and 21μm for zinc phosphate cements. Alkumru et al.46 showed that crowns luted with composite have a 2.5 times smaller marginal discrepancy than crowns, which were cemented with zinc phosphate cement. These findings are in accordance with findings of other investigators.47,48
However, in relation to other studies, lower values of increase in marginal discrepancy after cementation have been found in the present study.4,40,47,48
In this investigation, slightly lower marginal gap values after artificial aging were found. This can be explained by considering that after artificial aging, a certain degree of degradation of the cement film is occurring according to the literature.43,49,50 Some microns of the cement film might have been washed out during the aging procedure leading to a clearer image and created the possibility for more precise measurements of the marginal gap. Only micro leakage analysis can supply information about the density of the cement seal. As mentioned before, the design of the present study did not offer the possibility to evaluate marginal degradation and micro leakage. More scientific data of the marginal accuracy of all-ceramic FPD must be generated under clinical conditions.
Conclusion
Within the limits of this investigation, it can be concluded that marginal accuracy of all-ceramic Empress®2, EPC FPD and the use of conventional MC techniques is on a similar level. In particular, almost all marginal gap values observed in this study were within the limits of clinical acceptance. The process of cementation reduces the marginal accuracy of FPD restorations irrespective of the FPD material.
References
Burke FJ, Qualtrough AJ, Wilson NH . A retrospective evaluation of a series of dentin-bonded ceramic crowns. Quintessence Int 1998; 29: 103–106.
Weaver JD, Johnson GH, Bales DJ . Marginal adaptation of castable ceramic crowns. J Prosthet Dent 1991; 66: 747–753.
Sulaiman F, Chai J, Jameson LM, Wozniak WT . A comparison of the marginal fit of In-Ceram, IPS Empress, and Procera crowns. Int J Prosthodont 1997; 10: 478–484.
Beschnidt SM, Strub JR . Evaluation of the marginal accuracy of different all-ceramic crown systems after simulation in the artificial mouth. J Oral Rehabil 1999; 26: 582–593.
Boening KW, Wolf BH, Schmidt AE, Kastner K, Walter MH . Clinical fit of Procera AllCeram crowns. J Prosthet Dent 2000; 84: 419–424.
Gardner FM . Margins of complete crowns — literature review. J Prosthet Dent 1982; 48: 396–400.
Lang NP, Kiel RA, Anderhalden K . Clinical and microbiological effects of subgingival restorations with overhanging or clinically perfect margins. J Clin Periodontol 1983; 10: 563–578.
Knoernschild KL, Campbell SD . Periodontal tissue responses after insertion of artificial crowns and fixed partial dentures. J Prosthet Dent 2000; 84: 492–498.
Tuntiprawon M, Wilson PR . The effect of cement thickness on the fracture strength of all-ceramic crowns. Aust Dent J 1995; 40: 17–21.
Kappert HF, Altvater A . [Field study on the accuracy of fit and the marginal seal of In-Ceram crowns and bridges]. Dtsch Zahnarztl Z 1991; 46: 151–153.
May KB, Russell MM, Razzoog ME, Lang BR . Precision of fit: the Procera AllCeram crown. J Prosthet Dent 1998; 80: 394–404.
Sorensen JA, Kang SK, Torres TJ, Knode H . In-Ceram fixed partial dentures: three-year clinical trials. J Calif Dent Assoc 1998; 26: 207–214.
Chitmongkolsuk S, Heydecke G, Stappert CFJ, Strub JR . Fracture strength of all-ceramic lithium disilikate and porcelain-fused-to-metal bridges for molar replacement after dynamic loading. Eur J Prosthodont Restor Dent 2002; 10: 131–138.
Sorensen JA, Cruz M, Mito WT, Raffeiner O, Meredith HR, Foser HP : A clinical investigation on three-unit fixed partial dentures fabricated with lithium disilicate glass-ceramic. Pract Periodontics Aesthet Dent 1999;11: 95–106.
Rinke S, Behi F, Huls A . Fitting accuracy of all-ceramic posterior crowns produced with three different systems. J Dent Res 2001; 80: Special issue (IADR Abstracts) abstract no 0997 p 651.
Andersson M, Oden A . A new all-ceramic crown: A densely-sintered, high-purity aluminua coping with porcelain. Acta Odontol Scand 1993; 51: 59–64.
Ödman PA, Andersson B . Procera AllCeram crowns followed for 5-10.5 years. Int J Prostodont 2001; 14:
Tinschert J, Natt G, Mautsch W, Spiekermann H, Anusavice KJ . Marginal fit of alumina- and zirconia-based fixed partial dentures produced by CAD/CAM system. Oper Dent 2001; 26: 367–374.
Sparrius O, Grossman ES . Marginal leakage of composite resin restorations in combination with dentinal and enamel bonding agents. J Prosthet Dent 1989; 61: 678–684.
Kern M, Strub JR, Lu XY . Wear of composite resin veneering materials in a dual-axis chewing simulator. J Oral Rehabil 1999; 26: 372–378.
DeLong R, Douglas WH . An artificial oral environment for testing dental materials. IEEE Trans Biomed Eng 1991; 38: 339–345.
Sorensen JA . A standardized method for determination of crown margin fidelity. J Prosthet Dent 1990; 64: 18–24.
DeLong R, Sakaguchi RL, Douglas WH, Pintado MR . The wear of dental amalgam in an artificial mouth: a clinical correlation. Dent Mater 1985; 1: 238–242.
Sakaguchi RL, Douglas WH, DeLong R, Pintado MR . The wear of a posterior composite in an artificial mouth: a clinical correlation. Dent Mater 1986; 2: 235–240.
Bates JF, Stafford GD, Harrison A . Masticatory function - a review of the literature. III. Masticatory performance and efficiency. J Oral Rehabil 1976; 3: 57–67.
Kumagai H, Suzuki T, Hamada T, Sondang P, Fujitan M . Occlusal force distribution on the dental arch during various levels of clenching. J Oral Rehabil 1999; 26: 932–935.
Rinke S, Huls A, Jahn L . Marginal accuracy and fracture strength of conventional and copy-milled all-ceramic crowns. Int J Prosthodont 1995; 8: 303–310.
Groten M, Axmann D, Probster L, Weber H . Determination of the minimum number of marginal gap measurements required for practical in-vitro testing. J Prosthet Dent 2000; 83: 40–49.
Davis DR . Comparison of fit of two types of all-ceramic crowns. J Prosthet Dent 1988; 59: 12–16.
Pera P, Gilodi S, Bassi F, Carossa S . In vitro marginal adaptation of alumina porcelain ceramic crowns. J Prosthet Dent 1994; 72: 585–590.
Friedlander LD, Munoz CA, Goodacre CJ, Doyle MG, Moore BK . The effect of tooth preparation design on the breaking strength of Dicor crowns: Part 1. Int J Prosthodont 1990; 3: 159–168.
Pröbster L . Compressive strength of two modern all-ceramic crowns. Int J Prosthodont 1992; 5: 409–414.
Kern M, Schaller HG, Strub JR . Marginal fit of restorations before and after cementation in vivo. Int J Prosthodont 1993; 6: 585–591.
Bieniek KW, Marx R . The mechanical loading capacity of new all-ceramic crown and bridge materials. Schweiz Monatsschr Zahnmed 1994; 104: 284–289.
Ferrari M, Mason PN, Poli L, Di Dente M . Marginal adaptation of crowns: a scanning electron microscopic investigation. Int J Periodont Rest Dent 1994; 14: 273–279.
Steinbrenner H, Eickholz P, Staehle HJ . Zur Reproduzierbarkeit der qualitativen und quantitativen Randanalyse. Dtsch Zahnärztl Z 1995; 50: 920–923.
Molin MK, Karlsson SL, Kristiansen MS . Influence of film thickness on joint bend strength of a ceramic/resin composite joint. Dent Mater 1996; 12: 245–249.
Fransson B, Oilo G, Gjeitanger R . The fit of metal-ceramic crowns, a clinical study. Dent Mater 1985; 1: 197–199.
Karlsson S . The fit of Procera titanium crowns. An in vitro and clinical study. Acta Odontol Scand 1993; 51: 129–134.
Belser UC, MacEntee MI, Richter WA . Fit of three porcelain-fused-to-metal marginal designs in vivo: a scanning electron microscope study. J Prosthet Dent 1985; 5: 24–29.
Kawai K, Isenberg BP, Leinfelder KF . Effect of gap dimension on composite resin cement wear. Quintessence Int 1994; 25: 53–58.
Bayne SC, Taylor DF, Rekow ED, Wilder AD, Heymann HO . Confirmation of Leinfelder clinical wear standards. Dent Mater 1994; 10: 11–18.
Buchalla W, Attin T, Hellwig E . Brushing abrasion of luting cements under neutral and acidic conditions. Oper Dent 2000; 25: 482–487.
Yoshinari M, Derand T . Fracture strength of all-ceramic crowns. Int J Prosthodont 1994; 7: 329–338.
Hahn P, Schaller H, Hafner P, Hellwig E . Effect of different luting procedures on the seating of ceramic inlays. J Oral Rehabil 2000; 27: 1–8.
Alkumru HN, Wilson HJ, Bor S . The fit of all-ceramic crowns cemented with different luting agents. J Marmara University Dental Faculty 1992; 1: 198.
Oilo G, Evje D . Film thickness of dental luting cements. Dent Mater 1986; 2: 85–289.
Staninec M, Giles WS, Saiku JM, Hattori M . Caries penetration and cement thickness of three luting agents. Int J Prosthodont 1988; 1: 259–263.
Eppenberger J, Marinello CP, Scherle W, Schärer P . Composite as an attachment cement? Initial clinical experiences in crown and bridge prosthetics. Schweiz Monatsschr Zahnheilk 1987; 97: 1237–1250.
Krejci I, Mueller E, Lutz F . Effects of thermocycling and occlusal force on adhesive composite crowns. J Dent Res 1994; 73: 1228–1232.
Acknowledgements
The authors are very grateful to Prof. Dr. H. F. Kappert, PD Dr. R. Kohal and M. Bächle. Technical support by Vivadent-Ivoclar AG, Schaan, FL - H. P. Foser.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Stappert, C., Dai, M., Chitmongkolsuk, S. et al. Marginal adaptation of three-unit fixed partial dentures constructed from pressed ceramic systems. Br Dent J 196, 766–770 (2004). https://doi.org/10.1038/sj.bdj.4811390
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4811390
This article is cited by
-
The effect of pre-ceramic soldering on marginal and internal fit of 4-unit zirconia frameworks and monolithic zirconia fixed dental prostheses
Odontology (2024)
-
Marginal adaptation of lithium disilicate ceramic crowns cemented with three different resin cements
Clinical Oral Investigations (2019)
-
Pressed ceramic in fixed partial dentures construction
British Dental Journal (2004)