Abstract
Objective To investigate the effect of midazolam and flumazenil on psychomotor function and alertness in human volunteers.
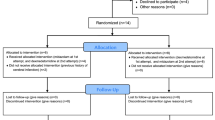
Design Randomised, double-blind, cross over study.
Methods Intravenous flumazenil was administered to sedated and non-sedated healthy human volunteers, in doses typical of those used clinically to induce sedation with midazolam and for reversal with flumazenil. Subjective assessment of alertness and objective measures of psychomotor function using light reaction time and the Maddox wing were made over a 1 hour period.
Results Seven males and seven females each attended four experimental sessions. Psychomotor function was impaired by midazolam but there was some individual variation to this response. All sedated subjects receiving flumazenil had significantly improved alertness and psychomotor function when compared with those subjects who received placebo. Mean alertness (P < 0.01) and light reaction time (P < 0.05) showed significant improvement and returned to baseline by 60 minutes. Stability also showed significant improvement (P < 0.05) but did not return to baseline by 60 minutes. There was no significant effect on psychomotor function or alertness when the antagonist flumazenil was administered in the absence of the agonist midazolam.
Conclusion An earlier discharge time based on subjective assessment of alertness is not advocated for patients whose intravenous midazolam sedation is reversed with flumazenil.
Similar content being viewed by others
Main
Benzodiazepines are now commonly used as intravenous sedatives for many dental and oral surgery procedures that may be unpleasant or when the patient is particularly anxious.1 In this context they have many desirable properties and few unwanted effects, when used in association with appropriate patient selection, and a carefully controlled technique. Benzodiazepines, including diazepam and midazolam, have proved to be safe and effective for intravenous conscious sedation in dentistry.2 Their selective anxiolytic activity and wide safety margin contribute to their popularity. Midazolam (Hypnovel, Roche Products Ltd) has superseded diazepam as the drug of choice because of better tolerance on injection, fewer venous complications, higher incidence of profound anterograde amnesia and more rapid metabolism. While the risk of overdose is very low with benzodiazepines because of their high therapeutic index, the introduction of the benzodiazepine receptor antagonist, flumazenil, has provided flexibility and added safety. 3 Some have advocated a shorter recovery period when benzodiazepine sedation is reversed with flumazenil.4
Flumazenil (Anexate, Roche Products Ltd.) rapidly and effectively terminates the actions of benzodiazepines by competitive antagonism at specific benzodiazepine receptors in the central nervous system.5,6,7 It has been shown to rapidly reverse the sedative effects of benzodiazepines in normal subjects8,9 and patients appear more awake4 but there has been some suggestion that psychomotor function may remain impaired after reversal.1,10 A previous study by the authors,11 has reported poorer psychomotor performance in patients whose sedation was reversed with flumazenil compared with patients who were allowed to recover spontaneously. The aim of this study was to investigate the effects of midazolam and its antagonism with flumazenil on psychomotor performance and alertness in human volunteers. Intravenous flumazenil was administered to sedated and non-sedated human volunteers, in doses typical of those used clinically to induce sedation with midazolam and for reversal with flumazenil.
Method
Healthy volunteers were recruited by advertisement within The University of Manchester. Respondents were then invited for interview to inform them about the nature of the study, to carry out medical screening and to obtain written consent. Health screening was undertaken by questionnaire, physical examination and full blood count investigation. Volunteers were excluded if they were taking any central nervous system (CNS) active medication, suffered from epilepsy, were pregnant or lactating or suffered any cardiovascular or respiratory impairment. A total of 14 male and female ASA (American Society of Anaesthesiologists Classification of physical status) Class I subjects were entered into the study. Expenses were paid for study attendance. The protocol was approved by the Research Ethics Committee of Central Manchester Health Authority.
The study was carried out within the Oral Surgery Day Case Unit of the Manchester Royal Infirmary where facilities for resuscitation were available. Subjects were required to attend four experimental sessions as follows:
-
Session A Subjects received an intravenous injection of 3 ml physiological saline, followed 15 minutes later by a further 5 ml of physiological saline
-
Session B Subjects received an intravenous injection of 3 ml physiological saline, followed 15 minutes later by 0.5 mg (5 ml) of flumazenil
-
Session C Subjects received an intravenous injection of midazolam (Hypnovel 10 mg/5 ml), to a level of satisfactory sedation as judged by the administering clinician up to a maximum dose of 6 mg (3 ml) followed 15 minutes later by 0.5 mg (5 ml) of flumazenil
-
Session D Subjects received an intravenous injection of midazolam (Hypnovel 10 mg/5 ml), to a level of satisfactory sedation as judged by the administering clinician up to a maximum dose of 6 mg (3 ml) followed 15 minutes later by 5 ml of physiological saline.
The order in which subjects attended these sessions was randomly allocated. A summary of this schedule is shown in Table 1. There was a 7-day minimum interval between each session. If a subject was unable to attend on all four occasions then they were excluded from the study.
At the start of each experimental session subjects were seated on a semi-reclined chair and an indwelling intravenous cannula sited in the dorsum of the hand. A subjective global assessment of alertness was made by the experimenter according to the following categorical scale: (i) Alert, (ii) Drowsy, and (iii) Sedated. Baseline objective psychomotor testing was then carried out using the following two tests:
-
1
Reaction time was measured using a simple light reaction time apparatus, in which reaction times taken to perceive and extinguish randomly illuminated light sources were recorded and the mean of ten recordings calculated.
-
2
Stability was assessed using the Maddox wing,12 which measures extra-ocular eye muscle imbalance. The subjects' field of vision looking into the instrument is divided by oblique and vertical wings revealing an arrow in the right eye and a numerical scale in the left. Benzodiazepine sedation induces eye divergence, because of its muscle relaxation effect, and this can be measured objectively by the numerical scale. The degree of divergence is measured by asking the subject to report the number that the image of the arrow points to when it stops moving, higher values corresponding to increased sedation. This objective measure of extra-ocular muscle relaxation provides an indirect measure of the patients postural stability.
Drug preparation was carried out by an independent clinician holding the randomisation code so that the experimenter and subject were blind to a drugs identity. As the experimenter was not aware of whether the prepared syringe contained saline or midazolam, drugs were administered for safety according to the following schedule.
The first drug which could have been saline or midazolam (Table 1) was administered according to recommendations for conscious intravenous sedation with midazolam (Roche Hypnovel Data Sheet). Initially, 1 ml of the solution was injected over 30 seconds and then following a 2-minute pause, further 0.5 ml increments per minute were given until a satisfactory level of sedation as judged by the experimenter was achieved or until a maximum volume of 3 ml (equivalent to 6 mg midazolam or 3 ml saline) had been injected.
The second drug administration was carried out 15 minutes following the first. The second drug could have been saline or flumazenil (Table 1) and so was administered according to the guidelines for reversal of conscious sedation with flumazenil (Roche Annexate Data Sheet). Initially, 2 ml of the solution were injected over 15 seconds and then following a 1 minute pause, further 1 ml increments per minute were given, up to a maximum of 5 ml of solution (equivalent to 0.5 mg flumazenil or 5 ml saline).
One minute following titration of the first drug, the two psychomotor tests were repeated. Psychomotor testing was then repeated at 15-minute intervals for 1 hour. The third testing was therefore carried out 1 minute following titration of the second drug. Subjective global assessments of alertness were made by the experimenter every 15 minutes, at the same time points as for the psychomotor testing.
Continuous pulse rate and peripheral arterial oxygen saturation were monitored with non-invasive pulse oximetry (Ohmenda Biox 3700) for 1 hour. Subjects were allowed home with an escort after 1 hour had elapsed from the time of the final increment of the first injection. All subjects were advised after each experimental session to refrain from driving, operating machinery or drinking alcohol until the next day.
Data were analysed using Wilcoxon, McNemar and t-test for paired observations. Results were adjusted for multiple comparisons (five comparisons as the comparison saline-> flumazenil and midazolam-> saline was not clinically useful). For the statistical calculations, the software package SPSS was used (SPSS 8.0, 1998).
Results
Seven males and seven females were entered into the study, with an age range of 19–24 years (mean = 20.4 years). Each subject attended all four experimental sessions. The mean dose of midazolam administered was 5.78mg (SD = 0.93). The mean peripheral arterial oxygen saturation was 98% and there were no recordings below 90% at any time during the study. There were no adverse events during the study sessions or reported after discharge.
Subjective assessment of alertness
All the participants were alert at the baseline of each experimental session. During saline->saline session and saline->flumazenil sessions, all the participants were alert (Table 2). However, at the end of sessions (60 minutes), only 9 (64%) of the participants receiving midazolam->saline were alert while most (13, 93%) were alert after receiving midazolam->flumazenil. There was no statistically significant difference when comparing the two former sessions with saline->saline results (McNemar test, corrected P > 0.05). In order to asses overall alertness during each session, a total alertness score during the 60 minutes session was calculated for each participant as the number of times being alert. It was significantly lower in comparison to saline->saline session for both midazolam sessions (Wilcoxon corrected P < 0.01 for both sessions). The score for midazolam->saline session was low in comparison to midazolam->flumazenil (Wilcoxon corrected P < 0.01).
Light reaction time
Mean light reaction time by session and time is presented in Figure 1. For all the participants throughout all experimental sessions, the minimum light reaction time was 0.26 and the maximum was 2.25. When final (60 minutes) measurements were compared between each two sessions, the only significant difference was found between midazolam-> saline and saline->saline (paired t-test corrected P = 0.01). To assess overall light reaction time during the experiment, an area under the curve was calculated for each session for each participant. Each two groups were significantly different (paired t-test corrected P < 0.01) except saline->saline and saline-> flumazenil sessions (P = 0.70) and midazolam-> flumazenil and midazolam-> saline (P = 0.03). One subject showed no change in light reaction time following the injection of 6 mg midazolam.
Maddox wing stability
Mean stability by session and time is presented on Figure 2. For all the participants throughout all experimental sessions minimum stability was 0 and maximum 16. When final (60 minutes) measurements were compared between each two sessions, the only statistically significant difference found for comparison was midazolam->flumazenil and saline-> flumazenil (paired t-test corrected P < 0.01). To assess overall stability during the experiment, an area under the curve was calculated for each session for each participant. Each two groups were significantly different (paired t-test corrected P < 0.01) except for saline-> saline and saline -> flumazenil (P = 0.03) and midazolam->flumazenil and midazolam-> saline (P = 0.05). One subject showed no change in stability following the injection of 6 mg midazolam.
Discussion
No significant change from baseline in light reaction time, stability or alertness was observed in the control group (receiving saline followed by saline). This supports the validity of the measures used in this study. No adverse events were associated with the study and monitoring of peripheral arterial oxygen saturation indicated that there were no episodes of respiratory depression resulting in hypoxia.
No significant effect on psychomotor function or alertness was observed when the antagonist flumazenil was administered in the absence of the agonist midazolam. This is not unexpected as flumazenil is known to act as a competitive antagonist with the benzodiazepine/GABA receptor complex5,13 but was interesting to confirm as some workers have cast doubt on the commonly accepted GABAergic mechanism of action for midazolam and flumazenil.14 This observation concurs with the findings of other studies15,16 reporting very little or no effect seen in isolated tissues at even relatively high concentrations of flumazenil and suggests an absence of agonist activity.
Psychomotor function as measured by light reaction time was significantly poorer in the midazolam followed by saline group than the placebo group (saline followed by saline). However, one subject suffered no such impairment following the injection of 6 mg midazolam. Stability as measured with the Maddox wing was significantly poorer in the midazolam followed by saline group than the placebo group (saline followed by saline), but again, one subject suffered no changes in stability following 6 mg midazolam. This was a different subject to one showing no light reaction impairment. Impaired psychomotor function is to be anticipated following injection of midazolam and is well reported in the literature. However, the variation in individual psychomotor response to midazolam observed in this study is clinically important. Other workers have reported such a variation in response to both midazolam and flumazenil.17
Sedated subjects given flumazenil had significantly improved psychomotor function when compared to those subjects who received saline. Mean light reaction times returned to baseline at the 45 minutes time point. Light reaction times did not return to baseline at 60 minutes in the midazolam group when flumazenil was not used for reversal. Sedated subjects given flumazenil had significantly improved stability when compared to those given saline. However, even at 60 minutes, stability was still significantly different from the control group. Other workers have reported variable changes in psychomotor function. Hunter et al. noted that flumazenil administration significantly improved Choice Reaction Times,1 but failed to reverse changes in Critical Flicker Fusion up to 120 minutes later. Klaffey et al. noted little difference between reversed and placebo groups.10
Alertness was significantly different between the subjects receiving midazolam followed by saline and the control group (saline followed by saline). Sedated subjects given flumazenil had significantly improved alertness when compared with those given saline as described by other investigators.18 At 60 minutes, alertness was not significantly different from the control group.
While subjective assessment of alertness was judged as being returned to baseline at 60 minutes after titration with midazolam in subjects who were reversed with flumazenil, the stability of these subjects was significant different from baseline. Subjective assessment of alertness alone may therefore be inadequate criteria for the safe discharge of patients.
A previous study investigated psychomotor function and alertness in response to flumazenil reversal in a group of patients rather than volunteers.11 While alertness was found to be significantly improved by reversal with flumazenil compared with the spontaneously recovering patients, psychomotor testing with light reaction time and Maddox wing stability both revealed significantly poorer performance in the group reversed with flumazenil rather than spontaneously recovering.
The apparent inconsistency in the literature regarding the variable psychomotor response to flumazenil reversal has several possible explanations. It may be that resedation after antagonism of midazolam sedation with flumazenil is occurring because some individuals have rapid elimination of flumazenil but slow elimination of midazolam. Divergence in the disposition and elimination of midazolam and flumazenil has been described in the literature, with the midazolam elimination half-life ranging from less than half that of flumazenil to more than three times that of flumazenil in some individuals and resulting in a relatively poor correlation between calculated receptor occupancy and psychomotor testing and scale of sedation and anxiolysis.13
An alternative explanation may lie in the nature of the study populations. The group described in the previous study by the authors consisted of anxious patients and this study group, non-anxious volunteers. Perhaps anxiety has effected the psychomotor function in response to flumazenil. However the suggestion that catecholamines may modulate the receptor activity requires further investigation. Interestingly there is evidence in the literature that the mechanism of action of benzodiazepines is modulated by the action of sexual hormones and that testosterone plays a relevant role.18
It has been suggested that the elimination half-lives of benzodiazepines do not necessarily correspond with their sedative pharmacodynamic effects19 and this has lead some to advocate continuous infusion of flumazenil for 2 hours to ensure that patients are free from resedation following induction of anaesthesia with midazolam.20 Certainly after the smaller doses required for conscious sedation, there is no evidence that this is required. When the effect of flumazenil declines, patients only return to the level of sedation which would have been present had they not received flumazenil. The term 'residual sedation' is therefore probably more appropriate than 'resedation'. There are no reports of clinically significant residual sedation when flumazenil has been used to reverse midazolam-induced sedation for endoscopy.21
Conclusions
The mean psychomotor function as measured by light reaction time and Maddox wing stability was significantly poorer following midazolam when compared with the placebo group. However it is important to note that there was some individual variation to this response. All sedated subjects given flumazenil had significantly improved subjective measures of alertness and also significantly improved psychomotor function when compared with those subjects who received placebo. Alertness returned to baseline by 60 minutes in this group and mean light reaction time also returned to baseline in this time frame. However, while stability also showed some improvement, it did not return to baseline by 60 minutes. While it would be inappropriate to suggest that these psychomotor function parameters should be returned to baseline prior to discharge, given the individual variability in the responses to these drugs observed in this study, a shorter recovery period cannot be advocated for all patients whose intravenous midazolam sedation is reversed with flumazenil. Patients receiving flumazenil should not therefore be discharged home earlier according to their subjective alertness.
References
Hunter K M, Zacharias M, Parkinson R, Luyk N H . Effect of flumazenil on the recovery from intravenous midazolam. N Z Dent J 1994; 90: 9–12.
Runes J, Strom C . Midazolam intravenous conscious sedation in oral surgery. A retrospective study of 372 cases. Swed Dent J 1996; 20: 29–33.
Finder R L, Moore P A . Benzodiazepines for intravenous conscious sedation: agonists and antagonists. Compendium 1993; 14: 972–780.
al-Quorain A . The use of flumazenil in reversing the midazolam and diazepam sedation in outpatients undergoing gastroscopy. Trop Gastroenterol 1993; 14: 51–54.
Zhi J, Massarella J W, Melia A T et al. The pharmacokinetic-pharmacodynamic (Digit Symbol substitution test) relationship of flumazenil in a midazolam steady-state model in healthy volunteers. Clin Pharmacol Ther 1994; 56: 530–536.
Cone A M, Stott S A . Fumazenil. Br J Hosp Med 1994; 51: 346–348.
Shannon M, Albers G, Burkhart K et al. Safety and efficacy of flumazenil in the reversal of benzodiazepine-induced conscious sedation. J Pediatr 1997; 131: 582–586.
Darragh A, Lamb R, Kenny M, Brick I, Taaffe W, O'Boyle C . Ro 15-1788 antagonises the central effects of diazepam in man without altering diazepam bioavailability. Br J Clin Pharmacol 1982; 14: 677–682.
Lauvan P M, Stoeckel H, Schilden H, Arendt R, Greenblatt D J, Schuttler J : Application of a benzodiazepine antagonist (Ro 15-1788) under steady-state conditions of midazolam. Anesthesiolgy 1982; 57: A325–A326.
Klaffey L, Plourde G, Morris J, Trahan M, Dean D M . Sedation with midazolam during regional anaesthesia: is there a role for flumazenil? Can J Anaesth 1994; 41: 1084–1090.
Thomson P J, Coulthard P, Snowdon A T, Mitchell K : Recovery from intravenous sedation with midazolam — the value of flumazenil. Br J Oral Maxfacial Surg 1993; 31: 101–103.
Hannington-Kiff J G . Measurement of recovery from out-patient general anaesthesia with simple ocular test. Br Med J 1970; 3: 132.
Short T G, Young K K, Tam Y H, Gin T, Oh T E : Midazolam and flumazenil pharmacokinetics and pharmacodynamics following simultaneous admin-istration to human volunteers. Acta Anaesthesiol Scad 1994; 38: 350–356.
Ishizawa Y, Furuya K, Yamagishi S, Dohi S . Non-GABAergic effects of midazolam, diazepam and flumazenil on voltage-dependent ion currents in NG108-15 cells. Neuroreport 1997; 8: 2635–2638.
Krespan B, Springfield S A, Haas H, Geller H M . Electrophysiological studies on benzodiazepine antagonists. Brain Res 1984; 295: 265–274.
Schofield C N . Ro 15-1788 is a potent antagonist of benzodiazepines in the olfactory cortex slice. Pfugers Arch 1983; 396: 292–296.
Gupta, A, Lind S, Eklund A, Lennmarken C . The effects of midazolam and flumazenil on psychomotor function. J Clin Anesth 1997; 9: 21–25.
Pesce M E, Acevedo X, Pinardi G, Miranda H F . Gender differences in diazepam withdrawal syndrome in mice. Pharmacol Toxicol 1994; 75: 353–355.
Riano R E, Kassum D A, Aronson K J . Comparison of sedative recovery times after midazolam versus diazepam administration. Crit Care Med 1994; 22: 1492–1496.
Yoshino A, Nishimura K, Tatsumi K et al. Effect of continous infusion of flumazenil on unexpected postoperative resedation by midazolam. Masui Jap J Anesth 1994; 43: 1668–1674.
McCloy R . Asleep on the job: sedation and monitoring during endoscopy. Scand J Gastroenterol 1992; 27: 97–101.
Author information
Authors and Affiliations
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Coulthard, P., Sano, K., Thomson, P. et al. The effects of midazolam and flumazenil on psychomotor function and alertness in human volunteers. Br Dent J 188, 325–328 (2000). https://doi.org/10.1038/sj.bdj.4800470
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4800470