Key Points
-
The epithelial root sheath of Hertwig is necessary for root growth
-
Although usually sensitive to trauma the epithlial root sheath of Hertwig may survive significant insult
-
Tooth apex development may occur separate from the coronal tooth portion if the root sheath remains viable
-
Regular, long-term clinical and radiographic review is advocated for all trauma cases.
Abstract
Two cases of trauma to immature teeth are described which differed significantly in their initial severity. However, both subsequently presented with continued apical root formation. In the two cases a histological examination after tooth removal confirmed continued apical development ot the traumatised immature teeth distant to their respective coronal portions. These cases highlight the resilience of the root sheath of Hertwig to trauma.
Similar content being viewed by others
Main
Traumatic injuries to young permanent teeth are not uncommon, affecting 30 per cent of children.1 The majority of accidents occur when root formation is still immature2 and the effects may be very destructive.
Many studies have looked at root growth subsequent to trauma and have highlighted the importance of the root sheath of Hertwig in continued root formation. It is thought to provide a source of undifferentiated cells that could give rise to further hard tissue formation. In addition, it may protect against the ingrowth of periodontal ligament cells into the root canal which would result in intracanal bone formation and arrest of root development.3
The root sheath of Hertwig is usually sensitive to trauma, however in some circumstances it may resist damage from trauma and infection.4,5 The following case reports aim to highlight this fact by presenting unusual sequelae of trauma to both erupted and unerupted developing permanent incisors.
Case 1
A healthy 7fi year old boy was referred to the department of Child Dental Health by his dental practitioner after a cycling accident. He attended 11 days following the incident complaining of a loose upper tooth.
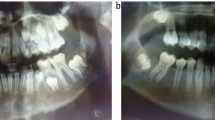
On examination his upper right permanent central incisor (tooth 11) was minimally mobile, but was in good occlusion and not tender to percussion. The tooth responded positively to sensitivity testing, and radiographs (Fig. 1) revealed it to have a very immature apex with no evidence of root fracture. No treatment was necessary, and the parents requested follow up with their dental practitioner.
Seven years later another practitioner re-referred the patient because of persistent buccal and palatal swelling associated with teeth 11 and 12. Examination revealed 12 to be periostitic and 11 to be darkened. There was a marked fluctuant swelling of the palatal mucosa in the 13, 12 and 11 region. Vitality tests with electric pulp tester were positive for 12, 21, 22 but negative for 11. Radiographs revealed a large poorly defined periapical radiolucency extending from the midline of the maxilla to tooth 13, and this appeared to have caused displacement of the root of tooth 12 (Fig. 2). Tooth 11 had an immature root formation and separate and apical to this was a 5 mm↔5 mm radiopacity that appeared to be an apical fragment.
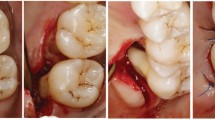
Treatment consisted of extraction of 11 and curettage of the apical region under a short general anaesthetic.The fragment removed from the 11 apical area proved both macroscopically(Fig. 3) and microscopically(Fig. 4) to be a completed apex.
Case 2
A healthy 13 year old boy attended for an orthodontic assessment with imbricated lower incisors and a retained lower primary incisor. He had apparently sustained a fracture of his mandible in the region of the retained primary tooth as a result of a cycle accident at age 4 years.
Clinical examination showed retained 71 to be minimally mobile and 31 to be absent. Radiographic investigation revealed the following:
-
71 with a calcified root canal
-
32 with an apical third root dilaceration
-
31 to be unerupted and in 2 fragments (the coronal part of 31 with a calcified pulp chamber and the apical portion of 31 distinct from the coronal portion) (Fig. 5).
The orthodontic treatment plan included extraction of 71 and 31 and subsequent histopathological examination revealed the following: 71 with an obliterated pulp canal by calcified repair tissue and apical resorption with associated cellular fibrosis(Fig. 6); 31 with pulp canal obliteration by calcified repair tissue (Fig. 7) and a separate apical fragment.
Discussion
Rule and Winter6 stated that root growth is only possible where the epithelial root sheath of Hertwig has retained its specialised function. In the cases reported, in spite of the different types of trauma, the root sheath of Hertwig remained viable and continued to map out the apical fragments of the teeth at positions displaced from their coronal portions. Indeed Andreasen et al.,3 Smith and Thaler,5 Gibson,7 Burley et al.,8 Cooke and Rowbotham,9 and Feiglin,10 have described similar cases of continued root formation, even in unfavourable conditions following dental trauma. These cases emphasise the considerable powers of recovery of the dental papilla, probably due to its large number of undifferentiated mesenchymal cells.
From a practical point of view this emphasises the need for regular systematic review of all trauma cases which may have resulted in tooth displacement and disruption of the root sheath of Hertwig. Any review must include good quality periapical radiographs, clinical observation of the colour of the tooth, the presence or not of sinus formation, sensitivity testing, and whether the tooth is tender to percussion.
The management of teeth with separate apical root fragments may be technically difficult. Should the tooth retain clinical and radiographic vitality it is acceptable to continue to monitor the tooth. However, if loss of vitality is suspected then root canal treatment is indicated. Induced apical closure of the coronal fragment using non-setting calcium hydroxide paste is the treatment of choice. This should be followed by root canal obturation to create a hermetical apical seal. The latter is often technically demanding due to the width of the immature canal, and the thin fragile walls make the tooth susceptible to root fracture during treatment. The retained apical fragment may be left in-situ unless it becomes infected or hinders orthodontic tooth movement.
All trauma cases should receive careful initial assessment. Only treatment appropriate to the correct diagnosis will achieve an acceptable clinical outcome. Regular clinical and radiographic review of all traumatised teeth is critical, as non-vitality may occur as late as 2–6 years after an injury.
References
Andreasen J O, Andreasen F M . Textbook and Colour Atlas of Traumatic Injuries to the teeth. 3rd ed. Munksgaard 1994.
Andreasen J O, Ravn J J . Epidemiology of traumatic dental injuries to primary and permanent teeth in a Danish population sample. Int J oral Surg 1972; 1: 235–9.
Andreasen J O, Borum M K, Andreasen F M . Replantation of 400 avulsed permanent incisors. Endod Dent Traumatol 1995; 11: 69–75.
Rule D C . Proc Brit Paedodontic Soc 1973; 3: 33.
Cvek M . Prognosis of luxated non-vital maxillary incisors treated with calcium hydroxide and filled with gutta percha. Endod Dent Traumatol 1992; 8: 45–55.
Rule D C, Winter G B . Root growth and apical repair subsequent to pulpal necrosis in children. Br Dent J 1966; 120: 586–590.
Gibson A C L . Continued root development after traumatic avulsion of poorly formed permanent incisor. Br Dent J 1969; 126: 356–7.
Burley M A, Reece A . Root formation following traumatic loss of an immature incisor. Br Dent J 1976; 141: 315–6.
Cooke C, Rowbotham T C . Root canal therapy in non-vital teeth with open apices. Br Dent J 1960; 108: 147–150.
Feiglin B . Differences in apex formation during apexification with calcium hydroxide paste. Endod Dent Traumatol 1985; 1: 195–199.
Acknowledgements
We gratefully acknowledge the help of the Department of Oral Pathology, Newcastle upon Tyne Dental School and Hospital.
Author information
Authors and Affiliations
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Welbury, R., Walton, A. Continued apexogenesis of immature permanent incisors following trauma. Br Dent J 187, 643–644 (1999). https://doi.org/10.1038/sj.bdj.4800356
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4800356
This article is cited by
-
Radiographic outcomes and prognostic factors in nonvital immature permanent teeth after apexification with modified calcium hydroxide paste: a retrospective study
Clinical Oral Investigations (2022)
-
Effect of Er,Cr:YSGG laser irradiation on eruption of rat mandibular incisor after disturbance of the enamel organ in the pulp
Lasers in Medical Science (2006)
-
Pulsed Nd:YAG laser effect on eruption of rat mandibular incisors following disturbance of the enamel organ in the pulp
Lasers in Medical Science (2005)