Abstract
Aim The aim of this study was to compare the incidence of glove perforation when double gloved or single gloved during the routine treatment of HIV-positive patients. In addition, a glove perforation indication system based on a double gloving technique was assessed.
Design Prospective, randomised and open study of glove perforation.
Methods 138 consecutive HIV-positive patients underwent routine dental treatment by senior dental staff and dental hygienists in a teaching hospital. Staff wore either single gloves (Regent Biogel D or standard surgical gloves) or double gloves (Regent 'Reveal' perforation indication system or standard surgical gloves). A subjective assessment of glove comfort, sensitivity and ease of donning was made using a visual analogue scale.
Results The incidence of glove perforation/procedure was low, 2.9%. There were no skin penetrating injuries, visible exposure to body fluids or unnoticed perforations. Double gloving was subjectively less comfortable and sensitive than single gloving (P < 0.0001). The glove perforation indication system did not increase the detection of intra-operative perforations.
Conclusions There is unlikely to be any significant benefit from the use of a double gloving technique or perforation indication system during the routine dental treatment of HIV-positive patients.
Similar content being viewed by others
Main
The wearing of gloves is one essential element of the barrier measures required for effective cross-infection control.1,2 Glove perforation rates of between 4–7.5% have been reported during routine operative dentistry and are higher during minor oral surgery procedures.3,4,5,6 The incidence also varies with the duration of the procedure and the quality of the glove, especially if single use gloves are used for several patients.3,5 Many glove perforations pass unnoticed at the time of treatment. Double gloving during minor oral surgery and dental hygiene procedures reduces the incidence of inner glove perforation and therefore potential exposure to cross-infection.5,6 Double gloving of either both hands or just the non-dominant hand has been suggested for procedures that are exposure prone or when treating patients who are 'high-risk' for the transmission of bloodborne viral diseases such as the human immunodeficiency virus (HIV) and hepatitis.3,4,5 Although double gloving will not prevent a penetrating injury it may reduce the risk of disease transmission because of the wiping effect of two layers.8 This is probably most important when a significant volume of blood with a high viral titre is involved. However, all patients should be assumed to be an infection risk and universal barrier precautions applied equally.9
Glove perforation rates during surgery are high in major general surgery, orthopaedic and trauma surgery, including some maxillofacial trauma, and double gloving has been shown to reduce the incidence of inner glove perforation.10,11,12,13,14,15The incidence of unnoticed perforations is often high and the 'Reveal' glove perforation indication system has been shown to increase the intra-operative detection rate.15,16
It is uncertain whether there is a role for double gloving or a glove perforation indication system during the treatment of 'high risk' dental patients. The main aim of this study was to compare the glove perforation rate when using single or double gloving techniques during the routine dental treatment of HIV-positive patients. In addition, a glove perforation indication system was assessed to determine whether it increased the intra-operative detection of perforations. A comparison of glove comfort, sensitivity and ease of donning was also made.
Methods
A prospective, randomised and open study of 138 HIV-positive patients treated by one of two senior dental surgeons (WB and PG) or one of three qualified dental hygienists, during a 6-month period in 1996/7.
The study was divided into single gloving and double gloving arms, with each arm including two different types of glove. The single gloving arm used either Regent Biogel D gloves or sterile surgical gloves and the double gloving arm either the Regent 'Reveal' glove perforation indication system or double sterile surgical gloves. The operator and assistant were both randomly allocated to one of the four subgroups.
The 'Reveal' glove perforation indication system is a double gloving technique using gloves that are identical to surgical gloves except that the inner glove is green. The inner glove becomes visible at the site of an outer glove perforation as fluid seeps through the outer latex and renders it more transparent; this is an optical effect and no dye is released. Universal precautions were practised for all patients.
Single glove arm (n = 71 patients)
-
Single Regent surgical gloves (n = 37)
-
Single Biogel D gloves (n = 34)
Double glove arm (n = 67 patients)
-
Double Regent surgical gloves (n = 27)
-
Regent 'Reveal' perforation indication system (n = 40).
Each dental procedure was classified into one of six subgroups (Table 1). If a glove perforation was noted during a procedure then the glove was replaced and examined later. At the end of a procedure the operator and assistant visually inspected their hands for evidence of contamination with blood. Perforations were detected using a standard water inflation technique. Each glove was filled with at least 500 ml of water. This technique may underestimate the perforation rate by about 25% but allows comparison between studies using a similar method.17 Ten pairs of each type of glove were tested as controls and no perforations were detected.
The operator and assistant recorded their subjective opinions of the ease of glove donning, comfort and sensitivity on visual analogue scales (VAS) marked on a range of one to ten (Table 2).
The glove perforation rate for the single and double gloving arms were compared using the Fishers Exact Test. The VAS scores of both arms were compared using a Mann-Whitney U test.
Results
A total of 759 gloves from 138 patients were examined. There were 251 outer gloves and 248 inner gloves in the double gloving arm, and 260 gloves in the single gloving arm. Four additional patients were excluded from the analysis because of inadequate records. Twenty-two patients were treated by a single operator, single gloved for 12 patients and double gloved for 10 patients.
There were four glove perforations and they were all sustained by the operator (Table 1). They were caused by a drill (2) or an instrument (2) and all occurred during restorative treatment. This group had a statistically significant higher risk of perforation (P = 0.01, Fishers Exact Test). Three of these perforations were in the outer gloves in the 'Reveal' subgroup and one was in the single surgical glove subgroup. Only three gloves were replaced as one perforation occurred at the end of a procedure.
The mean number of perforations/procedure was 2.9% (n = 4/138). It was slightly higher in the double gloving arm than the single gloving arm but this was not significant (4.2%, n = 3/71 compared with 1.5%, n =1/67). The mean outer glove perforation rate in the double gloving arm was 1.2% (n = 3/251) and the glove perforation rate in the single gloving arm was 0.38% (n = 1/260). There were no significant differences between the single and double gloving subgroups. There were no unnoticed perforations, skin penetrating injuries, inner glove perforations or visible exposure to body fluids. The mean procedure duration was 48 minutes (SD = 11.5).
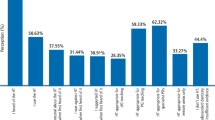
The median VAS scores of the single and double gloving arms were compared using a Mann-Whitney U Test analysis. Glove comfort, sensitivity and ease of donning were all significantly higher when using a single gloving technique, P < 0.0001 (Table 3). There was no significant difference between the Biogel D gloves and single standard surgical gloves or between the 'Reveal' system gloves and double gloving with standard surgical gloves.
Discussion
The incidence of glove perforation during dental treatment was relatively low, 2.9% per procedure. There were no skin penetrating injuries, inner glove perforations, unnoticed perforations or visible skin contamination. Restorative procedures had a higher risk of perforation (P = 0.01, Fishers Exact Test) but the low number of perforations should be interpreted with caution. The dental procedures did not seem to be exposure prone and no minor surgical procedures were performed. Several other factors may have contributed to the low perforation rate including: the open study protocol, patient HIV status, experienced staff and attitudes to cross-infection control.
Neither double gloving nor the glove perforation indication system was found to be helpful. The low rate of glove perforation reduced the potential benefit of double gloving and the poor VAS scores indicate that double gloving was uncomfortable for dental procedures. The 'Reveal' system did not increase intra-operative perforation detection because it was necessary to wet the gloves to check for a suspected perforation.
A subjective loss of comfort and sensitivity, during surgery, when double gloved has been reported.10,11 Phillips et al. reported a significant loss of sensory function but a lesser effect upon motor functions performed under direct vision.20 The decision whether to double glove should take account of factors such as: discomfort, loss of sensitivity and dexterity, nature and length of the procedure, and the perceived risk of cross-infection. The Centers for Disease Control recognise exposure prone procedures as being characterised by the 'digital palpation of a needle tip in a body cavity or the simultaneous presence of a healthcare workers fingers and a sharp instrument or object in a poorly visualised or highly confined anatomic site'.9 It is certainly possible to complete some surgical procedures, including maxillofacial trauma, without difficulty while double gloved.15
Whether the surgical extraction of teeth for a 'high risk' patient justifies double gloving remains contentious. A relatively low incidence of glove perforation (4.3% per surgeon/operation side) during the surgical extraction of wisdom teeth under general anaesthesia has been recorded by the current author. 21 Burke et al. reported a higher rate of 16% per minor oral surgery procedure under local anaesthetic.4 There were no skin penetrating injuries in either of these studies. It is likely that the risk of exposure depends on many factors including: the procedure and operating conditions, temperament and skill of the surgeon, and attitudes toward cross-infection control and the use of safe surgical techniques.10
It remains difficult to define a level at which the risk of exposure would justify double gloving. The infection status of a patient is usually unknown and therefore universal barrier precautions should be applied equally and universally. Perhaps individual surgeons should assess their own perforation rate for a procedure and, if it is high, improve their technique or double glove for all patients. It is also sensible to avoid using instruments, materials or techniques that are likely to cause a perforation. If the surgeon has non-intact skin then even a low perforation rate represents a risk of exposure.
Finally, double gloving will reduce the risk of exposure because of a manufacturing defect. The incidence in high quality surgical gloves is less than 0.6% (Standard EN455-1, Regent Medical, UK). Although non-sterile, the Biogel D dental glove should reach this standard but poorer quality gloves will not.22 Whether single or double gloved we strongly recommend the use of a well-fitting high quality glove.
Conclusions
We have found little evidence to support either double gloving or the use of a glove perforation indication system during the routine dental treatment of HIV-positive patients.
References
British Dental Association. Advice Sheet A12. Infection control in dentistry. London: BDA, 1996.
UK Health Departments. Guidance for clinical healthcare workers: protection against infection with blood-borne viruses. Wetherby: Department of Health, 1998.
Baggett F, Burke F J T, Wilson N H F . An assessment of the incidence of punctures in gloves when worn for routine operative procedures. Br Dent J 1993; 174: 412–416.
Burke F J T, Baggett F J, Lomax A M . Assessment of the risk of glove puncture during oral surgery procedures. Oral Surg, Oral Med, Oral Pathol, Oral Radiol, Endod 1996; 82: 18–21.
Patton L, Campbell T L, Evers S P . Prevalence of glove perforations during double-gloving for dental procedures. Gen Dent 1995; 41: 22–26.
Schwimmer A, Massoumi M, Barr C E . Efficacy of double gloving to prevent inner glove perforation. JADA 1994; 125: 196–198.
Burke F J T, Wilson N H F . The incidence of undiagnosed punctures in non-sterile gloves. Br Dent J 1990; 168: 67–71.
Johnson G K, Nolan T, Wuh H C, Robinson W S . Efficacy of glove combinations in reducing cell culture infection after glove puncture with needles contaminated with human immunodeficiency virus type 1. Infect Control Hosp Epidemiol 1991; 12: 435–438.
Centers for Disease Control: recommendations for preventing transmission of human immunodeficiency virus and hepatitis B virus to patients during exposure-prone invasive procedures. MMWR 1991; 40 (1S), RR-8: 1–9.
Gerberding J L, Littell C, Tarkington A, Brown A, Schecter W P . Risk of exposure of surgical personnel to patients' blood during surgery at San Francisco General Hospital. N Engl J Med 1990; 322: 1788–1793.
Quebbeman E J, Telford G L, Wadsworth K, Hubbard S, Goodman H, Gottlieb M S . Double gloving: protecting surgeons from blood contamination in the operating room. Arch Surg 1992; 127: 213–217.
McLeod G G . Needlestick injuries at operations for trauma. J Bone Joint Surg [Br] 1989; 71-B: 489–491.
Matta H, Thompson A M, Rainey J B . Does wearing two pairs of gloves protect operating staff from skin contamination. BMJ 1988; 297: 597–598.
Upton L G, Barber H D . Double gloving and the incidence of perforations during specific oral and maxillofacial surgical procedures. J Oral Maxillofac Surg 1993; 51: 261–263.
Avery C M E, Taylor J, Johnson P A . Double gloving and use of the 'Reveal' glove perforation indication system in maxillofacial trauma surgery. Br J Oral Maxillofac Surg (in press).
Brown J N . Surgeon protection: early recognition of glove perforation using a green under glove. J R Coll Surg Edin 1996; 41: 395–396.
Smith J R, Grant J M . Does wearing two pairs of gloves protect against skin contamination? Br Med J 1988; 297: 1193.
Wilson S J, Uy A, Sellu D, Jaffer M A . Subjective effects of double gloves on surgical performance. Ann R Coll Surg Engl 1996; 78: 20–22.
Watts D, Tassler P L, Dellon A L . The effect of double gloving on cutaneous sensibility, skin compliance and suture. Contemp Surg 1994; 289–292.
Phillips A M, Birch N C, Ribbans W J . Protective gloves for use in high-risk patients: how much do they affect the dexterity of the surgeon? Ann R Coll Surg Engl 1997; 79: 124–127.
Avery C M E, Hjort A, Walsh S, Johnson P A . Glove perforation during the surgical extraction of wisdom teeth. Oral Surg, Oral Med, Oral Pathol, Oral Radiol Endod 1998; 86: 23–25.
Chua K L, Taylor G S, Bagg J . A clinical and laboratory evaluation of three types of operating gloves for use in orthodontic practice. Br J Orthod 1996; 23: 115–120.
Acknowledgements
The authors gratefully acknowledge the support of our staff dental hygienists: Judy Blackshaw, Amanda Filcock and Sue Lloyd. Dr Derek Cooper of King's College School of Medicine and Dentistry for the statistical analysis. Regent Medical, UK for supplying the gloves and secretarial support.
Author information
Authors and Affiliations
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Avery, C., Gallagher, P. & Birnbaum, W. Double gloving and a glove perforation indication system during the dental treatment of HIV- positive patients: are they necessary?. Br Dent J 186, 27–29 (1999). https://doi.org/10.1038/sj.bdj.4800009
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4800009
This article is cited by
-
The People Living with HIV STIGMASurvey UK 2015: Stigmatising experiences and dental care
British Dental Journal (2018)
-
The HIV positive dentist in the United Kingdom - a legal perspective
British Dental Journal (2009)