Abstract
The human immunodeficiency virus type-1 (HIV-1) accessory gene vpr encodes a conserved 96-amino-acid protein that is necessary and sufficient for the HIV-1-induced block of cellular proliferation. Expression of vpr in CD4+ lymphocytes results in G2 arrest, followed by apoptosis. In a previous study, we identified the ataxia telangiectasia-mutated (ATM) and Rad3-related protein (ATR) as a cellular factor that mediates Vpr-induced cell cycle arrest. In the present study, we report that the breast cancer-associated protein-1 (BRCA1), a known target of ATR, is activated in the presence of Vpr. In addition, the gene encoding the growth arrest and DNA damage-45 protein α (GADD45α), a known transcriptional target of BRCA1, is upregulated by Vpr in an ATR-dependent manner. We demonstrate that RNAi-mediated silencing of either ATR or GADD45α leads to nearly complete suppression of the proapoptotic effect of Vpr. Our results support a model in which Vpr-induced apoptosis is mediated via ATR phosphorylation of BRCA1, and consequent upregulation of GADD45α.
Similar content being viewed by others
Introduction
Human immunodeficiency virus type-1 (HIV-1) viral protein R (Vpr) causes cell cycle arrest in G2 of infected lymphocytes, a phenotype that precedes cell death by apoptosis.1, 2, 3, 4 It has been suggested that apoptosis of infected cells may play a significant role in the depletion of CD4+ lymphocytes in vivo.5, 6, 7, 8 The mechanism by which Vpr induces apoptosis is not fully understood. Muthumani et al.9 reported that vpr-expressing cells undergo apoptosis via the intrinsic pathway that involves loss of mitochondrial membrane potential. This pathway of apoptosis is characterized by cytochrome c release, and caspase 9 activation, and is triggered in the absence of death receptor ligation.9 However, the initial event induced by Vpr towards activation of the proapoptotic signaling cascade has not been elucidated.
In an effort to elucidate whether Vpr might directly promote the release of proapoptotic mediators from the mitochondria, Vieira et al.10 and Jacotot et al.12 found that in a cell-free system, Vpr interacts with the permeability transition pore complex (PTPC) to cause ion permeability and swelling of mitochondria leading to release of cytochrome c.10, 11 These results support a model in which Vpr induces mitochondrial depolarization directly rather than activating upstream stress signals.10, 11
In contrast to the studies by Vieira et al.10 and Jacotot et al.,11 our group demonstrated that treatment of vpr-expressing cells with caffeine, which inhibits the DNA damage-signaling proteins ATM and ATR, significantly reduces Vpr-induced apoptosis.4 Our observations indicated that Vpr first induces stress signals that are similar or identical to those induced by certain forms of genotoxic stress, and then these signals activate a proapoptotic signaling cascade. Recently, we found that ATR is the mediator of Vpr-induced DNA damage-like signals.12 This finding provided us with the opportunity to use highly specific molecular tools, such as RNA interference (RNAi), to dissect the upstream signaling events triggered by Vpr. We specifically asked whether activation of ATR was required for Vpr-induced apoptosis, as we previously found for induction of G2 arrest.12 We hypothesized that, if Vpr induces apoptosis by directly binding and controlling the PTPC, then signaling through ATR would still be necessary for induction of G2 arrest, but would be dispensable towards induction of apoptosis. Conversely, if ATR activation was required for induction of apoptosis, then examination of potential proapoptotic phosphorylation targets of ATR should lead to a specific target or set of targets that would mediate the signaling events between ATR activation and apoptosis.
ATR can directly control several targets via serine/threonine phosphorylation.12, 13, 14, 15, 16, 17 These targets include: the checkpoint kinase-1 (CHK1); RAD17; breast cancer associated-1 gene (BRCA1); the histone 2A variant X (H2AX); E2F; and p53. ATR targets initiate signaling cascades that may result in three global effects: cell cycle blockade, recruitment of DNA repair/transcription factors, and induction of apoptosis. We recently identified both RAD17 and H2AX as targets of Vpr.18 We and others previously ruled out p53 as a mediator of apoptosis induced by Vpr.4, 19 Therefore, in an effort to find mediators of apoptosis downstream of ATR, we focused on another proapoptotic target of ATR, BRCA1.
BRCA1 is a tumor suppressor that is mutated in over half of the cases of hereditary breast cancer,20 and has recently emerged as a regulator of both apoptosis and G2 arrest.21, 22 In response to genotoxic insults, BRCA1 is recruited to sites of DNA damage and is phosphorylated by both ATM and ATR.17, 23 BRCA1 has been proposed to play a distinct role in DNA repair and apoptosis as a transcriptional regulator of genes including cyclin B1, p53R2, MDM2, and p53.24 Recently, GADD45α was identified as a transcriptional target of BRCA1.22
GADD45α was originally identified in Chinese hamster cell lines as one of several genes rapidly induced by UV radiation.25 GADD45α is induced by a variety of genotoxic stresses including ionizing radiation (IR), medium starvation, and methyl methanesulfonate (MMS),26, 27 and has been shown to play roles in both G2/M arrest and apoptosis following DNA damage.28, 29 Harkin et al.22 demonstrated that BRCA1-induced upregulation of GADD45α resulted in c-jun N-terminal kinase/stress-activated protein kinase (JNK/SAPK)-dependent apoptosis.
In the present study, we examined targets of ATR with possible roles in Vpr-induced apoptosis. We demonstrate that Vpr-induced apoptosis is signaled through the DNA damage signaling protein ATR, which initiates a pathway that involves phosphorylation of BRCA1 at residue S1423, and subsequent upregulation of GADD45α. We demonstrate that both ATR and GADD45α are required for Vpr-induced apoptosis.
Results
ATR is required for apoptosis induced by HIV-1 Vpr
We have previously shown that Vpr-induced G2 arrest is signaled via the ATR DNA damage pathway.12 Considering the growing body of evidence implicating ATR in the control of apoptosis,30, 31, 32, 33 it was compelling to investigate the participation of ATR in the context of Vpr-induced apoptosis. We transfected HeLa cells with short-interfering RNA (siRNA) duplexes directed at ATR or nonspecific siRNA and then transduced cells with lentiviral vectors expressing either HIV-1NL4-3 Vpr and GFP (pHR-VPR), or GFP alone (pHR-GFP), which were previously described.34 The construct, pHR-VPR, expresses vpr and GFP from a dicistronic mRNA that uses an intervening internal ribosome entry site (IRES). To examine Vpr-induced apoptosis, we treated cells with the nuclear stain, 4′6-diamidino-2-phenylindole dihydrochloride (DAPI), and examined nuclear morphology (Figure 1a). We found that treatment of pHR-VPR-transduced cells with ATR-specific siRNA resulted in a 67% decrease in apoptosis (Figure 1b). This reduction in apoptosis correlated with a reduction in G2 arrest (data not shown). As a control, we used siRNAs against ATM or checkpoint kinase-2 (CHK2). ATM is a close relative of ATR that was shown to be dispensable for Vpr-induced G2 arrest.2, 18 CHK2 is a checkpoint kinase that is activated by ATM, but not by ATR. Knockdown of ATM or CHK2 produced no appreciable changes in the level of apoptosis induced by Vpr (Figure 1b). None of the siRNA treatments had a significant effect on apoptosis in mock-treated or pHR-GFP-transduced cells (Figure 1b).
siRNA-mediated knockdown of ATR and GADD45α abrogates Vpr-induced apoptosis. (a) HeLa cells were transfected with nonspecific (NS) siRNA or siRNA targeted to ATM, CHK2, ATR, or GADD45α then, 48 h post-transfection, cells were mock-transduced or transduced with pHR-VPR. (b) The results from three independent experiments described in panel a were quantitated. (c) Hela cells were either mock treated or transduced with pHR-VPR in the presence of nonspecific siRNA or siRNA targeted to ATR, GADD45α, ATM, or CHK2. At 48 h post-transduction, cell lysates were harvested and subjected to Western blot analysis with anti-PARP antibodies that recognize both full-length PARP and caspase cleaved (89 kDa) PARP. (d) Cells treated with indicated siRNAs were lysed and each siRNA treatment was assayed by Western blot to verify knockdown. (e) To ensure that our siRNA treatments did not affect pHR-VPR expression, lysates from each siRNA treatment were assayed by Western blot for Vpr protein levels
In addition to measuring apoptosis by DAPI staining, we confirmed our results by measuring caspase-induced cleavage of poly(ADP-ribose) polymerase (PARP). PARP cleavage produces an 89 kDa fragment that is an early result of caspase activation, which precedes DNA cleavage,35, 36 and is essential for progression into apoptosis (reviewed in Bernstein et al.30). ATR knockdown resulted in a marked decrease in Vpr-induced PARP cleavage compared to nonspecific siRNA, ATM, and CHK2 siRNA treatments (Figure 1c, compare lanes 2, 3, 5, 6). Kockdown of the corresponding proteins by each of the siRNAs was evaluated by Western blot (Figure 1d).
To rule out the possibility that ATR- or GADD45α-specific siRNA treatments may relieve the effects of Vpr by disrupting expression of Vpr itself rather than affecting the function of ATR or GADD45α, we performed Western blot analysis for Vpr protein in the above experiments (Figure 1e). None of the siRNA treatments had any appreciable effect on Vpr protein levels.
Vpr induces phosphorylation of BRCA1 at serine 1423 in an ATR-dependent manner
Following cellular insults such as ionizing radiation, BRCA1 is recruited to sites of DNA damage where it is phosphorylated by ATR and/or ATM.17, 23, 37 Recruitment of BRCA1 to DNA damage foci can be visualized as a punctate nuclear staining pattern.17, 23, 37 We previously demonstrated that Vpr-induced G2 arrest is associated with BRCA1 and H2AX nuclear foci formation.18 The above work demonstrated that BRCA1 was recruited to DNA damage foci as part of the G2 checkpoint activation.18 As ATR is also required for Vpr-induced apoptosis (Figure 1), and BRCA1 was previously shown to be able to trigger apoptosis,22, 30 we reasoned that ATR may initiate apoptosis through phosphorylation of BRCA1. Following DNA damage, ATR phosphorylates BRCA1 at serine 1423.17, 37 To determine whether Vpr induced the phosphorylation of BRCA1 at serine 1423 in an ATR-dependent manner, we infected HeLa cells with pHR-VPR and examined phosphorylation of BRCA1 at serine 1423 in the presence of either nonspecific or ATR-specific siRNA. We found that Vpr induced phosphorylation of BRCA1 at serine 1423 (Figure 2a). Treatment of HeLa cells with ATR-specific siRNA prior to transduction reduced Vpr-induced phosphorylation of BRCA1 (Figure 2a). Therefore, phosphorylation of BRCA1 by Vpr is ATR-dependent.
Vpr induces ATR-dependent phosphorylation of BRCA1 at serine 1423. (a) HeLa cells were either mock treated or transduced with pHR-VPR in the presence of either nonspecific siRNA or siRNA targeted to ATR. Cell lysates were harvested 48 h post-transduction and then subjected to Western blot analysis with anti-BRCA1 phospho-serine 1423 antibodies. (b) SupT1 CD4+ cells were infected were either infected with HIV-1, HIV-1-VprX, or mock infected. Cells were harvested once infection levels were similar, and each sample was subject to Western blot analysis with anti-BRCA1 phospho-serine 1423 antibodies
The previous experiments were performed with lentiviral vectors in which the vpr gene is expressed from a cytomegalovirus immediate-early promoter. Therefore, we sought to confirm that Vpr expressed in the context of an infection with full-length HIV-1 could induce BRCA1 phosphorylation at serine 1423. To test this, we infected immortalized, CD4+ SupT1 lymphocytes with HIV-1NL4-338 or a vpr mutant, termed HIV-1NL4-3VprX, that expresses a truncated form of Vpr.39 We harvested cells at several timepoints postinfection, measured infection levels by staining for intracellular p24, and examined phosphorylation of BRCA1 by Western blot. To ensure that differences in levels of infection between the two viruses did not affect the results, we compared samples with similar levels of infection (32 and 40% of cells were p24-positive in the HIV-1, and HIV-1-VprX infections, respectively). We found that HIV-1NL4-3, but not HIV-1NL4-3VprX, induced BRCA1 phosphorylation at serine 1423 (Figure 2b). Therefore, Vpr is necessary and sufficient for induction of phosphorylation of BRCA1, whether expressed from a lentiviral vector or in the context of HIV-1.
Knockdown of GADD45α relieves Vpr-induced apoptosis
Recent reports have suggested that GADD45α is a transcriptional target of BRCA1,22, 24, 40 involved in the induction of apoptosis.22 Based on these reports, and our observation that BRCA1 was activated in response to Vpr, we decided to examine whether GADD45α played a role in Vpr-induced apoptosis. We first examined whether GADD45α is required for Vpr-induced apoptosis. We treated HeLa cells with nonspecific siRNA or GADD45α-specific siRNA and then transduced them with pHR-VPR or pHR-GFP, and measured apoptosis by DAPI staining (Figure 1a). We observed that efficient knockdown of GADD45α resulted in a 70% decrease in Vpr-induced apoptosis (Figure 1b). However, ATM-specific, CHK2-specific, or nonspecific siRNA treatments had no appreciable effect on Vpr-induced apoptosis (Figure 1b). PARP cleavage was then measured to verify the results from DAPI staining. As observed with ATR knockdown, GADD45α knockdown prior to pHR-VPR transduction resulted in a marked reduction in PARP cleavage (Figure 1c, compare lanes 2, 4–6).
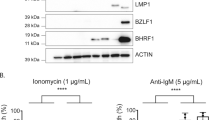
Vpr upregulates GADD45 protein levels in primary CD4+ lymphocytes and SupT1 cells
Based on our previous observation that GADD45α was required for Vpr-induced apoptosis, we hypothesized that vpr expression would lead to upregulation of GADD45α. To determine whether Vpr expression resulted in upregulation of GADD45α protein, we transduced SupT1 cells (a CD4+ lymphocyte cell line) and HeLa cells (HeLa cell data not shown) with pHR viruses. As an additional negative control, we used a lentiviral vector that expressed Vpr with the mutation R80A, which is unable to induce G2 arrest or apoptosis.41 We lysed cells at 24, 48 and 72 h post-transduction and measured GADD45α protein levels by Western blot. In order to quantify GADD45α upregulation by Western blot, we loaded, in parallel to our samples, two-fold dilutions of commercially available, recombinant GADD45α protein (Figure 3a). Based on densitometry scanning analysis using recombinant protein as a standard, we estimated a five-fold upregulation of GADD45α protein at 48 h post-transduction in pHR-VPR-transduced cell lysates, in comparison to lysates from cells transduced with pHR-VPR(R80A) (Figure 3a).
Vpr upregulates GADD45α protein levels in both SupT1 cells, and primary human CD4+ lymphocytes. (a) SupT1 cells were transduced with pHR-VPR or pHR-VPR(R80A), then harvested 24, 48, and 72 h post-transduction. Cell lysates from each timepoint were subjected to Western blot analysis with polyclonal antibodies against GADD45α. In order to quantify levels of GADD45α, purified, recombinant GADD45α protein was loaded, in two-fold dilutions. (b) Primary human CD4+ lymphocytes were transduced with pHR-VPR or pHR-VPR(R80A), then harvested 48 and 72 h post-transduction. Primary cell lysates were subjected to Western blot analysis with polyclonal antibodies against GADD45α. Transduction efficiencies for both pHR-VPR and pHR-VPR(R80A) in primary CD4+ lymphocytes were between 25 and 30%, a marked reduction from efficiencies observed in SupT1 cells, which ranged from 70 to 80%. (c) SupT1 CD4+ lymphocytes were infected with either HIV-1, HIV-1-VprX, or mock treated. Once infection levels were similar, cells were harvested and subjected to Western blot analysis with polyclonal antibodies against GADD45α. Purified, recombinant GADD45α was used to estimate the fold-upregulation of GADD45α in our samples
These results prompted us to examine whether Vpr could induce upregulation of GADD45α in primary human CD4+ lymphocytes, a physiologically relevant target of HIV-1. We hypothesized that if an increase in GADD45α expression was associated Vpr-induced apoptosis, then Vpr(R80A) should not be capable of such an increase. Similar to our results in cell lines, transduction of primary human CD4+ lymphocytes with pHR-VPR resulted in marked upregulation of GADD45α protein (Figure 3b). In comparison, transduction with pHR-VPR(R80A) did not induce GADD45α upregulation above levels observed in mock-transduced lysates (Figure 3b).
As we reasoned earlier for BRCA1 phosphorylation, it is possible that overexpression of Vpr from lentiviral vectors may artificially induce stress signals that result in increased GADD45α protein. To rule out this possibility, we performed infections with HIV-1NL4-3 and HIV-1NL4-3VprX and tested the levels of GADD45α protein. We found that HIV-1NL4-3, but not HIV-1NL4-3VprX, effectively induced GADD45α upregulation (Figure 3c), similar to what we observed in SupT1 cells transduced with pHR-Vpr. These data correlate with our observation that HIV-1NL4-3, but not HIV-1NL4-3VprX, induces BRCA1 phosphorylation (Figure 2b).
Induction of GADD45α by Vpr is ATR-dependent
Although overexpression of BRCA1, a known target of ATR, has been shown to transcriptionally upregulate GADD45α,22 no functional relationship has previously been established between ATR and GADD45α. To determine whether GADD45α induction by Vpr was dependent on signaling via ATR, we asked whether knockdown of ATR would impair upregulation of GADD45α. We transfected HeLa cells with ATR siRNA or scrambled siRNA, and then transduced these cells with pHR viruses. At 48 h post-transduction, we measured GADD45α protein levels by Western blot (Figure 4). Knockdown of ATR resulted in abrogation of Vpr-induced GADD45α upregulation. As a control experiment, knockdown of GADD45α did not reduce ATR protein levels (Figure 1d). These data confirm that Vpr upregulates GADD45α via ATR and that this regulation is unidirectional.
Vpr-induced upregulation of GADD45α is ATR-dependent. HeLa cells were transfected with either nonspecific siRNA, GADD45α-specific siRNA, or ATR-specific siRNA, then mock-transduced or transduced with pHR-VPR. The cells were lysed at 48 h post-transduction and subjected to Western blot with polyclonal antibodies against GADD45α
Caspase inhibition does not abrogate Vpr-induced G2 arrest or BRCA1 phosphorylation
It has been proposed that Vpr associates with the mitochondrial PTPC and induces cytochrome c release, caspase activation, and subsequent apoptosis.10, 11 Our data suggest a model in which Vpr is activating a proapoptotic DNA damage pathway that is mediated by ATR and GADD45α and lies upstream of mitochondrial signaling. In an attempt to reconcile the apparent differences between these two models, we hypothesized that early caspase activation induced by Vpr binding to the PTPC may activate the ATR pathway. We reasoned that a low level of caspase activity could potentially lead to DNA degradation,42 which may, in turn, activate ATR. To test this hypothesis, we transduced SupT1 cells with pHR-Vpr or pHR-Vpr(R80A), then treated with a pan-caspase inhibitor (Z-VAD-FMK) for the duration of the experiment. A previous study from our group demonstrated that BOC-D-FMK, another pan-caspase inhibitor, could effectively block Vpr-induced apoptosis.3 At 48 h post-transduction, we harvested cells and measured caspase 3 activity, G2 arrest, and phosphorylation of BRCA1 at serine 1423. We found that incubation with Z-VAD-FMK (Figure 5a) had no effect on BRCA1 phosphorylation at serine 1423 (Figure 5b) or G2 arrest (Figure 5c) in the presence of Vpr.
Inhibition of caspase activity does not affect Vpr-induced G2 arrest or BRCA1 phosphorylation. (a) SupT1 CD4+ lymphocytes were incubated with Z-VAD-FMK, then either mock-treated or transduced with pHR-VPR. Cells were harvested 48 h post-transduction and stained with FITC-VAD-FMK, then subjected to flow cytometric analysis to determine the percentage of cells undergoing apoptosis, that is, staining positive for FITC-VAD-FMK. (b) SupT1 CD4+ lymphocytes were incubated with Z-VAD-FMK, then either mock-treated or transduced with pHR-VPR. Cells were harvested 48 h post-transduction and subjected to Western blot analysis with anti-BRCA1 phospho-serine 1423 antibodies. (c) SupT1 CD4+ lymphocytes were incubated with Z-VAD-FMK, then either mock-treated or transduced with pHR-VPR. Cells were harvested 48 h post-transduction and stained with propidium iodide, then subjected to flow cytometric analysis in order to characterize the percentage of cells arrested in G2/M
Induction of apoptosis by Vpr is not mediated by activation of the MAP kinases, JNK, or p38
Considering earlier reports that GADD45α activates a mitogen-activated protein kinase (MAPK) cascade culminating in Jun N-terminal kinase (JNK) activation and apoptosis,22 we decided to examine whether Vpr-induced apoptosis was associated with activation of JNK. We measured phosphorylation of c-Jun, a target of JNK, in response to Vpr. As a positive control for JNK activation, we treated cells with anisomycin. Transduction of SupT1 cells with pHR-VPR did not result in any detectable phosphorylation of c-Jun (Figure 6a). We reasoned that it is possible that Vpr activates JNK in a manner that does not result in phosphorylation of c-Jun. In order to measure JNK activation in a more direct manner, we transduced SupT1 cells with pHR-VPR, then harvested and lysed cells at 24, 48 and 72 h post-transduction. Cell lysates from each time point were subjected to Western blot with phospho-specific antibodies against JNK. In agreement with the previous data, we determined that JNK was not activated in response to Vpr (data not shown).
Vpr-induced upregulation of GADD45α does not result in activation of JNK or p38 kinase. (a) SupT1 cells were transduced with pHR-VPR. At 48 h post-transduction, cells were lysed and incubated with recombinant c-Jun. The relative levels of c-Jun phosphorylation for each treatment were determined by Western blot, using phospho-specific antibodies against c-Jun. As a positive control, cells were treated with anisomycin to induce JNK activation. (b) SupT1 cells were transduced with pHR-VPR then lysed at 24, 48, and 72 h post-transduction. VPR-induced phosphorylation of p38 kinase was determined by Western blot using a phospho-specific antibody against p38 kinase. As a positive control, cells were treated with anisomycin to induce p38 kinase activation
In view of the negative results concerning the role of JNK downstream from GADD45α, we turned our attention to p38 kinase, another member of the MAPK family implicated in apoptosis.43 We infected SupT1 cells with pHR-VPR and harvested three time points at 24, 48, and 72 h post-infection, then assayed for the presence of activated, phosphorylated p38 kinase by Western blot. We found that, as we previously observed for JNK, p38 kinase was not activated in Vpr-expressing cells (Figure 6b).
Therefore, our work conclusively demonstrates the requirement of ATR and GADD45α for Vpr-induced apoptosis, and a correlation with BRCA1 activation/phosphorylation. However, our experiments failed to identify the downstream mediators of GADD45α among two documented candidates, JNK and p38. Therefore, we hypothesize that an unsuspected cellular factor(s) may participate in GADD45α-mediated apoptosis in the context of Vpr and, perhaps, also in the context of certain forms of stress. Future investigations will be aimed at identifying downstream targets of GADD45α.
Discussion
Loss of CD4+ lymphocytes over the course of an HIV-1 infection plays a central role in disease progression and immune suppression in AIDS patients (reviewed in Hazenberg et al.44). However, the exact mechanism by which CD4+ T cells are lost is poorly understood. Several mechanisms have been proposed to explain the loss of CD4+ T cells in HIV-1-infected patients, including direct killing by HIV-1 infection, CD8+ T-cell-mediated killing of infected CD4+ lymphocytes, and apoptosis of uninfected ‘bystander’ cells. In addition, the HIV-1 proteins Tat, Rev, Vpu, Nef and Vpr have been implicated in the apoptosis of infected and/or bystander cells (reviewed in Roshal et al.34).
Since Vpr was found to be sufficient to induce apoptosis,1 the functional relationship between induction of apoptosis and that of G2 arrest has been somewhat controversial. While G2 arrest plateaus at approximately 36 h post-transduction with Vpr-expressing lentiviral vectors, apoptosis appears to be maximal at 48–72 h (Andersen and Planelles, unpublished). In addition, alleviation of cell cycle arrest with drugs such as caffeine largely eliminated induction of apoptosis.4, 45 On the other hand, mutants of Vpr have been described, which are able to dissociate both phenotypes partially.46, 47, 48, 49 The results from the present study suggest yet a different model. We propose that G2 arrest and apoptosis are induced concomitantly, since both are dependent on activation of the same kinase, ATR. However, for reasons that are not clear, apoptosis and G2 arrest develop with different kinetics, such that G2 arrest peaks first. According to this model, two different targets of ATR initiate the G2 arrest and apoptotic responses. We propose that these are CHK1 and BRCA1/GADD45α, respectively. In support of this model, siRNA-mediated knockdown of ATR effectively abrogates both responses.
Previous reports have demonstrated in vitro binding of Vpr to the PTPC, which resulted in the release of cytochrome c from fractionated mitochondria.10, 11 These observations suggest that Vpr induces mitochondrial depolarization directly rather than activating upstream stress sensors, such as ATR. The observations of Jacotot et al.11 would suggest that Vpr induces apoptosis rapidly after being expressed, while observations made with virus infection indicate that apoptosis induced by Vpr is maximal at day 3 postinfection. In addition, the model proposed by Jacotot et al. does not explain the observation that Vpr-expressing cells undergo apoptosis in a cell cycle-dependent manner, specifically from G2.39 However, it would be theoretically possible that an interaction between Vpr and the PTPC may lead to activation of the ATR/DNA damage pathway. Specifically, one may hypothesize that low-level caspase activation resulting from the Vpr–PTPC interaction might lead to DNA degradation,42 and ultimately activate ATR toward G2 arrest. We observed that treatment with caspase inhibitors in the presence of Vpr did not alter the levels of G2 arrest or the phosphorylation of BRCA1 at serine 1423 (an upstream signal leading to the commitment to apoptosis). These data suggest that caspase activation, induced at any point over the course of Vpr expression, is not the trigger of ATR or BRCA1 activation. To reconcile observations made by Jacotot et al.11 and our observations, one would have to postulate that a Vpr–PTPC interaction leads to activation of the ATR pathway via the release or activation of an uncharacterized mitochondrial factor. This possibility, although unlikely, remains open.
We have previously observed BRCA1 foci formation as a downstream consequence of G2 arrest.18 In the present study, we further demonstrate that Vpr induces ATR-dependent phosphorylation of BRCA1 at serine 1423, which is indicative of BRCA1 activation following genotoxic stress.17 Past reports have suggested a role for BRCA1 in transcriptional regulation of genes involved in cell cycle arrest, apoptosis, and DNA repair.24, 40 Specifically, overexpression of BRCA1 resulted in transcriptional upregulation of GADD45α.22, 24 We observed activation of BRCA1 concomitant with upregulation of GADD45α. It will clearly be important to determine whether upregulation of GADD45α, by Vpr, requires BRCA1. However, past attempts to downregulate BRCA1 by RNAi have proven unsuccessful in our laboratory.
The downstream signaling events from GADD45α leading to apoptosis remain uncertain. Interestingly, upregulation of GADD45α by Vpr does not result in activation of the MAP Kinases p38 or JNK.22, 50 In the context of reports from Harkin et al.22 demonstrating that overexpressed BRCA1 results in GADD45α upregulation and JNK-dependent apoptosis, our results suggest that a unique JNK- and p38-independent pathway is active in Vpr-induced apoptosis. Wang et al.51 demonstrated that GADD45α-deficient fibroblasts are capable of JNK activation following DNA damage, and wild-type fibroblasts, in response to UV radiation, showed JNK activation prior to GADD45α upregulation. These data suggest that the proapoptotic effects of GADD45α may be signaled by a pathway that circumvents activation of the MAP kinases, p38, and JNK. GADD45α is able to associate with several cellular proteins, including p21Waf1, CDC2, and the proliferating cell nuclear antigen (PCNA).28, 52, 53, 54 It will be important to establish whether any of the known GADD45α partners play a role in apoptosis induced by Vpr.
Materials and Methods
Cell lines, primary cells, and treatments
The human cervical cancer cell line, HeLa, was maintained in Dulbecco's modified Eagle's medium (DMEM) (BioWhittaker, Walkersville, MD, USA) supplemented with 10% fetal calf serum (FCS). The human T-cell line SupT1 was propagated in RPMI 1640 (BioWhittaker) supplemented with 10% FCS. Primary human CD4+ lymphocytes were first isolated in buffy coats using vacutainer cell preparation tubes according to the manufacturer's protocol (Becton Dickinson, Franklin Lakes, NJ, USA). Buffy coats were then purified further using a CD4+ isolation kit (Dynal Biotechnology, Olso, Norway) according to the manufacturer's instructions. Isolated lymphocytes were cultured in RPMI 1640 supplemented with 100 μ/ml IL-2 (National Institute of Health, AIDS research and reference reagent program, Rockville, MD, USA), 6 μg/ml phytohemaglutinin (Sigma Aldrich, St. Louis, MO, USA; L-9017), and 10% FCS, for a period of 4 days prior to transduction. Following transduction, primary lymphocytes were cultured in RPMI 1640 supplemented with 10% FCS and 100 μ/ml IL-2. SupT1 cells were incubated in 20 μM Z-VAD-FMK pan caspase inhibitor (BD Pharmingen, San Diego, CA, USA), and media with caspase inhibitor was replaced daily.
Transduction methods
SupT1 and primary CD4+ lymphocytes were transduced with virus diluted in cell culture media with 8 μg/ml polybrene. Transduction was performed as previously described,55 HeLa cells were transduced in six well plates with virus diluted into cell culture media with 10 μg/ml polybrene. After 6 h, virus was replaced with fresh culture media. Transduction efficiencies were verified by flow cytometry for each experiment to ensure that efficiencies were similar between treatments.
Western blotting procedures
All Western blots were performed using the BioRad Criterion gel system (BioRad, Hercules, CA, USA). Recombinant GADD45α protein was obtained from Santa Cruz Biotechnology, Santa Cruz, CA, USA. Antibodies used were GADD45α (Santa Cruz Biotechnology; sc-797), Actin (Santa Cruz Biotechnologies; sc-797), CHK2 (Santa Cruz Biotechnology; sc-8813), ATM (Novus Biologicals, Littleton, CO, USA; catalog #100-104H1), phospho-JNK-Tyr183 (Cell Signaling Technology, Beverly, MA, USA; catalog #9255S), phospho-p38 kinase (Promega, Madison, USA; 15823207), JNK (Cell Signaling Technology; 9252), ATR (obtained from Dr. Paul Nghiem, Harvard), anti-rabbit secondary-HRP (Santa Cruz Biotechnology; sc-2030), anti-goat secondary-HRP (Santa Cruz Biotechnology; sc-2033), PARP (Cell Signaling Technology), BRCA1 phospho ser1423 (Bethyl Laboratories, Montgomery, TX, USA). HA-tagged Vpr protein was detected with anti-HA antibodies. SupT1 cells were treated with anisomycin (Sigma Aldrich) at a concentration of 25 μg/ml for 30 min, then lysed immediately. Changes in protein levels observed by Western blot were assessed by densitometry scanning.
Immunofluorescence staining
Cells were harvested 48 h post-transduction by trypsinization. Cells were then fixed in 2% paraformadehyde in phosphate-buffered saline (PBS) for 35 min at 4°C then washed 3 times for 5 min in PBS. All subsequent steps were carried out at room temperature. Samples were then blocked and permeabilized for 20 min in blocking buffer (3% bovine serum albumin (BSA), 0.2% Triton X-100, 0.01% skim milk in PBS). Primary antibody rabbit anti-BRCA1 (Bethyl Laboratories) was diluted 1 : 400 in incubation buffer (1% BSA, 0.02% Triton X-100 in PBS) and incubated on cells for 45 min. Cells were then washed with PBS, after which secondary antibody (goat anti-rabbit IgG-AlexaFluor568-conjugate; Molecular Probes, Eugene, OR, USA) was applied for 35 min diluted 1 : 500 in incubation buffer. Cells were then washed with PBS as before and mounted on glass slides using FluorSave reagent (CalBiochem, San Diego, CA, USA). Cells were then visualized for γ-H2AX immunostaining and GFP expression by scanning fluorescence confocal microscopy (FluoView FV300, Olympus, Melville, NY, USA).
Apoptosis assays
Cells were fixed in 2% paraformaldehyde (in PBS) for 15 min at room temperature. Fixed cells were then permeabilized in 0.1% Triton X-100 (in PBS) for 15 min at room temperature, then washed 2 times in PBS and incubated in 0.5 μg/ml 4′,6-diamidino-2-phenylindole, dihydrochloride (DAPI) (Molecular Probes) dissolved in PBS, for 45 min at 37°C. DAPI-treated cells were then analyzed by fluorescence microscopy. Random fields were chosen throughout the dish and apoptotic cells were marked by the presence of fragmented nuclei. Total apoptotic cells from three independent experiments were counted and divided by the total cell number to obtain a percentage of apoptotic cells for each treatment with standard deviations. A minimum of 1000 cells were counted per treatment/per experiment. PARP cleavage was assayed by Western blot as described above. SupT1 cells were stained with CaspACE-FITC (FITC-VAD-FMK) according to manufacturers protocol (Promega, Madison, WI, USA).
SiRNA treatments
All siRNA treatments were performed with Dharmacon smart pool siRNA duplexes: GADD45α (Dharmacon, Lafeyette, CO, USA; M-003893-00), ATR (Dharmacon; M-003202-01), ATM (Dharmacon; M-003201-01), CHK2 (Dharmacon; M-003256-03), and scrambled siRNA (Dharmacon; D-001206-13-05). Smart pool siRNAs were transfected at a final concentration of 100 nm into exponentially growing HeLa cells with oligofectamine (Invitrogen, Carlsbad, CA, USA), all according to the manufacturer's protocols.
In vitro kinase assay
SupT1 cells were infected with pHR-VPR and as a VPR-minus control, pHR-GFP, then lysed at 48 h post-transduction with supplied lysis buffer. JNK kinase activity was measured with the SAPK/JNK nonradioactive assay kit (Cell Signaling Technology), according to the manufacturer's protocol.
Note added in proof
Coberley et al. reported recently that BRCA1 and GADD45 are upregulated in macrophages infected with HIV-1 (reference56).
Abbreviations
- GADD45α:
-
growth arrest and DNA damage-45 alpha
- Vpr:
-
viral protein R
- BRCA1:
-
breast cancer-associated-1 gene
- ATM:
-
ataxia telangiectasia-mutated
- ATR:
-
ATM- and Rad3-related
- CHK2:
-
checkpoint kinase-2
- HIV-1:
-
human immunodeficiency virus type-1
- PTPC:
-
permeability transition pore complex
- PLK1:
-
polo-like kinase-1
- CHK1:
-
checkpoint kinase-1
- H2AX:
-
histone 2A variant-X
- 53BP1:
-
p53-binding protein-1
- JNK/SAPK:
-
c-jun N-terminal kinase/stress-activated protein kinase
- PARP:
-
poly(ADP-ribose) polymerase
References
Stewart SA, Poon B, Jowett JB and Chen IS (1997) Human immunodeficiency virus type 1 Vpr induces apoptosis following cell cycle arrest. J. Virol. 71: 5579–5592
Bartz SR, Rogel ME and Emerman M (1996) Human immunodeficiency virus type 1 cell cycle control: Vpr is cytostatic and mediates G2 accumulation by a mechanism which differs from DNA damage checkpoint control. J. Virol. 70: 2324–2331
Shostak LD, Ludlow J, Fisk J, Pursell S, Rimel BJ, Nguyen D, Rosenblatt JD and Planelles V (1999) Roles of p53 and caspases in the induction of cell cycle arrest and apoptosis by HIV-1 vpr. Exp. Cell Res. 251: 156–165
Zhu Y, Gelbard HA, Roshal M, Pursell S, Jamieson BD and Planelles V (2001) Comparison of cell cycle arrest, transactivation, and apoptosis induced by the simian immunodeficiency virus SIVagm and human immunodeficiency virus type 1 vpr genes. J. Virol. 75: 3791–3801
Gandhi RT, Chen BK, Straus SE, Dale JK, Lenardo MJ and Baltimore D (1998) HIV-1 directly kills CD4+ T cells by a Fas-independent mechanism. J. Exp. Med. 187: 1113–1122
Shaw GM, Hahn BH, Arya SK, Groopman JE, Gallo RC and Wong-Staal F (1984) Molecular characterization of human T-cell leukemia (lymphotropic) virus type III in the acquired immune deficiency syndrome. Science 226: 1165–1171
Fauci AS (1988) The human immunodeficiency virus: infectivity and mechanisms of pathogenesis. Science 239: 617–622
Zagury D, Bernard J, Leonard R, Cheynier R, Feldman M, Sarin PS and Gallo RC (1986) Long-term cultures of HTLV-III-infected T cells: a model of cytopathology of T-cell depletion in AIDS. Science 231: 850–853
Muthumani K, Hwang DS, Desai BM, Zhang D, Dayes N, Green DR and Weiner DB (2002) HIV-1 Vpr induces apoptosis through caspase 9 in T cells and peripheral blood mononuclear cells. J. Biol. Chem. 277: 37820–37831
Vieira HL, Haouzi D, El Hamel C, Jacotot E, Belzacq AS, Brenner C and Kroemer G (2000) Permeabilization of the mitochondrial inner membrane during apoptosis: impact of the adenine nucleotide translocator. Cell Death Differ. 7: 1146–1154
Jacotot E, Ravagnan L, Loeffler M, Ferri KF, Vieira HL, Zamzami N, Costantini P, Druillennec S, Hoebeke J, Briand JP, Irinopoulou T, Daugas E, Susin SA, Cointe D, Xie ZH, Reed JC, Roques BP and Kroemer G (2000) The HIV-1 viral protein R induces apoptosis via a direct effect on the mitochondrial permeability transition pore. J. Exp. Med. 191: 33–46
Roshal M, Kim B, Zhu Y, Nghiem P and Planelles V (2003) Activation of ATR-mediated DNA damage response by the HIV-1 viral protein R. J. Biol. Chem. 278: 25879–25886
Liu Q, Guntuku S, Cui XS, Matsuoka S, Cortez D, Tamai K, Luo G, Carattini-Rivera S, DeMayo F, Bradley A, Donehower LA and Elledge SJ (2000) Chk1 is an essential kinase that is regulated by Atr and required for the G(2)/M DNA damage checkpoint. Genes Dev. 14: 1448–1459
Abraham RT (2001) Cell cycle checkpoint signaling through the ATM and ATR kinases. Genes Dev. 15: 2177–2196
Yang J, Xu ZP, Huang Y, Hamrick HE, Duerksen-Hughes PJ and Yu YN (2004) ATM and ATR: sensing DNA damage. World J. Gastroenterol. 10: 155–160
Zou L, Cortez D and Elledge SJ (2002) Regulation of ATR substrate selection by Rad17-dependent loading of Rad9 complexes onto chromatin. Genes Dev. 16: 198–208
Tibbetts RS, Cortez D, Brumbaugh KM, Scully R, Livingston D, Elledge SJ and Abraham RT (2000) Functional interactions between BRCA1 and the checkpoint kinase ATR during genotoxic stress. Genes Dev. 14: 2989–3002
Zimmerman ES, Chen J, Andersen JL, Ardon O, DeHart JL, Blackett J, Choudhary S, Camerini D, Nghiem P and Planelles V (2004) HIV-1 Vpr mediated G2 arrest requires Rad17 and Hus1 and induces nuclear BRCA1 and gamma H2AX foci formation. Mol. Cell Biol. 24: 9286–9294
Stewart SA, Poon B, Jowett JB, Xie Y and Chen IS (1999) Lentiviral delivery of HIV-1 Vpr protein induces apoptosis in transformed cells. Proc. Natl. Acad. Sci. USA 96: 12039–12043
Scully R and Livingston DM (2000) In search of the tumour-suppressor functions of BRCA1 and BRCA2. Nature 408: 429–432
Xu X, Weaver Z, Linke SP, Li C, Gotay J, Wang XW, Harris CC, Ried T and Deng CX (1999) Centrosome amplification and a defective G2-M cell cycle checkpoint induce genetic instability in BRCA1 exon 11 isoform-deficient cells. Mol. Cell 3: 389–395
Harkin DP, Bean JM, Miklos D, Song YH, Truong VB, Englert C, Christians FC, Ellisen LW, Maheswaran S, Oliner JD and Haber DA (1999) Induction of GADD45 and JNK/SAPK-dependent apoptosis following inducible expression of BRCA1. Cell 97: 575–586
Cortez D, Wang Y, Qin J and Elledge SJ (1999) Requirement of ATM-dependent phosphorylation of brca1 in the DNA damage response to double-strand breaks. Science 286: 1162–1166
MacLachlan TK, Takimoto R and El-Deiry WS (2002) BRCA1 directs a selective p53-dependent transcriptional response towards growth arrest and DNA repair targets. Mol. Cell Biol. 22: 4280–4292
Fornace Jr AJ, Alamo Jr I and Hollander MC (1988) DNA damage-inducible transcripts in mammalian cells. Proc. Natl. Acad. Sci. USA 85: 8800–8804
Kastan MB, Zhan Q, el-Deiry WS, Carrier F, Jacks T, Walsh WV, Plunkett BS, Vogelstein B and Fornace Jr AJ (1992) A mammalian cell cycle checkpoint pathway utilizing p53 and GADD45 is defective in ataxia-telangiectasia. Cell 71: 587–597
Papathanasiou MA, Kerr NC, Robbins JH, McBride OW, Alamo Jr I, Barrett SF, Hickson ID and Fornace Jr AJ (1991) Induction by ionizing radiation of the gadd45 gene in cultured human cells: lack of mediation by protein kinase C. Mol. Cell Biol. 11: 1009–1016
Zhan Q, Antinore MJ, Wang XW, Carrier F, Smith ML, Harris CC and Fornace Jr AJ (1999) Association with Cdc2 and inhibition of Cdc2/cyclin B1 kinase activity by the p53-regulated protein Gadd45. Oncogene 18: 2892–2900
Jin S, Antinore MJ, Lung FD, Dong X, Zhao H, Fan F, Colchagie AB, Blanck P, Roller PP, Fornace Jr AJ and Zhan Q (2000) The GADD45 inhibition of Cdc2 kinase correlates with GADD45-mediated growth suppression. J. Biol. Chem. 275: 16602–16608
Bernstein C, Bernstein H, Payne CM and Garewal H (2002) DNA repair/pro-apoptotic dual-role proteins in five major DNA repair pathways: fail-safe protection against carcinogenesis. Mutat. Res. 511: 145–178
Foray N, Marot D, Gabriel A, Randrianarison V, Carr AM, Perricaudet M, Ashworth A and Jeggo P (2003) A subset of ATM- and ATR-dependent phosphorylation events requires the BRCA1 protein. EMBO J. 22: 2860–2871
Sampath D, Rao VA and Plunkett W (2003) Mechanisms of apoptosis induction by nucleoside analogs. Oncogene 22: 9063–9074
Yamane K, Wu X and Chen J (2002) A DNA damage-regulated BRCT-containing protein, TopBP1, is required for cell survival. Mol. Cell Biol. 22: 555–566
Roshal M, Zhu Y and Planelles V (2001) Apoptosis in AIDS. Apoptosis 6: 103–116
Soldani C, Bottone MG, Pellicciari C and Scovassi AI (2001) Two-color fluorescence detection of poly (ADP-Ribose) polymerase-1 (PARP-1) cleavage and DNA strand breaks in etoposide-induced apoptotic cells. Eur. J. Histochem. 45: 389–392
Soldani C, Lazze MC, Bottone MG, Tognon G, Biggiogera M, Pellicciari CE and Scovassi AI (2001) Poly(ADP-ribose) polymerase cleavage during apoptosis: when and where? Exp. Cell Res. 269: 193–201
Gatei M, Zhou BB, Hobson K, Scott S, Young D and Khanna KK (2001) Ataxia telangiectasia mutated (ATM) kinase and ATM and Rad3 related kinase mediate phosphorylation of Brca1 at distinct and overlapping sites. In vivo assessment using phospho-specific antibodies. J. Biol. Chem. 276: 17276–17280
Adachi A, Gendelman HE, Koenig S, Folks T, Willey R, Rabson A and Martin MA (1986) Production of acquired immunodeficiency syndrome-associated retrovirus in human and non-human cells transfected with an infectious molecular clone. J. Virol. 59: 284–291
Jowett JB, Planelles V, Poon B, Shah NP, Chen ML and Chen IS (1995) The human immunodeficiency virus type 1 vpr gene arrests infected T cells in the G2 + M phase of the cell cycle. J. Virol. 69: 6304–6313
MacLachlan TK, Somasundaram K, Sgagias M, Shifman Y, Muschel RJ, Cowan KH and El-Deiry WS (2000) BRCA1 effects on the cell cycle and the DNA damage response are linked to altered gene expression. J. Biol. Chem. 275: 2777–2785
Gaynor EM and Chen IS (2001) Analysis of apoptosis induced by HIV-1 Vpr and examination of the possible role of the hHR23A protein. Exp. Cell Res. 267: 243–257
Enari M, Sakahira H, Yokoyama H, Okawa K, Iwamatsu A and Nagata S (1998) A caspase-activated DNase that degrades DNA during apoptosis, and its inhibitor ICAD. Nature 391: 43–50
Oh-Hashi K, Maruyama W and Isobe K (2001) Peroxynitrite induces GADD34, 45, and 153 VIA p38 MAPK in human neuroblastoma SH-SY5Y cells. Free Radic. Biol. Med. 30: 213–221
Hazenberg MD, Hamann D, Schuitemaker H and Miedema F (2000) T cell depletion in HIV-1 infection: how CD4+ T cells go out of stock. Nat. Immunol. 1: 285–289
Andersen JL and Planelles V (2005) The role of Vpr in HIV-1 pathogenesis. Curr. HIV Res., in press
Waldhuber MG, Bateson M, Tan J, Greenway AL and McPhee DA (2003) Studies with GFP-Vpr fusion proteins: induction of apoptosis but ablation of cell-cycle arrest despite nuclear membrane or nuclear localization. Virology 313: 91–104
Nishizawa M, Kamata M, Mojin T, Nakai Y and Aida Y (2000) Induction of apoptosis by the Vpr protein of human immunodeficiency virus type 1 occurs independently of G(2) arrest of the cell cycle. Virology 276: 16–26
Lum JJ, Cohen OJ, Nie Z, Weaver JG, Gomez TS, Yao XJ, Lynch D, Pilon AA, Hawley N, Kim JE, Chen Z, Montpetit M, Sanchez-Dardon J, Cohen EA and Badley AD (2003) Vpr R77Q is associated with long-term nonprogressive HIV infection and impaired induction of apoptosis. J. Clin. Invest. 111: 1547–1554
Somasundaran M, Sharkey M, Brichacek B, Luzuriaga K, Emerman M, Sullivan JL and Stevenson M (2002) Evidence for a cytopathogenicity determinant in HIV-1 Vpr. Proc. Natl. Acad. Sci. USA 99: 9503–9508
Mita H, Tsutsui J, Takekawa M, Witten EA and Saito H (2002) Regulation of MTK1/MEKK4 kinase activity by its N-terminal autoinhibitory domain and GADD45 binding. Mol. Cell. Biol. 22: 4544–4555
Wang X, Gorospe M and Holbrook NJ (1999) gadd45 is not required for activation of c-Jun N-terminal kinase or p38 during acute stress. J. Biol. Chem. 274: 29599–29602
Kearsey JM, Coates PJ, Prescott AR, Warbrick E and Hall PA (1995) Gadd45 is a nuclear cell cycle regulated protein which interacts with p21Cip1. Oncogene 11: 1675–1683
Smith ML, Chen IT, Zhan Q, Bae I, Chen CY, Gilmer TM, Kastan MB, O'Connor PM and Fornace Jr AJ (1994) Interaction of the p53-regulated protein Gadd45 with proliferating cell nuclear antigen. Science 266: 1376–1380
Chen IT, Smith ML, O'Connor PM and Fornace Jr AJ (1995) Direct interaction of Gadd45 with PCNA and evidence for competitive interaction of Gadd45 and p21Waf1/Cip1 with PCNA. Oncogene 11: 1931–1937
O'Doherty U, Swiggard WJ and Malim MH (2000) Human immunodeficiency virus type 1 spinoculation enhances infection through virus binding. J. Virol. 74: 10074–10080
Coberley CR, Kohler JJ, Brown JN, Oshier JT, Baker HV and Popp MP (2004) Impact on genetic networks in human macrophages by a CCR5 strain of human immunodeficiency virus type 1. J. Virol. 78: 11477–11486
Acknowledgements
We thank Dr. Wayne Green, Todd Kinard, and Michael Blackwell for excellent technical help. We are grateful to Dr. Paul Nghiem for providing antibodies to ATR. This work was supported by an NIH research grant to VP (R01AI49057).
Author information
Authors and Affiliations
Corresponding author
Additional information
Edited by W El-Deiry
Supplementary Information accompanies the paper on Cell Death and Diffrentiation website (http://www.nature.com/cdd)
Supplementary information
Rights and permissions
About this article
Cite this article
Andersen, J., Zimmerman, E., DeHart, J. et al. ATR and GADD45α mediate HIV-1 Vpr-induced apoptosis. Cell Death Differ 12, 326–334 (2005). https://doi.org/10.1038/sj.cdd.4401565
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.cdd.4401565
Keywords
This article is cited by
-
Upregulation of GADD45α in light-damaged retinal pigment epithelial cells
Cell Death Discovery (2016)
-
BRCA1 functions as a novel transcriptional cofactor in HIV-1 infection
Virology Journal (2015)
-
How SLX4 cuts through the mystery of HIV-1 Vpr-mediated cell cycle arrest
Retrovirology (2014)
-
Cellular phenotype impacts human immunodeficiency virus type 1 viral protein R subcellular localization
Virology Journal (2011)
-
Mesenchymal stem cell derived hematopoietic cells are permissive to HIV-1 infection
Retrovirology (2011)