Abstract
Orthotopic liver transplantation, by eliminating the major site of amyloidogenic protein synthesis, is currently the only definitive treatment of most hereditary amyloidoses. Because of the minimal parenchymal involvement, the explanted livers from familial amyloidotic polyneuropathy (FAP) patients have been transplanted into non-FAP patients in a “domino” fashion. The aim of this study was to evaluate the extent of amyloid deposits in explanted livers from two patients with apolipoprotein A-I amyloidosis, with the Arg26 mutation, to determine their suitability as domino donors. A detailed histologic review of the explanted livers from two patients was performed and assessed for the extent of amyloid deposition by routine and Congo red stains. Both patients had identical histopathologic features. The liver parenchymal involvement was strikingly severe. Large patches of amyloid separated hepatic cords, with accentuation around the central veins. All portal triads were consistently and markedly involved with amorphous eosinophilic deposits within the connective tissue compressing the bile ducts and vascular structures. Hilar vessels had patchy deposits. No involvement of hilar nerve branches was seen. The hepatic parenchyma is extensively involved in hereditary Apolipoprotein A-I amyloidosis, with the Arg26 mutation. These livers, removed at orthotopic liver transplantation, are not suitable for domino donation.
Similar content being viewed by others
INTRODUCTION
Orthotopic liver transplantation (OLT) is currently employed for a multitude of genetic errors of metabolism (1, 2). The liver, which appears normal but is usually the site of the abnormal protein synthesis, is removed and replaced by a new liver capable of producing the nonmutant form of the same protein, and this slows the progression of the disease. In a previous study, we confirmed that explanted livers from patients with familial amyloidotic polyneuropathy (FAP) associated with transthyretin (TTR) mutations were histologically normal livers (3). These livers with intact hepatic synthetic functions, in our opinion, were considered suitable for transplantation into other nonamyloidotic patients in a “domino” fashion; in other words, the liver, resected at OLT, from the FAP patient is transplanted into a second patient who has end-stage liver disease and is in need of synthetic and metabolic liver functions. The long period required for the mutated amyloidogenic protein to cause symptomatic amyloidosis is in all probability more than the remaining life span of the “domino” recipient, thus, making this domino-style donation an acceptable and justifiable therapeutic option.
During routine pathologic evaluation of explanted livers from two patients (sisters) with familial amyloidosis, it was evident that their histologic features were strikingly different from those reported by us in TTR-related FAP. This was further corroborated by the detection of a different genetic mutation in this family involving a change from glycine to arginine at Position 26 in the Apolipoprotein A-I (Apo A-I) protein (Arg26) and not TTR (4).
Our aims are to describe the pathologic features seen in the native livers and other tissues removed from these patients at OLT and to determine the suitability of the resected livers as domino-style donors.
CLINICAL HISTORIES
Case 1 (LT506)
The patient was first diagnosed with renal insufficiency in January 1996 at the age of 57 years. The clinical diagnosis of polycystic renal disease was ruled out by ultrasound examination revealing small, noncystic kidneys. The patient’s father had died of chronic renal disease of unknown etiology at the age of 42 years. Her cousin had died at the age of 43 years with renal disease and hepatic failure (4). The latter had been diagnosed with familial apolipoprotein A-I amyloidosis at the Amyloid Treatment and Research Program at Boston Medical Center. All affected family members had the same glycine to arginine mutation at Position 26 in the Apo A-I protein. A diagnosis of familial nephropathic systemic amyloidosis was made. The results of a neurologic examination at this time were essentially unremarkable. The liver function test results were normal, and liver biopsy showed trace positivity for amyloid by special stains. A combined liver and kidney transplantation was advised, with an attempt to halt the progression of the inherited metabolic disorder and gain improvement in renal function. During the work-up, a 1-cm, tubular-type, infiltrating ductal carcinoma of the breast was detected and was treated with lumpectomy, followed by radiation and chemotherapy.
The patient underwent combined liver and kidney transplantations in April 1999 after a 2-year cancer-free interval. The posttransplant course was complicated by thrombotic occlusion of renal graft artery, necessitating a transplant nephrectomy and return to hemodialysis.
Case 2 (LT 512)
This patient, the younger sister of the patient in Case 1, was diagnosed in June 1996, at the age of 50 years, with the presence of the mutant Arg26 Apo A-I protein during the evaluation of the family at the Amyloid Treatment and Research Program at Boston Medical Center. During the work-up, the patient was found to have slightly increased blood pressure and a creatinine level of 2.0 mg/dL. A right nephrectomy for a 5-cm papillary renal cell carcinoma was performed in July 1996, the carcinoma having been incidentally discovered during the evaluation. The resected kidney had medullary deposition of amyloid and focal glomerulosclerosis with tubular atrophy. It is possible that not only amyloid deposition but also hypertensive changes may have played a role in the patient’s renal insufficiency. No other gastrointestinal, neurological, or liver function abnormalities were noted.
The patient underwent combined liver and kidney transplantations in June 1999 after a 2-year cancer-free clinical course. Her posttransplant course was uneventful.
PATHOLOGIC EVALUATION
Case 1 (LT 506)
The explanted liver measured 24.5 × 20 × 6 cm and had a dark red, tan cut surface. No masses, nodules, nor evidence of cirrhosis were noted. The attached gallbladder contained multiple stones. A 0.6 × 0.4 × 0.1-cm segment of vagus nerve without definite thickening was also submitted to the pathology laboratory for examination.
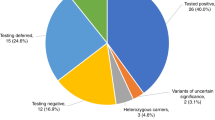
Histologically, the liver parenchymal involvement was striking (Fig. 1). Large patches of amyloid, confirmed by apple-green birefringence on Congo red–stained tissue sections replaced the hepatic lobular areas (Fig. 2). Thick subsinusoidal columns of amyloid separated hepatic cords, with accentuation around the central veins. All portal triads were markedly involved with amorphous, eosinophilic deposits within the connective tissue, which compressed the bile ducts and vascular structures. The hilar vessels had patchy amyloid deposits within their walls. No involvement of hilar nerve branches or vagus nerve was seen. Hilar soft tissues also had amyloid deposits.
Congo-red–stained section (medium power) from a slightly less involved liver parenchyma. Congophilic material in portal connective tissue is seen in a nodular configuration compressing the portal structures. In addition, congophilic material is seen surrounding the hepatic cords diffusely within the lobules. Under polarized light, bright apple-green birefringence was noted.
Case 2 (LT512)
The explanted liver measured 23 × 15 × 7 cm and had a musky, dark, and somewhat variegated cut surface. No masses, nodules, nor evidence of cirrhosis were noted. The patient’s gallbladder and segment of vagus nerve were not included in the specimen.
Microscopically, the features were identical to those observed in Case 1. There were abundant amyloid deposits within the liver and hilar soft tissues. The hilar nerve branches were free of amyloid deposition.
DISCUSSION
Amyloidosis is characterized by systemic deposition of β-pleated protein fibrils. Hereditary amyloidosis is associated with mutations in TTR, fibrinogen, gelsolin, lysozyme, and Apo A-I genes (5). Apo A-I is the major protein constituent of plasma high-density lipoproteins (HDL) and is synthesized in the liver and intestines in approximately the same proportions (6). Decreased plasma levels of HDL due to a lack of normal Apo A-I are associated with an increased risk of atherosclerotic cardiovascular disease (7).
Many centers have elected OLT to treat patients with FAP because over 98% of the mutant TTR, the amyloidogenic protein, is synthesized in the liver (3). The preliminary results give cause for optimism because serum mutant TTR levels drop with slowing down in disease progression, but demonstrable improvement in peripheral neuropathy or cardiomyopathy have not been observed (8, 9, 10). On the basis of similar rationale as in the case of FAP patients, two sisters with mutant Apo A-I–associated amyloidosis underwent a novel treatment, which has not been published in the literature, of combined liver and kidney transplantations at our institutions. The intent was to replace the liver-derived mutant Apo A-I with normal Apo A-I and thus slow the amyloid deposition and possibly decrease the risk of accelerated atherosclerosis. These patients needed renal transplants additionally because of the nephropathic nature of their disease.
In a previous study, we showed that the explanted livers from FAP patients with TTR mutations are both histologically and functionally normal and can be transplanted into nonamyloidotic patients (domino-style donor livers; 3). The two patients in our current report, although they had normal liver function tests before OLT and grossly (deceptively) unremarkable livers, had extensive microscopic parenchymal amyloid deposits. With the progression of the disease, these patients were bound to have liver insufficiency. Our patients had extensive involvement of the hepatic parenchyma, and it was likely to progress if transplanted into other nonamyloidotic patients. Therefore, we feel that livers from patients with Apo A-I mutations are not suitable for domino-style donation. These livers also may not be suitable because of the synthesis of a mutant Apo A-I protein, which may lower the HDL levels in the recipients and cause atherosclerotic cardiovascular disease.
At least four different mutations of Apo A-I are known to be amyloidogenic (5). These disorders are autosomal dominant, with various clinical presentations. One mutation found in an Iowa family consisted of a point mutation with replacement of glycine to arginine at Position 26, the same mutation seen in both of our patients (7). The clinical presentation of the affected patients from the Iowa family included neuropathy, peptic ulcer disease, and nephropathy with decreased plasma levels of HDL and Apo A-I. Although our patients’ family has the same mutation in Apo A-I as the Iowa family, the Arg26 mutation, the clinical disease is different, nephropathy being the predominant presentation without any neurologic or gastrointestinal complaints. Our patients’ father and cousin (proband) both died of chronic renal failure at a young age. Liver dysfunction was severe in the cousin after a kidney transplant. Both our patients had varying degrees of renal dysfunction at the time of diagnosis. It is possible that their renal disease may be related to hypertension and accelerated atherosclerosis because of abnormalities in lipid metabolism resulting from the inherited disorder of Apo A-I. If the predominant nephropathy in our family is not entirely due to amyloid deposits but is also related to decreased levels of HDL, then an early intervention with OLT may indeed obviate the need for a concurrent renal transplant. This may be an important consideration because there are younger members with the same genetic mutation within this extended family.
Some forms of Apo A-I–associated amyloidosis have been referred to as FAP Type III or Type IV, which is somewhat confusing and probably does not represent the same disease as seen in this family. Perhaps it is best to subclassify the various forms of hereditary amyloidoses according to their genetic mutations. In our literature review of Apo A-I–associated hereditary amyloidoses, it is apparent that the disease and pattern of amyloid deposition varies with different genetic mutations and within different families with the same mutation. It is therefore prudent to examine the liver biopsy of the first patient from a family with hereditary amyloidosis, before domino-style liver donation is contemplated from other members of the same family undergoing OLT.
To summarize, we report here on the first detailed histopathologic evaluation of the liver involvement in one subset (Arg26) of Apo A-I amyloidosis. On the basis of our findings, we conclude that explanted livers from these patients are unsuitable for domino-style donation.
References
Pratschke J, Steinmuller T, Bechstein WO, Neuhaus R, Tullius SG, Jonas S, et al. Orthotopic liver transplantation for hepatic associated metabolic disorders. Clin Transpl 1998; 12: 228–232.
Mowat AP . Orthotopic liver transplantation in liver-based metabolic disorders. Eur J Pediatr 1992; 152 (1 Suppl): S32–S38.
Shaz BH, Gordon F, Lewis WD, Jenkins RL, Skinner M, Khettry U . Orthotopic liver transplantation for familial amyloidotic polyneuropathy: a pathologic study. Hum Pathol 2000; 31: 40–44.
Jones LA, Harding JA, Cohen AS, Skinner M . New USA family has apolipoprotein A-I (Arg 26) variant. In: Natvig JB, Forre O, Husby G, Husabekk A, Skogen B, Sletten K, et al., editors. Amyloid and amyloidosis. Dordrecht, Netherlands: Kluwer Academic; 1990. p. 385–388.
Genschel J, Haas R, Propsting MJ, Schmidt HH . Apolipoprotein A-I induced amyloidosis. FEBS Lett 1998; 430: 145–149.
Booth DR, Tan SY, Booth SE, Tennent GA, Hutchinson WL, Hsuan JJ, et al. Hereditary hepatic and systemic amyloidosis caused by a new deletion/insertion mutation in the apolipoprotein AI gene. J Clin Invest 1996; 97: 2714–2721.
Rader DJ, Gregg RE, Meng MS, Schaefer JR, Zech LA, Benson MD, et al. In vivo metabolism of a mutant apolipoprotein, apoA-IIowa, associated with hypoalphalipoproteinemia and hereditary systemic amyloidosis. J Lipid Res 1992; 33: 755–763.
Pomfret EA, Lewis WD, Jenkins RL, Bergethon P, Dubrey SW, Reisinger J, et al. Effect of orthotopic liver transplantation on the progression of familial amyloidotic polyneuropathy. Transplantation 1998; 65: 918–925.
Parrilla P, Ramirez P, Bueno FS, Robles R, Acosta F, Miras M, et al. Clinical improvement after liver transplantation for type I familial amyloid polyneuropathy. Br J Surg 1995; 82: 825–828.
Suhr OB, Wiklund U, Ando Y, Ando E, Olofsson BO . Impact of liver transplantation on autonomic neuropathy in familial amyloidotic polyneuropathy: an evaluation by spectral analysis of heart rate variability. J Intern Med 1997; 242: 225–229.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented in part at the United States and Canadian Academy of Pathology Meeting, New Orleans, LA, March, 2000.
Rights and permissions
About this article
Cite this article
Shaz, B., Lewis, W., Skinner, M. et al. Livers from Patients with Apolipoprotein A-I Amyloidosis Are Not Suitable as “Domino” Donors. Mod Pathol 14, 577–580 (2001). https://doi.org/10.1038/modpathol.3880353
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3880353