Abstract
The expression of p27Kip1, a negative regulator of the cell cycle, has been reported to correlate with the biological behavior and prognosis of several tumors. However, its prognostic importance in transitional cell carcinoma of the upper urinary tract (TCC-UUT) has not previously been investigated. We investigated p27Kip1 protein expression using immunohistochemistry in 132 cases of TCC-UUT and also its relation to proliferating cell nuclear antigen (PCNA) immunoreactivity, p53 oncoprotein immunoreactivity, clinicopathologic parameters, and clinical outcome. A positive expression of p27Kip1 protein was recognized in 94.7% of the samples and was apparent within tumor nuclei. In the normal urothelium, its expression was identified in all cell layers. A positive expression of p53 oncoprotein was recognized in 27.2% of the patients. The PCNA index was 7.4 to 93.1% (mean, 66.4%). Examination of the relationships between the expression of p27Kip1 protein and clinicopathologic findings, PCNA index, and the expression of p53 oncoprotein revealed that the expression of p27Kip1 protein decreased significantly with stage and grade. In a univariate analysis of disease-free and overall survival rates, no correlation was found between the expression of p27Kip1 protein and prognosis. The expression of p27Kip1 protein appears to be of little or no value in informing the prognosis in TCC-UUT.
Similar content being viewed by others
INTRODUCTION
Cyclins and cyclin-dependent kinase (CDK) complexes, which play important regulatory roles during cell cycle progression (1, 2, 3), are negatively regulated by CDK inhibitors. These inhibitors are assigned to two families on the basis of their structural and functional properties. The members of the INK4 family—such as p16INK4a, p15INK4b, p18INK4c, and p19INK4d—each have four ankyrin repeats and form complexes with CDK and/or CDK6 and the D-type cyclins. The members of the second group of CDK inhibitors, the Cip/Kip family—which includes p21Cip/waf1, p27Kip1, and p57Kip2—each have an homologous amino terminal domain containing contiguous cyclin- and CDK-binding regions.
The Cip/Kip family member p27Kip1 regulates progression from G1 into S phase by binding and inhibiting the cyclin E/CDK2 complex necessary for entry into S phase (2, 3, 4). p27Kip1 is present in large amounts in quiescent cells but has been found to be decreased in malignant tumors. Furthermore, a low expression of p27Kip1 protein has been found to be associated with tumor aggressiveness and an unfavorable prognosis in several cancers, including those of the urinary bladder (5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16). In transitional cell carcinoma of the upper urinary tract (TCC-UUT), however, the expression of p27Kip1 protein has not been examined for its clinical significance in predicting survival.
As a CDK inhibitor, p27Kip1 has been considered to be a potential candidate for a tumor suppressor gene. p53, a known tumor suppressor gene, is thought to regulate cell growth and proliferation, and mutations in the p53 gene have been reported in a variety of human tumors, including approximately 40 to 60% of muscle-invasive bladder carcinomas (17, 18, 19). In response to genotoxic stress, wild-type p53 protein is up-regulated and either induces growth arrest in G1 or triggers cell death. The current study, using an immunohistochemical approach to examine formalin-fixed, paraffin-embedded, tumor-tissue sections from 132 patients with TCC-UUT, was aimed at ascertaining whether p27Kip1 is expressed in such sections and whether its expression shows any correlation with a variety of clinicopathologic findings, with proliferating cell nuclear antigen (PCNA) immunoreactivity, with the immunoreactivity for p53 oncoprotein, and/or with clinical outcome in such patients.
MATERIALS AND METHODS
The material used comprised 132 surgically resected specimens from patients with primary TCC-UUT that had been obtained at the Mutual Aid Associations' Hospital, Tachikawa, Japan, and the National Defense Medical College Hospital, Tokorozawa, Japan, between 1970 and 1995. Their histopathologic stage was determined according to the criteria proposed by the International Union Against Cancer (20). Tumor cells were divided histopathologically into two grades using the criteria for urinary bladder tumors of the Armed Forces Institute of Pathology (21).
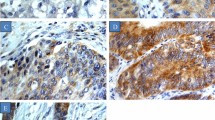
For immunohistochemistry, we used the catalyzed signal amplification system method (DAKO, Glostrup, Denmark) on deparaffinized sections, employing mouse monoclonal antibodies against p27Kip1 protein (Tranduction Laboratories, Lexington, KY) diluted 1:100. Autoclave pretreatment in 0.1 m citrate buffer, pH 6.0, was performed for 15 minutes at 120°C. For the negative control, the incubation step with the primary antibody was omitted. Cells were considered positive when distinct nuclear staining was identified. The extent of staining was scored as low expression, indicating <50% of tumor area stained, or high expression, indicating ≥50% stained. The evaluation was performed twice by one investigator (KN), who was blind to the tumor stage and grade.
For the analysis of PCNA and on the basis of the immunoreaction in ≥1000 tumor cells, the percentage of nuclei exhibiting a positive immunoreaction (PCNA index) was determined as previously described (22). The PCNA index was classified as high if it was ≥69%, a figure representing the median value for the carcinomas. p53 oncoprotein was evaluated immunohistochemically; the technique used and the results obtained in these same patients have been reported elsewhere (23).
In the statistical analysis, disease-free and overall survival rates were the two main dependent variables tested in this study. Disease-free survival was defined as the period between the initial radical operation and the subsequent appearance of recurrence or metastasis. Recurrence was defined as transitional cell carcinoma (TCC) occurring anywhere in the genitourinary tract. The end point was either recurrence or metastasis of TCC or the closing date of the study, whichever came first. Overall survival was defined as the interval between surgery and death; the end point for this variable was either death or the closing date of the study.
Disease-free and overall-survival curves for the univariate analyses were assessed using the Kaplan-Meier method. Comparisons between survival curves were assessed using Wilcoxon and log-rank tests. Multivariate analysis of the clinicopathologic parameters was performed using the Cox stepwise-regression model. The above analyses were performed using the SAS statistical software package (SAS Institute, Inc., Cary, NC; 24).
Comparisons between p27Kip1 protein immunoreactivity and other tumor characteristics (see Table 1) were performed using the χ2 analysis. Differences were considered significant at P < .05.
RESULTS
The patients' age at diagnosis was within the range of 34 to 84 years, with a median age of 66 years. Thirty-two of the 132 patients died as a result of their tumors 1 to 132 months after surgery (mean, 23 mo; median, 14 mo). The remainder survived 0 to 257 months after surgery (mean, 70 mo; median 64 mo). Among the 132 cases, 55 tumors (41.7%) were in the renal pelvis or calyces, 53 (40.1%) were in the ureter, and 24 (18.2%) were multicentric. Ten patients had simultaneous bladder tumors at the time of diagnosis, 30 had subsequent bladder tumors, and 7 had an antecedent bladder tumor. In all, 47 (35.6%) patients had an associated bladder neoplasm; of these, 4 had such a neoplasm at more than one of the above times and thus appear in more than one group. The initial management of the 125 patients who were not treated as having bladder cancer included complete nephroureterectomy with a bladder cuff (92 patients), nephroureterectomy without a bladder cuff (8 patients), nephroureterectomy with total cystectomy (10 patients), nephrectomy (13 patients), and urectomy (2 patients). Thirty-four patients received adjacent chemotherapy (23 patients), radiotherapy (7 patients), or both (4 patients), in addition to surgery.
The tumors were divided into six stages according to the criteria proposed by the International Union Against Cancer. There was 1 case (0.8%) in Stage pTis (nonpapillary, noninvasive tumors), 51 cases (38.6%) in Stage pTa (papillary, noninvasive tumors), 13 cases (9.8%) in Stage pT1 (tumors invading the submucosa), 8 cases (6.1%) in Stage pT2 (tumors invading the muscularis), 38 cases (28.8%) in Stage pT3 (tumors invading beyond the muscularis or renal parenchyma), and 21 cases (15.9%) in Stage pT4 (tumors metastasizing the regional lymph node or a distant site).
Among all the patients, the one patient with a nonpapillary, noninvasive tumor (pTis) showed neither recurrence nor metastasis within the follow-up period (75 mo). Twelve of the 51 patients with a papillary, noninvasive tumor (pTa) showed recurrence (8 patients), metastasis (1 patient), or both (3 patients), but 39 developed neither recurrence nor metastasis within the follow-up period. In the 12 patients with recurrence and/or metastasis, the mean follow-up was 64 months (median, 48; range, 14 to 123), whereas the mean follow-up for patients without recurrence and metastasis was 83 months (median, 87; range, 4 to 203). Of the 80 patients with an invasive tumor (pT1, pT2, pT3, or pT4), 6 either had metastasis at surgery or had tumors that could not totally be excised by surgery, and 37 showed recurrence (8 patients), metastasis (17 patients), or both (12 patients); but the remaining 37 developed neither recurrence nor metastasis within the follow-up period. The mean follow-up for the 37 patients with recurrence and/or metastasis was 35 months (median, 15; range, 1 to 175), whereas the mean follow-up for the 37 patients without recurrence or metastasis was 59 months (median, 35; range, 0 to 257).
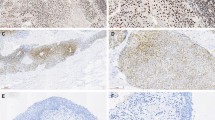
A positive expression of p27Kip1 protein was recognized in 94.7% of the patients studied (seven cases showed no staining by immunohistochemistry). The expression of p27Kip1 protein was confined to the nuclei of tumor cells and was seen frequently in all cell layers (Fig. 1A). In the normal urothelium, expression of p27Kip1 protein was found in all cell layers (Fig. 1B). A positive expression of p53 oncoprotein was recognized in 27.2% of the patients. The immunoreactivity for p53 oncoprotein was confined to the nuclei of tumor cells; no cytoplasmic staining was observed. The positive expression of PCNA was recognized in all tumors. The immunoreactivity for PCNA was confined to the nuclei of tumor cells. The PCNA index was 7.4 to 93.1% (mean and median values for PCNA index, 66.4 and 69%, respectively).
In the assessment of the relationship between the expression of p27Kip1 protein and clinicopathologic findings, the one case of nonpapillary, noninvasive TCC (carcinoma in situ) was excluded because of the difference in clinical course between carcinoma in situ and the other types. Our examination of the relationships between the expression of p27Kip1 protein and clinicopathologic findings, PCNA index, and the expression of p53 oncoprotein showed that the expression of p27Kip1 protein decreased with stage and grade in all tumors (Table 1). When the expression of p27Kip1 protein was assessed separately for noninvasive and invasive tumors, no significant correlations were found.
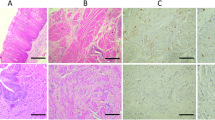
In the assessment of disease-free and overall survivals, 41 cases (8 cases with simultaneous bladder tumors at the time of diagnosis, 31 cases with adjacent treatment other than surgery, and 2 cases with both) were excluded because of the difference in clinical course. Furthermore, in the assessment of disease-free survival, the 87 patients who had no metastasis at surgery and in whom the malignant tumor was excised totally by surgery were included in the analysis. In the assessment of overall survival, 90 patients were included in the analysis. Disease-free and overall survival curves are shown in Figure 2. The rates for a 5-year disease-free survival and a 5-year overall survival were 67.5 and 77.5%, respectively. In a univariate analysis of disease-free and overall survival rates, no correlations were found between the expression of p27Kip1 protein and prognosis (Table 2). Stage, grade, pattern of growth, and immunoreactivity for p53 oncoprotein all had a significant effect on each of the two survivals in all tumors. PCNA index had a significant effect on overall survival. When the expression of p27Kip1 protein was assessed separately for noninvasive and invasive tumors, it was again found to have no effect.
Disease-free and overall survival curves for patients with transitional cell carcinoma (subdivided according to p27Kip1 protein status). (A) Disease-free survival curve: patients with low (n = 52) or high (n = 35) expression of p27Kip1 protein. (B) Overall survival curve: patients with low (n = 55) or high (n = 35) expression of p27Kip1 protein.
Next, only those variables that appeared significant in the univariate analyses of disease-free survival (87 cases) and overall survival (90 cases) were entered into the final models of the multivariate analysis. Only stage was found to be a prognostic factor for survival (for disease-free survival, risk ratio = 2.86, P = .0011; for overall survival, risk ratio = 3.13, P = .0004).
DISCUSSION
The purpose of our investigation was to look for a possible relation between the expression of p27Kip1 protein and clinicopathologic findings or clinical outcome in TCC-UUT. Our analysis of clinicopathologic findings revealed positive relationships between the expression of p27Kip1 protein and both stage and grade. However, no correlation between the expression of p27Kip1 protein and either disease-free or overall survival rate was found in the univariate analysis. Thus, the detection of p27Kip1 protein would appear to be of little or no value in informing the prognosis in TCC-UUT, although it may be a progressive marker for TCC-UUT.
A low expression of p27Kip1 protein has been found to be associated with tumor aggressiveness and an unfavorable prognosis in a variety of tumors, including carcinomas of the breast, stomach, colon, lung, prostate, and ovary (5, 6, 7, 8, 9, 10, 11, 12, 13, 14). With regard to the expression of p27Kip1 protein in TCC of the urinary tract, to our knowledge, only two reports have been published (15, 16). Del Pizzo et al. (15), using immunohistochemistry to examine 50 cases of TCC of the urinary bladder, reported that the expression of p27Kip1 protein was significantly lower in the poorly differentiated tumors and was an independent predictor. However, Kuczyk et al. (16), who used immunohistochemistry to examine 50 cases of muscle-invasive bladder carcinoma, failed to find a relationship between a low expression of p27Kip1 protein and either disease-free or overall survival, although the expression of p27Kip1 protein was related to stage and grade. Although it is true that there are some differences between these two studies in terms of materials (tumors of all stages vs. muscular-invasive tumors), antibodies (polyclonal antibody vs. monoclonal antibody), and the way the immunostaining was quantified (positive cell counts vs. taking “positive expression” as >1% of tumor cells stained), we cannot be sure whether this accounts for the discrepancy between the conclusions reached. In the present study of TCC-UUT, a low expression of p27Kip1 protein was also associated with high stage and high grade. However, no correlation was found between the expression of p27Kip1 protein and clinical outcome in our univariate analysis of disease-free and overall survival rates. On this basis, the detection of p27Kip1 protein would appear to be of little or no value in predicting tumor progression in TCC-UUT.
p27Kip1 protein blocks progression from the G1 to the S phase of the cell cycle and is highly expressed in cells arrested at the G0 or G1 phase (2, 3, 4). Recent reports have indicated that expression of p27Kip1 protein is inversely related to proliferative activity (as measured using Ki-67 antibody) in cells at all stages except the G0 phase in non–small-cell lung carcinomas, endocrine tumors, and malignant lymphomas (25, 26, 27). In the present study, no correlation was found between the expression of p27Kip1 protein and the proliferative activity measured using PCNA antibody, which reacts with nuclei in the late G1 and S phases of the cell cycle. Likewise, in carcinomas of the breast, colorectum, and oral cavity, no correlation has been found between the expression of p27Kip1 protein and proliferative activity (measured using Ki-67 antibody; 7, 28, 29). These results may suggest that the mechanisms by which cellular proliferation is regulated are similar among the various tumor types examined in the above study and the present one.
The CDK inhibitor p21Cip1 is a critical downstream effector in the p53-specific pathway for growth control in mammalian cells (30, 31). In TCCs of the urinary bladder, several investigators have reported finding an expression of p21Cip1 with a higher frequency in tumors with the p53 wild-type gene than in tumors with p53 mutations (32, 33). Furthermore, Lipponen et al. (34) showed by immunohistochemical analysis that the expression of p21Cip1 protein was related to p53 oncoprotein expression. Because p27Kip1 belongs to the same family of CDK inhibitors as p21Cip1, the potential might be thought to exist for a similar relationship between p27Kip1 and p53. In breast carcinomas, an inverse relationship between expression of p27Kip1 protein and expression of p53 oncoprotein was found (35). In ovarian tumors, however, a low expression of p27Kip1 protein was not associated with p53 oncoprotein expression in a study using immunohistochemistry (14). We also failed to demonstrate a correlation between the expression of p27Kip1 protein and an overexpression of p53 oncoprotein in TCC-UUT.
In conclusion, the finding of a low expression of p27Kip1 protein may be of little or no value in informing the prognosis in TCC-UUT, although there does appear to be an association with high stage and high grade. p27Kip1 protein is mainly degraded by the ubiquitin–proteasome pathway. Recently, several investigators indicated that cyclins D and E can regulate p27Kip1 protein levels in some cells (2, 3, 36). Furthermore, multiple CDK inhibitors are necessary to maintain cell cycle progression in this system (37). Therefore, further studies are needed to elucidate the interaction of p27Kip1 protein with other cell cycle regulatory proteins and the relationship between these proteins and clinicopathologic findings or clinical outcome in TCC-UUT.
References
Kamb A . Cell-cycle regulators and cancer. Trends Genet 1995; 11: 136–140.
Sherr CJ . Cancer cell cycles. Science 1996; 274: 1672–1677.
Lloyd RV, Erickson LA, Jin L, Kulig E, Qian X, Cheville JC, et al. p27kip1: a multifunctional cyclin-dependent kinase inhibitor with prognostic significance in human cancers. Am J Pathol 1999; 154: 313–323.
Kato J, Matsuoka M, Polyak K, Massagué J, Sherr CJ . Cyclic AMP-induced G1 phase arrest mediated by an inhibitor (p27Kip1) of cyclin-dependent kinase 4 activation. Cell 1994; 79: 487–496.
Catzavelos C, Bhattacharya N, Ung YC, Wilson JA, Roncari L, Sandhu C, et al. Decreased levels of the cell-cycle inhibitor p27Kip1 protein: prognostic implications in primary breast cancer. Nat Med 1997; 3: 227–230.
Porter PL, Malone KE, Heagerty PJ, Alexander GM, Gatti LA, Firpo EJ, et al. Expression of cell-cycle regulators p27Kip1 and cyclin E, alone and in combination, correlate with survival in young breast cancer patients. Nat Med 1997; 3: 222–225.
Tan P, Cady B, Wanner M, Worland P, Cukor B, Magi-Galluzzi C, et al. The cell cycle inhibitor p27 is an independent prognostic marker in small (T1a, b) invasive breast carcinomas. Cancer Res 1997; 57: 1259–1263.
Mori M, Mimori K, Shiraishi T, Tanaka S, Ueo H, Sugimachi K, et al. p27 expression and gastric carcinoma [Letter]. Nat Med 1997; 3: 593.
Loda M, Cukor B, Tam SW, Lavin P, Fiorentino M, Draetta GF, et al. Increased proteasome-dependent degradation of the cyclin-dependent kinase inhibitor p27 in aggressive colorectal carcinomas. Nat Med 1997; 3: 231–234.
Esposito V, Baldi A, DeLuca A, Groger AM, Loda M, Giordano GG, et al. Prognostic role of the cyclin-dependent kinase inhibitor p27 in non-small cell lung cancer. Cancer Res 1997; 57: 3381–3385.
Yatabe Y, Masuda A, Koshikawa T, Nakamura S, Kuroishi T, Osada H, et al. p27KIP1 in human lung cancers: differential changes in small cell and non-small cell carcinomas. Cancer Res 1998; 58: 1042–1047.
Tsihlias J, Kapusta LR, DeBoer G, Morava-Protzner I, Zbieranowski I, Bhattacharya N, et al. Loss of cyclin-dependent kinase inhibitor p27Kip1 is a novel prognostic factor in localized human prostate adenocarcinoma. Cancer Res 1998; 58: 542–548.
Yang RM, Naitoh J, Murphy M, Wang H-J, Phillipson J, DeKernion JB, et al. Low p27 expression predicts poor disease-free survival in patients with prostate cancer. J Urol 1998; 159: 941–945.
Newcomb EW, Sosnow M, Demopoulos RI, Zeleniuch-Jacquotte A, Sorich J, Speyer JL . Expression of the cell cycle inhibitor p27kip1 is a new prognostic marker associated with survival in epithelial ovarian tumors. Am J Pathol 1999; 154: 119–125.
Del Pizzo JJ, Borkowski A, Jacobs SC, Kyprianou N . Loss of cell cycle regulators p27kip1 and cyclin E in transitional cell carcinoma of the bladder correlates with tumor grade and patient survival. Am J Pathol 1999; 155: 1129–1136.
Kuczyk MA, Machtens S, Bokemeyer C, Hradil K, Macheel I, Jetscho V, et al. Prognostic value of p27Kip1 and p21WAF/Cip protein expression in muscle invasive bladder cancer. Oncol Rep 1999; 6: 687–693.
Sidransky D, Von Eschenbech A, Tsai YC, Jones P, Summerhayes I, Marshall F, et al. Identification of p53 gene mutations in bladder cancers and urine samples. Science 1991; 252: 706–709.
Fujimoto K, Yamada Y, Okajima E, Kakizoe T, Sasaki H, Sugimura T, et al. Frequent association of p53 gene mutation in invasive bladder cancer. Cancer Res 1992; 52: 1393–1398.
Esrig D, Spruck CH III, Nichols PW, Chaiwun B, Steven K, Groshen S, et al. p53 nuclear protein accumulation correlates with mutations in the p53 gene, tumor grade, and stage in bladder cancer. Am J Pathol 1993; 143: 1389–1397.
Nakanishi K, Kawai T, Torikata C . Immunohistochemical evaluation of p53 oncoprotein in transitional cell carcinoma of the upper urinary tract. Hum Pathol 1996; 27: 1336–1340.
Nakanishi K, Tominaga S, Kawai T, Torikata C, Aurues T, Ikeda T . Expression of bcl-2 oncoprotein in transitional cell carcinoma of the upper urinary tract. Virchows Archiv 1998; 432: 445–450.
UICC (International Union Against Cancer). Renal pelvis and ureter. In: Sobin LH, Wittenkind C, editors. TNM classification of malignant tumours. 5th ed. New York: Wiley, 1997: 183–186.
Murphy WM, Beckwith JB, Farrow GM . Tumors of the kidney, bladder, and related urinary structures. Atlas of tumor pathology. 3rd series, fascicle 11. Washington, DC: Armed Forces Institute of Pathology, 1994: 202–219.
SAS Institute Inc. The PHREG procedure, version 6. (SAS technical report P-217, SAS/STAT software.) Cary, NC: SAS Institute Inc.; 1991. p. 63.
Kawana H, Tamaru J, Tanaka T, Hirai A, Saito Y, Kitagawa M, et al. Role of p27kip1 and cyclin-dependent kinase 2 in the proliferation of non-small cell lung cancer. Am J Pathol 1998; 153: 505–513.
Lloyd RV, Jin L, Qian X, Kulig E . Aberrant p27kip1 expression in endocrine and other tumors. Am J Pathol 1997; 150: 401–407.
Sánchez-Beato M, Sáez AI, Martínez-Montero JC, Mateo MS, Sánchez-Verde L, Villuendas R, Troncone G, et al. Cyclin-dependent kinase inhibitor p27KIP1 in lymphoid tissue: p27KIP1 expression is inversely proportional to the proliferative index. Am J Pathol 1997; 151: 151–160.
Ciaparrone M, Yamamoto H, Yao Y, Sgambato A, Cattoretti G, Tomita N, et al. Localization and expression of p27KIP1 in multistage colorectal carcinogenesis. Cancer Res 1998; 58: 114–122.
Jordan RCK, Bradley G, Slingerland J . Reduced levels of the cell-cycle inhibitor p27Kip1 in epithelial dysplasia and carcinoma of the oral cavity. Am J Pathol 1998; 152: 585–590.
El-Deiry WS, Tokino T, Velculescu VE, Levy DB, Parsons R, Trent JM, et al. WAF1, a potential mediator of p53 tumor suppression. Cell 1993; 75: 817–825.
Harper JW, Adami GR, Wei N, Keyomarsi K, Elledge SJ . The p21 Cdk-interacting protein Cip1 is a potent inhibitor of G1 cyclin-dependent kinases. Cell 1993; 75: 805–816.
Malkowicz SB, Tomaszewski JE, Linnenbach AJ, Cangiano TA, Maruta Y, McGarvey TW . Novel p21WAF/CIP1 mutations in superficial and invasive transitional cell carcinomas. Oncogene 1996; 13: 1831–1837.
Pfister C, Larue H, Moore L, Lacombe L, Veilleux C, Tetu B, et al. Tumorigenic pathways in low-stage bladder cancer based on p53, MDM2 and p21 phenotypes. Int J Cancer 2000; 89: 100–104.
Lipponen P, Aaltomaa S, Eskelinen M, Ala-Opas M, Kosma V-M . Expression of p21(waf/cip1) protein in transitional cell bladder tumours and its prognostic value. Eur Urol 1998; 34: 237–243.
Wu J, Shen Z-Z, Lu J-S, Jiang M, Han Q-X, Fontana JA, et al. Prognostic role of p27Kip1 and apoptosis in human breast cancer. Br J Cancer 1999; 79: 1572–1578.
Cheng M, Sexl V, Sherr CJ, Roussel MF . Assembly of cyclin D-dependent kinase and titration of p27Kip1 regulated by mitogen-activated protein kinase kinase (MEK1). Proc Natl Acad Sci U S A 1998; 95: 1091–1096.
Pedram A, Razandi M, Hu R-M, Levin ER . Astrocyte progression from G1 to S phase of the cell cycle depends upon multiple protein interaction. J Biol Chem 1998; 273: 13966–13972.
Acknowledgements
The authors are indebted to Dr. R. Timms for correcting the English.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nakanishi, K., Kawai, T., Aida, S. et al. Expression of p27Kip1 Protein in Transitional Cell Carcinoma of the Upper Urinary Tract. Mod Pathol 14, 371–376 (2001). https://doi.org/10.1038/modpathol.3880320
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3880320
Keywords
This article is cited by
-
Significance of p53, p27, Ki-67, E-cadherin, and HER2 expression in upper urinary tract urothelial carcinoma
Journal of the Egyptian National Cancer Institute (2020)
-
Expression of p53 in upper urinary tract urothelial carcinoma
Nature Reviews Urology (2011)
-
pT classification, grade, and vascular invasion as prognostic indicators in urothelial carcinoma of the upper urinary tract
Modern Pathology (2006)