Abstract
Loss of heterozygosity (LOH) has previously been demonstrated at multiple chromosome microsatellites in primary and metastatic melanomas. Epidermotropic metastases of melanoma are unique in their varied histopathologic appearance, which can mimic a primary lesion. Our objective was to compare LOH profiles in primary and epidermotropic metastatic melanoma to delineate their clonal relationship. We examined the pattern of allelic loss in the primary melanomas of nine patients in addition to the 21 corresponding epidermotropic metastatic melanomas (average 2.3 metastases per patient). DNA samples were prepared from formalin-fixed, paraffin-embedded tissue sections using laser capture microdissection. Eight DNA microsatellite markers on six different chromosomes were analyzed: D1S214 (1p), D6S305 (6q), D9S171 (9p), D9S157 (9p), IFNA (9p), D10S212 (10q), D11S258 (11q), D18S70 (18q). In addition, X-chromosome inactivation analysis was performed in tumors from four women. LOH was seen in 67% (6/9) of primary melanomas and 81% (17/21) of epidermotropic metastatic melanomas. The most frequent allelic losses in informative cases occurred at 10q (33%), 9p (22%), and 11q (22%) in primary melanomas, and at 10q (50%), 1p (44%), and 6q (39%) in epidermotropic metastatic melanomas. Primary lesions demonstrating LOH had concordant allelic loss in at least one locus in a corresponding epidermotropic metastatic melanoma in 83% (5/6) of cases. X-chromosome analysis showed nonrandom inactivation in 75% (3/4) and 71% (5/7) of primary melanoma and epidermotropic metastatic melanoma cases, respectively. Our LOH and X-chromosome inactivation analysis data suggest that epidermotropically metastatic melanomas are clonally related to their primary lesion in many cases. Our data also indicated that some cases diagnosed as epidermotropic metastatic melanoma might be divergent clones or new primaries rather than metastatic disease.
Similar content being viewed by others
Introduction
Epidermotropic metastatic melanoma is an uncommon form of melanoma metastasis that can pose significant difficulty histopathologically in its distinction from a new primary melanoma. The clinical implications in this distinction are of paramount importance in staging and prognosis: a patient with multiple primary melanomas is staged based on the primary lesion with the worst prognostic features, whereas a patient with a distant cutaneous metastasis has stage IV disease with an approximate 10% 5-year survival rate.1, 2, 3
The histopathologic characteristics for differentiating epidermotropic metastatic melanoma from a primary melanoma were first proposed by Kornberg4 in 1978. According to that report, the following three features favored a diagnosis of epidermotropic metastatic melanoma: (1) thinning of the epidermis by the underlying aggregates of atypical melanocytes in the dermis, often in association with widened dermal papillae and an epidermal collarette at the periphery of the tumor; (2) atypical melanocytes present within endothelial lined spaces, and (3) a zone of atypical melanocytes in the dermis equal to or broader than the epidermal component. However, since the original description, multiple reports have described the varied histopathologic presentations of epidermotropic metastatic melanomas, proposed additional criteria, and questioned whether histopathology alone can differentiate these metastases from a new primary melanoma.5, 6, 7, 8, 9, 10, 11, 12
Molecular studies of melanoma and its metastases in various forms have revealed frequent genetic alterations. Traditional ideology infers that tumors result when a single transformed cell leads to a clonal population of malignant cells. Further divergence of the clone may result in subpopulations of neoplastic cells, some of which gain the capacity to metastasize.13, 14, 15, 16, 17 Although genetic heterogeneity is the norm in melanoma,18, 19, 20, 21, 22 it would be expected that a primary melanoma and its metastases would share at least one or more genetic alterations. Studies to date have shown that loss of heterozygosity (LOH) on 9p and 10q has been associated with early-stage primary disease, whereas LOH on 6q, 1p, 8q, and 11q has been associated with progression and metastasis.19 In this report, we studied primary melanomas and their corresponding epidermotropic metastases using LOH analysis and X-chromosome inactivation analysis to delineate their clonal relationship.
Materials and methods
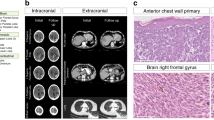
Cases were obtained using a diagnostic search for epidermotropic metastatic melanomas from the dermatopathology and surgical pathology case files at Indiana University and the University of Louisville dermatopathology files from January 1998 to September 2004. Only those patients with both the primary melanoma and corresponding epidermotropic metastatic melanomas available for review were included in the study. Archived formalin-fixed, paraffin-embedded tissue was obtained for nine patients (five men, four women; mean age 51 years), including their primary lesion and 21 epidermotropic metastatic melanoma's (average 2.3 epidermotropic metastatic melanoma's per patient) totaling 30 tumors. Table 1 lists the clinical characteristics for each case. Corresponding glass slides were reviewed for histologic confirmation (Figure 1) and to ensure adequate tumor was present for laser capture microdissection.
Histologic sections were prepared from the retrieved archival tissue, one of which was stained with hematoxylin and eosin for use as an identification slide for tumor cells. Laser-assisted microdissection of primary and metastatic melanoma was performed (Figure 2) on unstained sections using a PixCell II Laser Capture Microdissection (LCM) system (Arcturus Engineering, Mountain View, CA, USA) as described previously.23, 24, 25, 26 Approximately 400–1000 cells of primary and metastatic melanoma were microdissected from the 5-μm histologic sections. Normal tissue from each case was microdissected as a control.
The dissected cells were deparaffinized with xylene and ethyl alcohol. Amplification of genomic DNA via polymerase chain reaction (PCR) was performed at various specific loci on six different chromosomes, using the following primers (Research Genetics Inc., Huntsville, AL, USA): D1S214 (1p), D6S305 (6q), D9S157 (9p), D9S171 (9p), IFNA (9p), D10S212 (10q), D11S528 (11q), D18S70 (18q). PCR amplification and gel electrophoresis were performed as described previously.27, 28, 29, 30, 31 The criterion for allelic loss was complete or nearly complete (≥75%) absence of one allele in tumor DNA.27, 28, 29, 32, 33, 34 PCRs for each polymorphic microsatellite marker were repeated at least twice from the same DNA preparations, and the same results were obtained. Results were reported as noninformative when visual inspection could not distinguish two distinct band forms in control DNA following PCR amplification.
X-chromosome inactivation was performed on the melanomas from the four female patients. DNA samples were prepared from both primary and metastatic melanoma tumor components. Dissected cells were placed in 50 μl of buffer (10 mM Tris-HCl, 1 mM EDTA, 1% Tween 20, and 0.4 mg/ml of proteinase K at pH 8.3) and incubated overnight at 37°C. Proteinase K inactivation was achieved by boiling the solution for 10 min; subsequently the solution was used directly for clonal analysis without further purification. Aliquots (8 μl) of the DNA extract were digested overnight at 37°C with 1 U of HhaI restriction endonuclease (New England Biolabs Inc., Beverly, MA, USA) in a total volume of 10 μl. Control reactions incubating equivalent aliquots of the DNA extract in digestion buffer lacking HhaI endonuclease were performed for each sample. Following incubation, 3 μl of digested or nondigested DNA was amplified in a 25-μl PCR volume, containing 0.1 μl 32[P]α-labeled deoxyadenosine triphosphate (dATP) (3000 Ci/mmol), 4 μM AR-sense primer (5′-TCC AGA ATC TGT TCC AGA GCG TGC-3′), 4 μM AR-antisense primer (5′-GCT GTG AAG GTT GCT GTT CCT CAT-3′), 4% dimethyl sulfoxide, 2.5 mM MgCl2, 300 μM deoxycytidine triphosphate, 300 μM deoxythymidine triphosphate, 300 μM deoxyguanosine triphosphate, 300 μM dATP, and 0.65 U Taq polymerase (Perkin-Elmer Corp., Norwalk, CT, USA).
Each PCR amplification consisted of the following steps: denaturation at 95°C for 8 min, followed by 37 cycles at 95°C for 40 s, at 63°C for 40 s and at 72°C for 60 s, and then a single final extension step at 72°C for 10 min. PCR products were then diluted with 4 μl of loading buffer, containing 95% formamide, 20 mM EDTA, 0.05% bromphenol blue, and 0.05% xylene cyanol FF (Sigma Chemical Co., St Louis, MO, USA). Samples were heated to 95°C for 5 min, followed by placement on ice. A portion of the reaction mixture (3 μl) was loaded onto 6.5% polyacrylamide-denaturing gels without formamide, and the PCR products were separated by electrophoresis at 80 W for 2 h. The bands were observed after autoradiography with Kodak X-OMAT film (Eastman Kodak Company, Rochester, NY, USA) for 8–16 h.
Cases were considered informative if two AR allelic bands were detected after PCR amplification in normal control samples that had not been treated with HhaI, and only these were included in the analysis. Nonrandom X-chromosome inactivation was defined as a complete or nearly complete (≥75%) absence of an AR allele after HhaI digestion, which indicated a predominance of one allele.30, 31, 35, 36 Tumors were considered to be of the same clonal origin if the same AR allelic inactivation pattern was detected in both the primary melanoma and its corresponding epidermotropic metastatic melanomas. Conversely, tumors were considered to be of independent origin if alternate predominance of AR alleles after HhaI digestion (different allelic inactivation patterns) was detected in the primary and metastatic melanoma components.
Results
The overall frequency of allelic loss was 67% (6/9) in the primary melanomas and 81% (17/21) in the epidermotropic metastatic melanomas (Figure 3). The most frequent allelic losses in informative cases occurred at 10q (33%), 9p (22%), and 11q (22%) in primary melanomas, and at 10q (50%), 1p (44%), and 6q (39%) in epidermotropic metastatic melanomas (Figure 4). The frequency of allelic loss in all of the informative primary tumors was as follows: 2/9 (22%) at D9S171, 1/8 (13%) at D6S305, 2/9 (22%) at D11S528, 1/7 (14%) at D1S214, 2/6 (33%) at D10S212, 1/9 (11%) at D9S157, 0/8 (0%) at IFNA, and 1/8 (13%) at D18S70. The frequency of allelic loss in all of the informative epidermotropic metastatic melanomas was as follows: 8/21 (38%) at D9S171, 7/18 (39%) at D6S305, 2/21 (9%) at D11S528, 7/16 (44%) at D1S214, 6/12 (50%) at D10S212, 8/21 (38%) at D9S157, 2/19 (11%) at IFNA, and 5/17 (29%) at D18S70.
Representative electrophoretic gels from LOH analysis of cases 3 and 4 (a, b), and X-chromosome inactivation analysis of case 8 (c). N=normal; P=primary; EMM=epidermotropic metastatic melanoma, −=without hHaI digestion,+= with hHaI digestion. Case 3 demonstrates identical patterns of allelic loss on chromosome 1p for the primary lesion and its corresponding epidermotropic metastatic melanoma (a). Case 4 at chromosome 9p shows epidermotropic metastatic melanomas that appear related to each other, but clonally not related to the primary melanoma (b). Case 8 demonstrates clonal relationship with inactivation of the X-chromosome in both the primary and metastatic lesion (c).
Of those primary lesions demonstrating LOH, 83% (5/6) had concordant allelic loss in at least one locus of a corresponding epidermotropic metastatic melanoma lesion and 33% (2/6) had concordant allelic loss in two loci (Table 2). Nonrandom inactivation of X-chromosome was seen in 75% (3/4) of primary lesions and 71% (5/7) of epidermotropic metastatic melanomas. Based on LOH and X-chromosome inactivation patterns, as represented in Table 2, interpretations were made as follows: four cases demonstrated clonally related primary and metastatic lesions (cases 1, 3, 7, and 8); one case was likely clonally related as some shared patterns were observed (case 2); one case shared clonal relation to one of its epidermotropic metastases, but demonstrated independent origin from a second epidermotropic metastatic lesion (case 6); one case demonstrated clonal relationship among the four epidermotropic metastatic melanomas, but not between the primary melanoma and the metastatic lesions (case 4); one case showed an epidermotropic metastatic melanoma that was independent from the primary lesion (case 9); and one case had inconclusive results because of rare LOH and non-informative loci (case 5).
Discussion
Many studies have investigated the genetic relationships between melanoma and its various forms of metastatic lesions.19, 20, 21, 37, 38, 39 However, the present study is the first to assess clonal genetic relationships between primary melanomas and an uncommon subtype of metastasis, the epidermotropic metastatic melanoma. The importance of studying this relationship is underscored by the fact that histopathology alone may be insufficient to distinguish an epidermotropic metastatic melanoma from a new primary lesion. Kornberg's original histopathologic criteria for epidermotropic metastatic melanoma have been challenged since his original report in 1978.4 Descriptions of epidermotropic metastatic melanomas that are present, more similar to a primary melanoma, with epidermal components of atypical melanocytes that are broader than those seen in the dermis, in addition to epidermotropic metastatic melanomas, simulating melanoma in situ, have been reported.6, 11 Additionally, evolving criteria for epidermotropic metastatic melanomas, such as angiotropism, maturation, and striking pagetoid spread have been described.5, 7 Thus, there is a group of epidermotropic metastatic melanomas that fit the classic description; however, there is also a group that does not, often leading to significant diagnostic challenge in differentiating a metastasis from a new primary lesion. The resulting implications for staging and prognosis rest on accurately delineating this differential diagnosis.
Our findings, based on LOH analysis and X-chromosome inactivation analysis indicate that, in most cases, epidermotropic metastases are or are likely to be related to the primary lesion. However, some of the discordant results indeed confirm that histopathology alone may be insufficient to distinguish between a new primary melanoma vs a metastatic lesion. For example, one of the cases had shared clonality among the four metastatic lesions, but none of these metastases shared clonality with the primary lesion. This raises the possibility that perhaps this patient had two primary melanomas, one of which gave rise to a subpopulation that then metastasized. Another case demonstrated a clonal genetic relationship between the primary lesion and one of the two epidermotropic metastatic lesions. The second epidermotropic metastatic melanoma did not share clonality, and the possibility that this represented a new primary lesion warrants consideration. Furthermore, there was one case where the primary melanoma and single epidermotropic metastatic melanoma demonstrated independent origin. If in reality, the metastasis was a new primary, it is likely that this patient would be downstaged resulting in a different management strategy and an improved prognosis.
We do recognize that one limitation to any molecular study of melanoma is directly related to the intra- and intertumoral heterogeneity that is often demonstrated. A recent study by Katona et al39 challenges the traditional notion that a primary melanoma is derived from a single transformed cell. Furthermore, the study found independent origin for separate melanoma metastases that presumably arose from the same primary tumor. Overall the majority of metastases in the study shared common clonal origin with the primary tumor.
Studies have validated that certain loci frequently show LOH at different stages of tumor progression. Many reports have shown that primary melanomas most frequently demonstrate LOH on chromosome 9 in the region of a well-known tumor suppressor gene, p16INK4.19, 21, 38, 40, 41 Interestingly, this region was the second most frequent site of LOH in our primary melanomas, with LOH at 10q found most frequently. LOH at 10q was also found most frequently and in higher proportion in the epidermotropic metastatic melanomas. The marker used in this study represents the site at 10q26, which is very near to tumor suppressor genes, PTEN/MMAC and MXI1, which have both been described as showing allelic losses in melanomas.21, 38, 42 As epidermotropic metastases represent a somewhat unique form of melanoma metastasis, the question arises of whether perhaps the 10q loci may be of greater importance in this relationship of melanoma with epidermotropic metastases. Further study with larger sample size would be required to investigate this possibility. In the current study, LOH at 1p and 6q was also a frequent finding in the epidermotropic metastatic melanomas confirming past investigations that have found frequent LOH at these sites in various subtypes of melanoma metastases.19, 38
In conclusion, we found that primary melanomas and their epidermotropic metastatic melanomas have LOH at various microsatellite regions on chromosomes 1p, 6q, 9p, 10q, 11q, and 18q. Additionally, nonrandom X-chromosome inactivation is seen in the majority of cases in women. In many of the cases, concordant LOH was seen in primary melanomas and their corresponding epidermotropic metastatic melanomas, suggesting clonally related lesions. However, variable patterns within the same case indicate that, whereas some epidermotropic metastatic melanomas are clonally related to the primary, others are of independent origin. Furthermore, independent origin was shown in one case, indicating that some cases likely represent divergent clones or de novo primary lesions rather than true metastases. Additional testing is warranted to determine if LOH and clonality assays are useful in delineating epidermotropic metastatic melanomas from new primary melanomas.
References
Balch CM, Soong SJ, Atkins MB, et al. An evidence based staging system for cutaneous melanoma. CA Cancer J Clin 2004;54:131–149.
Balch CM, Buzaid AC, Soong SJ, et al. New TNM melanoma staging system: linking biology and natural history to clinical outcomes. Semin Surg Oncol 2003;21:43–52.
Balch CM, Buzaid AC, Soong SJ, et al. Final version of the American Joint Committee on Cancer staging system for cutaneous melanoma. J Clin Oncol 2001;19:3635–3648.
Kornberg R, Harris M, Ackerman AB . Epidermotropically metastatic malignant melanoma: differentiating malignant melanoma metastatic to the epidermis from malignant melanoma primary in the epidermis. Arch Dermatol 1978;114:67–69.
White WL, Hitchcock MG . Dying dogma: the pathological diagnosis of epidermotropic metastatic malignant melanoma. Semin Diagn Pathol 1998;15:176–188.
Heenan PJ, Clay CD . Epidermotropic metastatic melanoma simulating multiple primary melanomas. Am J Dermatopathol 1991;13:396–402.
Gerami P, Shea C, Stone MS . Angiotropism in epidermotropic metastatic melanoma: another clue to the diagnosis. Am J Dermatopathol 2006;28:429–433.
Warner TF, Gilbert EF, Ramirez G . Epidermotropism in melanoma. J Cutan Pathol 1980;7:50–54.
Jackson R . Epidermotropic malignant melanoma: the distinction between metastatic and new primary lesions in the skin. Can J Surg 1984;27:533–535.
Hayashi H, Kawashima T, Hosokawa K, et al. Epidermotropic metastatic malignant melanoma with a pedunculated appearance. Clin Exp Dermatol 2003;28:666–680.
Abernethy JL, Soyer HP, Kerl H, et al. Epidermotropic metastatic malignant melanoma simulating melanoma in situ: a report of 10 examples from two patients. Am J Surg Pathol 1994;18:1140–1149.
Bengoechea-Beeby MP, Velasco-Oses A, Fernandez FM, et al. Epidermotropic metastatic melanoma: are the current histologic criteria adequate to differentiate primary from metastatic melanoma? Cancer 1993;72:1909–1913.
Fidler IJ, Kripke ML . Metastasis results from preexisting variant cells within a malignant tumor. Science 1977;197:893–895.
Fidler IJ . Critical factors in the biology of human cancer metastasis: twenty-eighth G.H.A. clowes memorial award lecture. Cancer Res 1990;50:6130–6138.
Heppner GH . Tumor heterogeneity. Cancer Res 1984;44:2259–2265.
Konemann S, Schuck A, Malath J, et al. Cell heterogeneity and subpopulations in solid tumors characterized by simultaneous immunophenotyping and DNA content analysis. Cytometry 2000;41:172–177.
Nicolson GL . Generation of phenotypic diversity and progression in metastatic tumor cells. Cancer Metastasis Rev 1984;3:25–42.
Boni R, Matt D, Voetmeyer A, et al. Chromosomal allele loss in primary cutaneous melanoma is heterogeneous and correlates with proliferation. J Invest Dermatol 1998;110:215–217.
Morita R, Fujimoto A, Hatta N, et al. Comparison of genetic profiles between primary melanomas and their metastases reveals genetic alterations and clonal evolution during progression. J invest Dermatol 1998;111:919–924.
Bogdan I, Xin H, Burg G, et al. Heterogeneity of allelic deletions within melanoma metastases. Melanoma Res 2001;11:349–354.
Rao UNM, Jones MW, Finkelstein SD . Genotypic analysis of primary and metastatic cutaneous melanoma. Cancer Genet Cytogenet 2003;140:37–44.
Takata M, Morita R, Takehara K . Clonal heterogeneity in sporadic melanomas as revealed by loss-of-heterozygosity analysis. Int J Cancer 2000;85:492–497.
Emmert-Buck MR, Bonner RF, Smith PD, et al. Laser capture microdissection. Science 1996;274:998–1001.
Bonner RF, Emmert-Buck MR, Cole K, et al. Laser capture microdissection: molecular analysis of tissue. Science 1997;278:1481–1483.
Brandli DW, Ulbright TM, Foster RS, et al. Stroma adjacent to metastatic mature teratoma after chemotherapy for testicular germ cell tumor is derived from the same progenitor cells as the teratoma. Cancer Res 2003;63:6063–6068.
Kernek KM, Ulbright TM, Zhang S, et al. Identical allelic loss in mature teratoma and different histologic components of malignant mixed germ cell tumors of the testis. Am J Pathol 2003;163:2477–2484.
Cheng L, Shan A, Cheville JC, et al. Atypical adenomatous hyperplasia of the prostate: a premalignant lesion? Cancer Res 1998;58:389–391.
Cheng L, Song SY, Pretlow TG, et al. Evidence of independent origin of multiple tumors from patients with prostate cancer. J Natl Cancer Inst 1998;90:233–237.
Cheng L, Bostwick DG, Li G, et al. Allelic imbalance in the clonal evolution of prostate carcinoma. Cancer 1999;85:2017–2022.
Cheng L, Gu J, Eble JN, et al. Molecular genetic evidence for different clonal origin of components of human renal angiomyolipomas. Am J Surg Pathol 2001;25:1231–1236.
Gu J, Roth LM, Younger C, et al. Molecular evidence for the independent origin of extra-ovarian papillary serous tumors of low malignant potential. J Natl Cancer Inst 2001;93:1147–1152.
Emerson RE, Ulbright TM, Zhang S, et al. Nephroblastoma arising in a germ cell tumor of testicular origin. Am J Surg Pathol 2004;28:687–692.
McCarthy RP, Zhang S, Bostwick DG, et al. Molecular genetic evidence for different clonal origins of epithelial and stromal components of phyllodes tumor of the prostate. Am J Pathol 2004;4: 1395–1400.
Cheng L, MacLennan GT, Zhang S, et al. Laser capture microdissection analysis reveals frequent allelic losses in papillary urothelial neoplasm of low malignant potential of the urinary bladder. Cancer 2004;101:183–188.
Cheng L, Gu J, Ulbright TM, et al. Precise microdissection of human bladder carcinomas reveals divergent tumor subclones in the same tumor. Cancer 2002;94:104–110.
Paterson RF, Ulbright TM, MacLennan T, et al. Molecular genetic alterations in the laser-capture microdissected stroma adjacent to bladder carcinoma. Cancer 2003;98:1830–1836.
Slominski A, Wortsman J, Nickoloff B, et al. Molecular pathology of malignant melanoma. Am J Clin Pathol 1998;110:788–794.
Nakayama T, Taback B, Turner R, et al. Molecular clonality of in-transit melanoma metastasis. Am J Pathol 2001;158:1371–1378.
Katona TM, Jones TD, Wang M, et al. Genetically heterogeneous and clonally unrelated metastases may arise in patients with cutaneous melanoma. Am J Surg Pathol 2007 (in press).
Peris K, Keller G, Chimenti S, et al. Microsatellite instability and loss of heterozygosity in melanoma. J Invest Dermatol 1995;105:625–628.
Funk JO, Schiller PI, Barrett MT, et al. p16INK4a expression is frequently decreased and associated with 9p21 loss of heterozygosity in sporadic melanoma. J Cutan Pathol 1998;25:291–296.
Ariyanayagam-Baksh SM, Baksh FK, Swalsky PA, et al. Loss of heterozygosity in the MXI1 gene is a frequent occurrence in melanoma. Mod Pathol 2003;16:992–995.
Author information
Authors and Affiliations
Corresponding author
Additional information
Duality of interest
None declared.
Rights and permissions
About this article
Cite this article
Bahrami, S., Cheng, L., Wang, M. et al. Clonal relationships between epidermotropic metastatic melanomas and their primary lesions: a loss of heterozygosity and X-chromosome inactivation-based analysis. Mod Pathol 20, 821–827 (2007). https://doi.org/10.1038/modpathol.3800833
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3800833
Keywords
This article is cited by
-
Biological resonance for cancer metastasis, a new hypothesis based on comparisons between primary cancers and metastases
Cancer Microenvironment (2013)