Abstract
Accumulation of advanced glycation end products (AGE) of the Maillard reaction increases by aging and in age-enhanced diseases such as atherosclerosis and diabetic complications. Immunohistochemical analysis has been used to demonstrate AGE in vivo. In immunochemistry, the heat-induced epitope retrieval technique is extensively used with formalin-fixed, paraffin-embedded tissue sections. Here we examined whether AGE could be formed artificially through the heating process. Normal rat skin and liver samples were divided into two groups, one rapidly frozen, the other formalin-fixed, paraffin-embedded and submitted to heat-induced epitope retrieval treatment. In heat-treated sections, the cytoplasm of rat epidermal cells and hepatocytes were strongly stained by monoclonal antibody against Nε-(carboxymethyl)lysine (CML), while the staining was negligible in either frozen sections or in paraffin-embedded but heat-untreated sections. To clarify the mechanism, we conducted heat treatment to glycated human serum albumin (HSA), a model Amadori protein, and generation of CML was determined by immunochemical and HPLC analysis. CML was generated from glycated HSA by heat treatment (above 80° C) and increased in a time-dependent manner. In contrast, generation of CML from glycated HSA was significantly inhibited in the presence of NaBH4, a reducing agent, diethylenetriamine pentaacetic acid, a chelator of transition metal ion, or aminoguanidine, a trapping reagent for α-oxoaldehydes. Furthermore, heat-induced CML formation in rat liver samples determined by HPLC was markedly reduced by pretreatment with NaBH4. Reactive intermediates such as glucosone, 3-deoxyglucosone, methylglyoxal, and glyoxal were formed upon heat treatment of glycated HSA at 100° C, indicating that these aldehydes generated from Amadori products by oxidative cleavage can contribute to further CML formation. CML generated by heating, directly from Amadori products or via these aldehydes, might serve as an artifact upon immunohistochemistry.
Similar content being viewed by others
Introduction
Long-term incubation of proteins with glucose leads, through early-stage products such as Schiff base and Amadori products, to the formation of advanced glycation end products (AGE), which are characterized by fluorescence, brown color, and intra- or intermolecular cross-linking (Maillard, 1912). Several AGE structures have been identified including pyrraline (Hayase et al, 1989), pentosidine (Sell and Monnier, 1989), Nε-(carboxymethyl)lysine (CML) (Ahmed et al, 1986), crosslines (Nakamura et al, 1992), imidazolone (Konishi et al, 1994; Lo et al, 1994), methylglyoxal lysine dimer (Frye et al, 1998), Nε-(carboxyethyl)lysine (Ahmed et al, 1997), vesperlysine A, B, and C (Nakamura et al, 1997), glyoxal lysine dimer (Frye et al, 1998), argpyrimidine (Oya et al, 1999), and carboxymethylarginine (Iijima et al, 2000). Among these products, several in vitro experiments demonstrated that CML (Ikeda et al, 1996; Reddy et al, 1995) is a major antigenic AGE structure in vivo. CML is generated through three pathways in vitro: by oxidative cleavage of Amadori products, cleavage of Schiff base through Namiki pathway, and autoxidation of glucose through glyoxal. Among these, oxidative cleavage of Amadori products into CML is considered a major pathway in vivo because this pathway mostly progresses under physiological phosphate concentrations (Wells-Knecht et al, 1995b). Furthermore, we have demonstrated that hydroxyl radical plays a major role in the formation of CML from Amadori products (Nagai et al, 1997).
Recent immunological studies have demonstrated the presence of AGE proteins in several human and animal tissues. AGE modification is potentially involved in the normal aging process (Araki et al, 1992; Kimura et al, 1995, 1996), as well as in the pathogenesis of several age-enhanced diseases such as diabetic nephropathy (Imai et al, 1997; Makino et al, 1995; Suzuki et al, 1995), atherosclerosis (Kume et al, 1995; Sakata et al, 1998), diabetic retinopathy (Hammes et al, 1996), hemodialysis-associated amyloidosis (Miyata et al, 1993, 1996; Morita et al, 1996), chronic renal failure (Yamada et al, 1994b), and Alzheimer disease (Smith et al, 1994a, 1994b; Vitek et al, 1994; Yan et al, 1994). Furthermore, AGE accumulated in hippocampal neurons (Kimura et al, 1996), neurofibrillary tangles (Kimura et al, 1996), peripheral nerves (Sugimoto et al, 1997), atherosclerotic lesions in rat aortas (Meng et al, 1996, 1998), atherosclerotic coronary arteries (Nakamura et al, 1993), murine amyloid (Hoshii et al, 1996), peritoneum in patients on continuous ambulatory peritoneal dialysis (Nakayama et al, 1997), human skin elastin in actinic elastosis (Mizutari et al, 1997), adrenal lipofuscin (Shimokawa et al, 1998), cardiac tissues of renal transplant patients (Yoshida et al, 1998), pulmonary fibrosis (Matsuse et al, 1998), hemoglobin (Ando et al, 1999; Makita et al, 1992b), and human plasma (Bucala et al, 1993; Makita et al, 1992a). Therefore, accurate measurement of AGE accumulation is fundamental to further studies on the aging process and the pathogenesis of age-dependent diseases as well as to future clinical applications.
To determine the CML content in vivo, tissue samples are solubilized in alkaline condition to enhance solubility (Mitsuhashi et al, 1993; Nakayama et al, 1993). However, conversion of Amadori products to CML is enhanced under alkaline conditions (Nagai et al, 1998). Furthermore, 2-(2-furoyl)-4(5)-(2-furanyl)-1H-imidazole was once characterized as a major AGE structure (Chang et al, 1985; Pongor et al, 1984), but later studies confirmed it to be an artifact substance generated by ammonia treatment of Amadori products (Horiuchi et al, 1988; Njoroge et al, 1988). These reports demonstrated that pretreatment with alkaline solution or ammonia might overestimate AGE content in the samples.
AGE formation during the incubation of protein with reducing sugar is temperature-dependent (Dawnay and Millar, 1997; Millar et al, 1998; Yeboah et al, 1999). Specifically, CML and pentosidine contents increase in peritoneal dialysis fluid after heat sterilization (Miyata et al, 2000; Ueda et al, 2000). However, the effect of temperature on AGE formation from Amadori products has not yet been studied.
Immunohistochemistry is an important method used to demonstrate the presence of AGE in vivo. The epitope unmasking method by high-temperature process is effective and widely applied for antigen retrieval for immunohistochemical staining on formalin-fixed and paraffin-embedded tissue sections (Shi et al, 1991). Because this method has also been applied in some immunohistological studies on AGE (Horie et al, 1997; Sasaki et al, 1998; Takeda et al, 2001), we speculated that Amadori products might potentially convert into AGE as artifacts by high-temperature treatment of those histological sections, leading to false labeling of the samples as being AGE positive. To investigate this possibility, normal rat skin and liver samples were divided into two portions, half was formalin-fixed, paraffin-embedded and conducted to heat-induced epitope retrieval at 121° C for 10 minutes. The other half was rapidly frozen, followed by the standard staining process but without heat treatment. The reactivity to monoclonal anti-CML antibody was evaluated in heat-treated and heat-untreated sections. To further confirm and demonstrate this possibility in vitro, glycated human serum albumin (HSA), which contained a high level of Amadori products but an undetectable level of CML, was submitted to heat treatment to analyze CML formation by enzyme-linked immunosorbent assay (ELISA) with the anti-CML antibody as well as by high performance liquid chromatography (HPLC). Finally, CML contents of rat liver samples before and after heat treatment were also determined by HPLC to confirm the immunohistochemical result.
Results
Differences in Immunoreactivity of Anti-CML Antibody to Heat-Treated and Untreated Specimens
We first determined whether heat treatment could affect the immunohistochemical identification of CML; two different methods were employed with biopsy samples of normal rat skin and liver. Half of these samples were rapidly frozen and processed for the standard staining, which did not include heat treatment. This resulted in negative staining for CML in the skin (Fig. 1A) and liver (Fig. 1B), indicating the absence of CML in these tissues. In sharp contrast, the other half of these samples that underwent formalin-fixation, paraffin-embedding and autoclaving for antigen retrieval, followed by immunostaining with the anti-CML antibody, showed a strongly positive staining in the cytoplasm of skin epidermal cells and hepatocytes (Fig. 1, C and D), and weakly positive staining in the nuclei of skin epidermal cells (Fig. 1C). The positive immunoreactivity of the anti-CML antibody to autoclaved paraffin sections observed in Figure 1, C and D was completely inhibited when these sections were stained in the presence of excess amounts of CML-modified bovine serum albumin (BSA), antigen of this antibody (Fig. 1, E and F), confirming that CML-modified proteins are specifically stained by the present immunohistochemical method.
Immunoreactivity of the anti-Nε-(carboxymethyl)lysine (CML) antibody to heat-treated and untreated specimens. The biopsy samples of normal rat skin and liver were treated in two different ways. Half of these samples were rapidly frozen and processed for immunostaining with the antibody for CML, which did not include heat treatment. Both, skin (A) and liver (B) were negative for CML. In sharp contrast, the other half of these samples that underwent formalin-fixation, paraffin-embedding autoclaving for antigen retrieval, followed by immunostaining with the antibody, showed a strongly positive staining in skin epidermal cells (C) and hepatocytes (D) and more weakly in the nuclei of the skin epithelial cells (C). The positive immunoreactivity of the anti-CML antibody to autoclaved paraffin sections observed in C and D was completely inhibited when these sections were stained in the presence of 1 mg/ml of CML-BSA (E and F, respectively). Scale bars = 5 μm.
To evaluate the role of formalin fixation on the unexpectedly strong staining observed with the paraffin sections (Fig. 1, C and D), portions of these tissues were treated in the same way as in Figure 1, A and B except that formalin-fixation was performed before rapid freezing, followed by immunostaining with anti-CML antibody. The result showed that the immunostaining pattern of the formalin-fixed and frozen section was indistinguishable from that of the frozen section (nonformalin fixed) (data not shown), indicating that formalin fixation itself is not involved in the strong positive staining of formalin-fixed and autoclaved (heat treated) sections. These data demonstrate it is possible that the heating process of sections might be responsible for these phenomena.
To clarify the role of heat treatment in the positive staining of formalin-fixed, paraffin-embedded, and heat-treated samples of skin (Fig. 1C) and liver (Fig. 1D), sections of skin and liver from the same paraffin blocks were subjected to a similar staining process as in Figure 1, C and D except that the heat-induced epitope retrieval treatment was omitted. Both skin and liver samples resulted in negative staining for CML (data not shown), as was the case with frozen sections (Fig. 1, A and B).
A negative staining was also observed with a control experiment in which formalin-fixed, paraffin-embedded, and heat-treated samples were stained with nonimmune mouse IgG (data not shown). Because the actual absence of CML in those tissues was already confirmed by immunohistochemistry with frozen sections (Fig. 1, A and B), these data reinforce a dominant role of heating in the positive staining of the formalin-treated, paraffin-embedded, and autoclaved samples (Fig. 1, C and D).
Effect of Temperature on CML Formation
Glycated HSA that has high contents of Amadori products but extremely low levels of CML, was submitted to a course of rising temperatures ranging from 30° C to 100° C for 40 minutes. As shown in Figure 2, significant CML formation was detected by noncompetitive ELISA in 80° C-treated samples, and increased steeply at 90° C.
Temperature-dependent CML formation from Amadori products. Glycated human serum albumin (HSA) was incubated for 40 minutes at the indicated temperatures. The wells of the enzyme-linked immunosorbent assay (ELISA) plate were coated with 100 μl of samples (1 μg/ml). The wells were washed and blocked with gelatin, followed by 1-hour reaction with 100 μl of 0.1 μg/ml of the anti-CML antibody. The antibodies bound to wells were visualized by horseradish peroxidase-conjugated anti-mouse IgG as described under “Materials and Methods.”
Time Course of Heat-Facilitated CML Formation
To determine the effect of incubation time on CML formation, glycated HSA was heat treated at 100° C for up to 40 minutes, followed by determination of CML contents by ELISA. As shown in Figure 3, glycated HSA was recognized with anti-CML antibody as early as 5 minutes, and the extent of its reaction steeply increased with time up to 20 minutes, where it reached a plateau level. However, the reaction of this antibody to nonglycated HSA was almost negligible (Fig. 3).
Time course of heat-enhanced CML formation. Glycated HSA and nonglycated HSA were incubated at 100° C for up to 40 minutes. To determine CML contents by ELISA, 1 μg/ml of glycated HSA (closed squares) or nonglycated HSA (open squares) were coated to ELISA plate and incubated for 1 hour, blocked with gelatin, and reacted for 1 hour with 0.1 μg/ml of the anti-CML antibody. The antibodies bound to wells were detected by horseradish peroxidase-conjugated anti-mouse IgG as described under “Materials and Methods.”
Detection of CML by HPLC
To confirm the results of ELISA, CML content was measured in each sample by amino acid analysis. When hippuryl-CML was subjected to acid hydrolysis and amino acid analysis, CML appeared with a retention time of 50.7 minutes (Fig. 4A). CML content of glycated HSA incubated at 100° C for 40 minutes was significantly higher (1.2 mol of CML/mol of HSA) (Fig. 4C) than that of heat-untreated glycated HSA (0.12 mol of CML/mol of CML) (Fig. 4B). In contrast, the CML content of nonglycated HSA incubated at 100° C for 40 minutes was below the detection limit (<0.01 mol of CML/mol of HSA) (Fig. 4D). The time dependence of CML formation on glycated HSA incubated at 100° C was also confirmed by HPLC (Fig. 4E). It is likely, therefore, that the additional formation of CML from Amadori products occurs through the high-temperature treatment.
High performance liquid chromatography (HPLC) analysis of the effect of heat treatment on CML formation from glycated HSA. Glycated HSA and nonglycated HSA were incubated at 100° C for 40 minutes, subjected to acid hydrolysis, and applied to amino acid analysis as described in “Materials and Methods.” When glycated HSA was heat treated, a CML peak eluted at 50.7 minutes (C), which is identical to standard CML (A), could be detected and reached 1.2 mol of CML/mol of HSA. In contrast, formation of CML in heat-treated nonglycated HSA was less than the detection limit (D). Time-dependent CML formation on glycated HSA incubated at 100° C was also detected by HPLC (E)
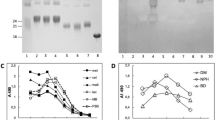
Inhibitory Effects of Metal Chelator, Sodium Borohydride, and Aminoguanidine on CML Formation from Amadori Products
To clarify the pathway involved in the heat-enhanced formation of CML, we determined the effects of metal chelator, NaBH4, and aminoguanidine on CML formation from Amadori products. Glycated HSA was reduced by NaBH4 (132 mm) to hexitollysine, then incubated at 100° C for 40 minutes, followed by determination of CML by ELISA. As shown in Figure 5, CML content in glycated HSA was significantly increased after heat treatment at 100° C for 40 minutes. In contrast, CML formation from NaBH4-reduced-glycated HSA was almost negligible (Fig. 5). Furthermore, diethylenetriamine pentaacetic acid (DTPA), a chelator of transition metal ion, also markedly inhibited CML formation (by >90%, Fig. 5). To examine the contribution of intermediate aldehydes of the Maillard reaction such as glyoxal, methylglyoxal, and 3-deoxyglucosone (Nagai et al, 2000; Thornalley et al, 1999), glycated HSA was incubated at 100° C in the presence of 90 mm of aminoguanidine, a trapping reagent for α-oxoaldehydes reacting with aminoguanidine to form aminotriazine derivatives, and determined CML content by ELISA. Enhanced formation of CML by heat treatment was inhibited by aminoguanidine (Fig. 5). Because CML was not detected in NaBH4-reduced glycated HSA, it is likely that CML was formed from the conversion of Amadori products.
Inhibitory effects of metal chelator, NaBH4-reduction, and aminoguanidine on CML formation from Amadori products. Glycated HSA was incubated at 100° C for 40 minutes with or without 132 mm of NaBH4, 1 mm of diethylenetriamine pentaacetic acid (DTPA), or 90 mm of aminoguanidine. The CML content was determined by noncompetitive ELISA as described in Figure 2.
Detection of α-Oxoaldehydes by 2, 3-Diaminonaphthalene (DAN)
Because CML formation from glycated HSA was significantly inhibited in the presence of aminoguanidine, we next determined whether reactive aldehydes were generated as intermediates for CML formation from glycated HSA by the heating process. When glycated HSA was incubated at 100° C for 40 minutes in the presence of 10 mm of DAN, four separated peaks emerged at 7.1, 9.8, 27.8, and 39.1 minutes. These peaks were identified at 7.1 minutes as glucosone, at 9.8 minutes as 3-deoxyglucosone, at 27.8 minutes as glyoxal, and at 39.1 minutes as methylglyoxal. Time-course study demonstrated that the generation of each aldehyde was increased in a time-dependent manner (Fig. 6). At the end of 40 minutes of incubation at 100° C, the concentration of these compounds generated were 14.38 μm for glucosone, 23.41 μm for 3-deoxyglucosone, 5.77 μm for glyoxal, and 17.01 μm for methylglyoxal.
Detection of α-oxoaldehydes by 2,3-diaminonaphthalene (DAN). Glycated HSA was incubated in the presence of 10 mm of DAN, and α-oxoaldehydes-DAN adducts were identified on reverse-phase HPLC as described under “Material and Methods.” Time-course study demonstrated that the generation of each aldehyde was time dependent. At the end of 40 minutes of incubation at 100° C, the concentration of these compounds generated were 14.38 μm for glucosone, 23.41 μm for 3-deoxyglucosone, 5.77 μm for glyoxal, and 17.01 μm for methylglyoxal.
Quantification of CML Contents by HPLC in Heat-Treated Rat Liver Samples
Finally, to obtain much solid evidence that CML detected by immunohistochemical study after the high-temperature unmasking method (Fig. 1, C and D) was not the retrieved antigen of the embedded tissue but was derived from Amadori products, CML contents of rat liver samples before and after heat treatment were quantitated by HPLC. Whereas CML in the nonheated rat liver sample was below detection levels (Fig. 7A), the autoclaved sample showed a high level of CML (21 mmol of CML/mol of lysine) (Fig. 7B). In sharp contrast, when the sample was pretreated with NaBH4 before heat treatment, the marked increase in CML content was significantly suppressed (1.03 mmol of CML/mol of lysine) (Fig. 7C). These quantitative results give convincing support to the notion that conversion of Amadori product to CML in the tissue sample’s CML occurs through heating.
Quantification of CML contents by HPLC in heat-treated rat liver samples. The rat liver slices were homogenized in two ways: one in 50 mm phosphate buffer pH 7.4 and the other in the same buffer plus 1 mm DTPA as described under “Methods and Materials.” The sample homogenized in phosphate buffer was autoclaved for 30 minutes (121° C) (B), and the other was treated with 50 mm NaBH4 for 2 hours at 37° C before autoclaving under identical conditions (C). The sample homogenized in 50 mm phosphate buffer in the presence of 1 mm DTPA was used to determine CML contents of nonheated samples (A). HPLC analyses were performed in identical way as in Figure 4. CML contents measured by these analyses were 21 mmol of CML/mol of lysine for B, 1.03 mmol of CML/mol of lysine for C, and below a detection level for A.
Discussion
In the present study, the high-temperature heating process was conducted as antigen retrieval for immunohistochemical staining of formalin-fixed, paraffin-embedded tissue sections because of the effectiveness of this technique in enhancing the staining for a wide range of antibodies (Shi et al, 1997; Taylor et al, 1996) and some immunohistochemical studies employed to identify AGE structures in various tissues. During fixation of the histological sample, biochemical studies indicated that hydrolysis of cross-linkages between formalin and protein is limited by certain amino acid residues, such as imidazole and indol, but that these cross-linkages can be reversed by high-temperature heating (121° C) (Fraenkel-Conrat and Olcot, 1948). However, over-treatment by prolonged heating may also result in false-positive or undesirable high background staining (Ezaki, 2000). Furthermore, it has long been known that AGE formation during incubation of proteins with glucose is enhanced temperature dependently because this early reaction depends on the reactivity between aldehyde of glucose and amino residues of amino acids such as lysine, histidine, and arginine. However, whether temperature is involved in the conversion of Amadori products to AGE structures has not been investigated.
The evident immunoreactivity of the tissues that were formalin-fixed, paraffin-embedded, and submitted to the high-temperature unmasking method to the anti-CML antibody, in comparison with the frozen tissues, implicates the involvement of temperature as an important factor for that difference. To confirm these results in vitro, CML, a major AGE structure identified in vivo, generated from glycated HSA (a model Amadori-rich protein) was determined by immunochemistry using the anti-CML antibody as well as by HPLC (Fig. 4). The experiments showing the direct correlation of rising temperature (Fig. 2) and incubation time (Fig. 3) with the amount of CML formed from Amadori products reinforces the role of temperature in this process. The results for other AGE structures such as Nε-(carboxyethyl)lysine, pyrraline, and pentosidine were negative by ELISA in heated glycated HSA (data not shown). Because paraffin-embedded tissue sections were submitted to 121° C for up to 20 minutes with the normal unmasking procedure (Sasaki et al, 1998), glycated HSA was also submitted to autoclaving (121° C), followed by determination of CML. The reactivity of the antibody to glycated HSA was significantly enhanced after autoclave treatment (data not shown). These in vitro results confirm that CML was generated from Amadori products under the condition used for unmasking.
To clarify the pathway of CML formation under heat treatment, glycated HSA was reduced by sodium borohydride to convert the Amadori product in hexitollysine and incubated under the same conditions. Because CML was not detected after heating using borohydride-reduced glycated HSA, it is therefore likely that CML was generated by conversion of Amadori product.
Because metal-induced oxidative cleavage of Amadori product is considered to play a major role in CML formation (Nagai et al, 1997; Wells-Knecht et al, 1995b), we next determined the involvement of oxidation in CML formation during the heating process by adding metal chelator. The formation of CML from glycated HSA was significantly inhibited by DTPA (Fig. 5), indicating that oxidation contributed to CML formation during the heating process. We also reported previously that CML formation from Amadori product is highly accelerated under alkaline conditions (Nagai et al, 1998). The possibility of the influence of this factor in our experiment was excluded because the pH of the samples of glycated HSA before and after incubation was neutral (data not shown).
Aminoguanidine, a potent α-oxoaldehydes trapping reagent and inhibitor of AGE formation (Brownlee et al, 1986), significantly inhibited the heat-enhanced CML formation (Fig. 5), indicating that α-oxoaldehydes could be generated through the incubation of glycated HSA and become involved in further CML formation. To address the contribution of α-oxoaldehydes to CML formation from Amadori products, glycated HSA was incubated at 100° C with DAN, an α-oxoalde-hydes trapping reagent, followed by determination of α-oxoaldehydes by HPLC, which lead us to detect 3-deoxyglucosone, methylglyoxal, glyoxal, and glucosone (Fig. 6). Although α-oxoaldehydes, such as 3-deoxyglucosone (Hayase et al, 1995; Niwa et al, 1998; Zyzak et al, 1995), glyoxal (Glomb and Monnier, 1995; Reddy et al, 1995; Wells-Knecht et al, 1995a, 1995b), and methylglyoxal (Lo et al, 1994; Thornalley et al, 1999, 2000) were already pointed as important precursors for AGE formation, our results suggested that glucosone might also play an important role in the formation of CML because 14.38 μm of glucosone was detected after incubation of glycated HSA at 100° C for 40 minutes (Fig. 6).
Miyata et al (2000) demonstrated that peritoneal dialysis fluid, which contains 76 mm of glucose, generated abundant 3-deoxyglucosone, glyoxal and methylglyoxal, after heat sterilization. In the present study, we demonstrated for the first time that 3-deoxyglucosone, methylglyoxal, glyoxal, and glucosone were generated from Amadori products by heating and further contributed to AGE formation, as illustrated in Figure 8. Among aldehydes detected in the present study, glucosone, 3-deoxyglucosone, and glyoxal are known as a precursor for CML formation, whereas methylglyoxal gives rise to other AGE-structures such as Nε-(carboxyethyl)lysine (Ahmed et al, 1997), imidazolone (Thornalley, 1996), methylglyoxal lysine dimer (Frye et al, 1998), and argpyrimidine (Oya et al, 1999). As shown in Figure 8, possible pathways for CML formation from Amadori products by heating are two-fold. First, heating enhances the oxidative cleavage of Amadori products between C2 and C3 of the carbohydrate chain, which directly leads to generation of CML-protein adduct (pathway A). Second, these α-oxoaldehydes react with amino groups of proteins to form CML-modified proteins (pathway B). Because heating-accelerated CML formation from Amadori products significantly inhibited aminoguanidine (>70%) (Fig. 5), pathway B may play a dominant role in the formation of CML from Amadori products by short-term heating.
Possible pathways of CML formation from Amadori product by heating. Two pathways could explain heating-enhanced CML formation from Amadori products. Because 3-deoxyglucosone, methylglyoxal, glyoxal, and glucosone were generated from glycated HSA (Amadori products) by heating, CML is generated not only by direct cleavage of Amadori products (pathway A) but also by contribution of reactive intermediates (pathway B). In pathway A, heating enhances the oxidative cleavage of Amadori products between C2 and C3 of carbohydrate chain, which directly leads to generation of CML-proteins. In pathway B, heating enhances the generation of glucosone, 3-deoxyglucosone, and glyoxal from the cleavage reaction of Amadori products. These α-oxoaldehydes then react with epsiron amino residues of lysine on proteins to form CML-proteins (pathway B). See text for details.
It is known that the early stages of the Maillard reaction progress under physiological conditions and most of proteins occur in vivo as adducts with Amadori products. Our results demonstrated that CML formation from Amadori products is enhanced by heat treatment in vitro. This notion was also confirmed by quantitative analysis of rat liver samples (Fig. 7). Taken together, results of the present study may well explain false-positive results observed in the immunohistochemical study with the anti-CML antibody after antigen retrieval by heating.
Materials and Methods
Chemicals
D-glucose and HSA (fraction V) were purchased from Sigma (St. Louis, Missouri). Aminoguanidinium chlo-ride was purchased from Wako (Osaka, Japan). DTPA and DAN were purchased from Dojindo Labora-tories (Kumamoto, Japan). 1-Ethyl-3-(3-Dimethylamino-propyl) carbodiimide hydrochloride was purchased from Pierce (Rockford, Illinois). Horseradish peroxidase-conjugated goat anti-mouse IgG antibody was purchased from Kirkegaard Perry Laboratories (Gaithersburg, Maryland). Microtitration plates (96-well, Nunc Immunoplate-maxisorp) were purchased from Nippon Inter Med (Tokyo, Japan). Glyoxal was obtained from Nakarai Chemicals (Kyoto, Japan) and methylglyoxal from Sigma. All other chemicals were of the best grade available from commercial sources.
Tissue Preparation
The skin and liver samples were obtained from a male Wistar rat that was 7 weeks old. Each sample was sectioned in two and processed using two different methods: the first section was formalin-fixed and paraffin-embedded, the other was rapidly frozen and stored at −80° C. In addition, the rat samples were also formalin-fixed, rapidly frozen, and stored at −80° C.
The remaining liver from the same rat was used as a sample for CML quantification by HPLC analysis. The tissue was minced and delipidized with chloroform and methanol (2:1, vol/vol) by mild shaking overnight at 4° C. The solvent was removed by suction, and pellets were washed three times with methanol and three more times with deionized water. We did not use collagenase for digestion of the tissue because it contained CML detected by ELISA (data not shown). The pellets were divided into two portions, one homogenized, on ice, in 50 mm phosphate buffer pH 7.4, and the other in the same buffer plus 1 mm DTPA. They were centrifuged at 8000 g for 15 minutes at 4° C (Ling et al, 2001). The protein concentration of the supernatant was measured by bicinchoninic acid assay with BSA as the standard (Pierce, Rockford, Illinois) (Smith et al, 1985; Wiechelman et al, 1988). An aliquot of the sample homogenized with phosphate buffer was autoclaved for 30 minutes (121° C), and the other was treated with 50 mm NaBH4 for 2 hours at 37° C before autoclaving under identical conditions. The rat liver sample homogenized in 50 mm phosphate buffer in the presence of 1 mm DTPA described above was used to determine CML contents of the nonheated sample.
Preparation of the Monoclonal Anti-CML Antibody
The experimental protocol was approved by the local ethics review committee for animal experimentation. The monoclonal anti-AGE antibody named 6D12 was prepared in mice using AGE-modified BSA as an antigen (Horiuchi et al, 1991) and purified by protein G affinity chromatography to IgG1. Our subsequent study revealed that this antibody recognizes CML-protein adduct (Ikeda et al, 1996).
Immunohistochemical Studies
The rapidly frozen samples, a portion nonfixed and another portion prefixed with formalin, were sectioned into 4 μm, air-dried, and fixed in 100% ice-cold acetone for 5 minutes. These sections were washed three times with phosphate buffer saline (PBS) and incubated overnight at 4° C with the anti-CML antibody (0.5 μg/ml) as the primary antibody, washed again three times with PBS, then incubated at room temperature for 30 minutes with biotinylated horse anti-mouse IgG antibody (Vector Laboratories, Burlingame, California). The sections were washed again three times with PBS, and endogenous peroxidase was inactivated by incubating the sections with 0.3% hydrogen peroxide in methanol for 30 minutes. Immunoreaction was detected with the avidin-biotin-horseradish peroxidase complex (Vector Laboratories), using 4-dimethylaminobenazobenzene as chromagen. Hematoxylin was used as the contrast staining. Nonimmune mouse IgG (DAKO, Glostrup, Denmark) was used as a negative control. To evaluate the specific immunoreactivity of the anti-CML antibody to CML, the tissue specimens were immunostained with the antibody (1 μg/ml) in the presence of 100 μg CML-BSA. CML-BSA was prepared by incubating BSA with glyoxylic acid and NaCNBH3 as described previously (Ikeda et al, 1996).
The paraffin-embedded sections (4-μm thick) were dried, deparaffinized, and unmasked by autoclaving for 10 minutes (121° C) in 2 mm acetic acid solution. One set of tissue sections was not autoclaved. After washing twice with PBS, endogenous peroxidase was inactivated by incubating the sections with 0.3% H2O2 in methanol for 30 minutes. These sections were washed three times with PBS and incubated overnight at 4° C with the anti-CML antibody (0.5 μg/ml) as the primary antibody. The following day, they were washed three times with PBS, and the sections were incubated at room temperature for 30 minutes with biotinylated horse anti-mouse IgG antibody (Vector Laboratories). Immunoreaction was detected with the avidin-biotin-horseradish peroxidase complex (Vector Laboratories), using 4-dimethylaminobenazobenzene as chromagen. Hematoxylin was used as the contrast staining. Nonimmune mouse IgG was used as a negative control. The specific immunoreactivity of the antibody to CML was also evaluated in the same way.
Preparation of Glycated and Nonglycated HSA
Glycated HSA and nonglycated HSA were prepared as described previously (Nagai et al, 1997). Briefly, 50 mg/ml of HSA was incubated at 37° C for 7 days with 1.6 M glucose in 10 ml of 50 mm sodium phosphate buffer (pH 7.2) in the presence of 2 mm DTPA, followed by dialysis against 50 mm sodium phosphate buffer (pH 7.2). Amino acid analyses showed that 21.9 out of 59 lysine residues were modified by glucose in glycated HSA. The fructosamine contents of glycated HSA (30 mg/ml), determined by fructosamine assay kit (Boehringer Mannheim, Mannheim, Germany), was 1186 μmol/l. To prepare nonglycated HSA, 1.0 g of HSA was dissolved in 300 ml of 0.5 M glycine-NaOH buffer (pH 8.5) in the presence of 2% MgCl2, mixed with 500 ml of phenyl boronic acid resin (PBA-60, Amicon, Beverly, Massachusetts) and incubated for 2 hours at room temperature, followed by filtration through a glass filter. The obtained solution was concentrated to 30 mg/ml by an ultrafiltration system and used for the experiments. The level of fructosamine in the nonglycated HSA (30 mg/ml) was negligible (10.9 μmol/L).
Preparation of 3-Deoxyglucosone
3-deoxyglucosone was prepared as described previously (Hayase et al, 1995). Briefly, a solution of D-glucose (20 g) and p-toluidine (11 g) in a mixture of 95% of ethanol (450 ml) and acetic acid (22 ml) was boiled under reflux for 30 minutes. To this solution was added benzoylhydrazine (33 g), and reflux was continued for 7 hours. The solution was allowed to cool to room temperature with stirring for 12 hours. The insoluble materials were separated by filtration, washed three times with 100 ml of methanol, three times with 100 ml of ether, and three times with 100 ml of methanol, and dried under reduced pressure, to yield 19 g of material. The crude product of 3-deoxy-d-erythro-hexos-2-urose bis(benzoylhydrazone) monohydrate was recrystallized from 95% ethanol. A suspension of bishydrazone monohydrate (5 g) in ethanol (150 ml), water (250 ml), acetic acid (1.5 ml), and freshly distilled benzaldehyde (8 ml) was boiled under reflux. The reaction was terminated by evaporation within 30 minutes, and the solution remained clear for an additional 30 minutes, at which time benzaldehyde benzoylhydrazone began to precipitate. Reflux was then continued for an additional 1.5 hours. With the concurrent addition of water (250 ml), 250 ml of distillate was collected in less than 30 minutes. The mixture was cooled and filtered, the filtrate was neutralized with Dowex 1 (CO32-) anion-exchange resin (The Dow Chemical Company, Midland, Michigan), and the mixture was filtered again. The filtrate was concentrated under low pressure to 100 ml, washed three times with 50 ml of ether, treated with activated charcoal, filtered, and evaporated under low pressure to a thick syrup. This material was dissolved in water (2 ml), and hot ethanol (50 ml, 50° C), filtered, and stirred with a mixture of Dowex 1 and Dowex 50W ion-exchange resin. The mixture was filtered, and the filtrate was concentrated under low pressure, frozen, and lyophilized to give an amorphous 3-deoxy-glucosone powder (1.7 g). The structure was confirmed by proton nuclear magnetic resonance.
Preparation of Glucosone
Glucosone (D-arabino-hexosulose) was synthesized as described previously (Whistler and Wolfrom, 1963), with some modifications. Briefly, D-arabino-hexose phenylosazone (6.5g), suspended in 200 ml of ethanol (99%), was mixed with 300 ml of distilled water in a 1 L round flask with a condenser. Acetic acid (7.6 ml) and distilled benzaldehyde (10.2 ml) were added, and the mixture was refluxed. After 3 hours, osazone dissolved completely, and the solution remained clear for a short time before precipitation of benzaldehyde phenylhydrazone began. From this stage, reflux was continued 90 minutes, then 50 ml of water was added. The mixture was evaporated under reduced pressure to remove ethanol and allowed to cool overnight at 2° C before the benzaldehyde phenylhydrazone was removed by filtration with suction. The filtrate was evaporated under reduced pressure to 100 ml, cooled, washed 10 times with 50 ml of ether, and evaporated under reduced pressure to remove the dissolved ether. Ten milliliters of this aqueous solution was treated with activated carbon. The carbon was removed by filtration with suction, and the filtrate was evaporated under reduced pressure to a thick syrup. The syrup was dissolved in 10 ml of water, and then charged on an ion exchange resine column (Amberlite IR-120; H+, 30 ml; Mallinckrott Chemicals, Phillipsburg, New Jersey). The eluate was lyophilized and then dissolved in a small quantity of ethylacetate, methanol:water (3:1:1). Then glucosone was further purified on a flash column (silica gel 60, 6 cm × 20 cm) with the above solvent system. The fast atom bombardment (negative)-mass spectrometry spectrum for glucosone showed an (M-H)− ion at m/z = 177.
Preparation of Samples
To determine the effect of temperature on CML formation in vitro, glycated HSA (2 mg/ml) was incubated at the indicated temperatures for 40 minutes, and the immunoreactivities of these samples to the anti-CML antibody were determined by noncompetitive ELISA. Under the same experimental conditions, the time course of CML formation at 100° C was also determined by noncompetitive ELISA. To confirm the contribution of Amadori product on CML formation, glycated HSA was reduced by 132 mm of NaBH4 to hexitollysine, followed by incubation at 100° C for 40 minutes. To clarify the pathway involved in this process, glycated HSA was incubated for 40 minutes at 100° C in the presence of DTPA (1 mm) or aminoguanidinium (90 mm), followed by determination of CML by noncompetitive ELISA using the antibody. For negative control, nonglycated HSA (2 mg/ml) was also incubated at 100° C for 40 minutes to verify the immunoreactivity to the anti-CML antibody.
Enzyme-Linked Immunosorbent Assay
ELISA was performed as described previously (Ikeda et al, 1996; Nagai et al, 1997). Briefly, each well of a 96-well microtiter plate was coated with 100 μl of the sample to be tested in 50 mm sodium carbonate buffer (pH 9.6), blocked with 0.5% gelatin, and washed three times with PBS containing 0.05% Tween 20 (washing buffer; Wako, Osaka, Japan). Wells were incubated for 1 hour with 0.1 ml of the anti-CML antibody (0.1 μg/ml) dissolved in washing buffer. The wells were then washed three times with washing buffer and reacted with horseradish peroxidase-conjugated anti-mouse IgG antibody (Kirkegaard and Perry Laboratories), followed by reaction with 1,2-phenylenediamine dihydrochloride. The reaction was terminated by 1.0 M sulfuric acid, and the absorbance at 492 nm was read by a micro-ELISA plate reader.
Detection of CML by HPLC
The CML content in the glycated HSA and in homogenized rat liver samples were quantified by amino acid analysis after acid hydrolysis with 6 N HCl for 24 hours at 110° C in an amino acid analyzer (L-8500A, Hitachi, Tokyo) equipped with an ion exchange HPLC column (#2622 SC, 4.6 ′ 80 mm, Hitachi) and the ninhydrin post-column detecting system as described previously (Nagai et al, 2000). Hippuryl-CML was prepared by incubating hippuryllysine (benzoylglycyllysine, Peptide Institute, Osaka, Japan) with glyoxylic acid and NaCNBH3 as described previously (Nagai et al, 1998) and was used as a standard CML.
Detection of α-Oxoaldehydes by DAN
Reactive α-oxoaldehydes including glucosone, 3-deoxyglucosone, methylglyoxal, and glyoxal were determined by DAN as described previously (Yamada H et al, 1994). Briefly, 2 mg/ml of glycated HSA was incubated in PBS in the presence of DAN (10 mm) at 100° C for up to 40 minutes. The aldehyde-DAN adducts were analyzed with HPLC (Hitachi) using a reverse phase column (Cat. #25546–96, Mightysil, RP-18 GP 150–3.0, 3 μm; Cica-Reagent, Tokyo, Japan). Effluents were monitored by fluorescence at Ex. 271 nm/Em. 503 nm. All analyses were performed at 40° C at an elution rate of 0.4 ml/minutes using as elution buffer composed of 70% phosphoric acid (50 mm), 15% methanol, and 15% acetonitrile. The glucosone-DAN, methylglyoxal-DAN, and glyoxal-DAN adducts were prepared by incubating the respective aldehydes (1 mm) with DAN (10 mm) at 100° C for each period of the analyzed time course as the standards.
References
Ahmed MU, Brinkmann Frye E, Degenhardt TP, Thorpe SR, and Baynes JW (1997). N-epsilon-(carboxyethyl)lysine, a product of the chemical modification of proteins by methylglyoxal, increases with age in human lens proteins. Biochem J 324: 565–570.
Ahmed MU, Thorpe SR, and Baynes JW (1986). Identification of Ne-carboxymethyllysine as a degradation product of fructoselysine in glycated protein. J Biol Chem 261: 4889–4894.
Ando K, Beppu M, Kikugawa K, Nagai R, and Horiuchi S (1999). Membrane proteins of human erythrocytes are modified by advanced glycation end products during aging in the circulation. Biochem Biophys Res Commun 258: 123–127.
Araki N, Ueno N, Chakrabarti B, Morino Y, and Horiuchi S (1992). Immunochemical evidence for the presence of advanced glycation end products in human lens proteins and its positive correlation with aging. J Biol Chem 267: 10211–10214.
Brownlee M, Vlassara H, Kooney A, Ulrich P, and Cerami A (1986). Aminoguanidine prevents diabetes-induced arterial wall protein cross-linking. Science 232: 1629–1632.
Bucala R, Makita Z, Koschinsky T, Cerami A, and Vlassara H (1993). Lipid advanced glycosylation: Pathway for lipid oxidation in vivo. Proc Natl Acad Sci USA 90: 6434–6438.
Chang JC, Ulrich PC, Bucala R, and Cerami A (1985). Detection of an advanced glycosylation product bound to protein in situ. J Biol Chem 260: 7970–7974.
Dawnay AB and Millar DJ (1997). Glycation and advanced glycation end-product formation with icodextrin and dextrose. Perit Dial Int 17: 52–58.
Ezaki T (2000). Antigen retrieval on formaldehyde-fixed paraffin sections: Its potential drawbacks and optimization for double immunostaining. Micron 31: 639–649.
Fraenkel-Conrat H and Olcot HS (1948). Reaction of formaldehyde with proteins. VI. Cross-linking of amino groups with phenol, imidazole, or indole groups. J Biol Chem 174: 827–843.
Frye EB, Degenhardt TP, Thorpe SR, and Baynes JW (1998). Role of the Maillard reaction in aging of tissue proteins. Advanced glycation end product-dependent increase in imidazolium cross-links in human lens proteins. J Biol Chem 273: 18714–18719.
Glomb MA and Monnier VM (1995). Mechanism of protein modification by glyoxal and glycolaldehyde, reactive intermediates of the Maillard reaction. J Biol Chem 270: 10017–10026.
Hammes HP, Weiss A, Hess S, Araki N, Horiuchi S, Brownlee M, and Preissner KT (1996). Modification of vitronectin by advanced glycation alters functional properties in vitro and in the diabetic retina. Lab Invest 75: 325–338.
Hayase F, Konishi Y, and Kato H (1995). Identification of the modified structure of arginine residues in proteins with 3-deoxyglucosone, a Maillard reaction intermediate. Biosci Biotechnol Biochem 59: 1407–1411.
Hayase F, Nagaraj RH, Miyata S, Njoroge FG, and Monnier VM (1989). Aging of proteins: immunological detection of a glucose-derived pyrrole formed during Maillard reaction in vivo. J Biol Chem 264: 3758–3764.
Horie K, Miyata T, Maeda K, Miyata S, Sugiyama S, Sakai H, Strihou CY, Monnier VM, Witztum JL, and Kurokawa K (1997). Immunohistochemical colocalization of glycoxidation products and lipid peroxidation products in diabetic renal glomerular lesions. Implication for glycoxidative stress in the pathogenesis of diabetic nephropathy. J Clin Invest 100: 2995–3004.
Horiuchi S, Araki N, and Morino Y (1991). Immunochemical approach to characterize advanced glycation end products of the Maillard reaction: Evidence for the presence of a common structure. J Biol Chem 266: 7329–7332.
Horiuchi S, Shiga M, Araki N, Takata K, Saitoh M, and Morino Y (1988). Evidence against in vivo presence of 2-(2-furoyl)-4(5)-(2-furanyl)-1H-imidazole, a major fluorescent advanced end product generated by nonenzymatic glycosylation. J Biol Chem 263: 18821–18826.
Hoshii Y, Kawano H, Gondo T, Takahashi M, Ishihara T, Higuchi K, and Horiuchi S (1996). Immunohistochemical study with anti-advanced glycation end-products antibody in murine amyloidosis. Pathol Int 46: 738–742.
Iijima K, Murata M, Takahara H, Irie S, and Fujimoto D (2000). Identification of N(omega)-carboxymethylarginine as a novel acid-labile advanced glycation end product in collagen. Biochem J 347: 23–27.
Ikeda K, Higashi T, Sano H, Jinnouchi Y, Yoshida M, Araki T, Ueda S, and Horiuchi S (1996). Ne-(carboxymethyl)lysine protein adduct is a major immunological epitope in proteins modified with advanced glycation end products of the Maillard reaction. Biochemistry 35: 8075–8083.
Imai N, Nishi S, Suzuki Y, Karasawa R, Ueno M, Shimada H, Kawashima S, Nakamaru T, Miyakawa Y, Araki N, Horiuchi S, Gejyo F, and Arakawa M (1997). Histological localization of advanced glycosylation end products in the progression of diabetic nephropathy. Nephron 76: 153–160.
Kimura T, Takamatsu J, Araki N, Goto M, Kondo A, Miyakawa T, and Horiuchi S (1995). Are advanced glycation end-products associated with amyloidosis in Alzheimer’s disease? NeuroReport 6: 866–868.
Kimura T, Takamatsu J, Ikeda K, Kondo A, Miyakawa T, and Horiuchi S (1996). Accumulation of advanced glycation end products of the Maillard reaction with age in human hippocampal neurons. Neurosci Lett 208: 53–56.
Konishi Y, Hayase F, and Kato H (1994). Novel imidazolones compound formed by the advanced Maillard reaction of 3-deoxyglucosone and arginine residues in proteins. Biosci Biotechnol Biochem 58: 1953–1955.
Kume S, Takeya M, Mori T, Araki N, Suzuki H, Horiuchi S, Kodama T, Miyauchi Y, and Takahashi K (1995). Immunohistochemical and ultrastructural detection of advanced glycation end products in atherosclerotic lesions of human aorta with a novel specific monoclonal antibody. Am J Pathol 147: 654–667.
Ling X, Nagai R, Sakashita N, Takeya M, Horiuchi S, and Takahashi K (2001). Immunohistochemical distribution and quantitative biochemical detection of advanced glycation end products in fetal to adult rats and in rats with streptozotocin-induced diabetes. Lab Invest 81: 845–861.
Lo TW, Westwood ME, McLellan AC, Selwood T, and Thornalley PJ (1994). Binding and modification of proteins by methylglyoxal under physiological conditions. A kinetic and mechanistic study with N alpha-acetylarginine, N alpha-acetylcysteine, and N alpha-acetyllysine, and bovine serum albumin. J Biol Chem 269: 32299–32305.
Maillard LC (1912). Action des acides amines sur les sucres: Formation des melanoidines par voie methodique. C R Acad Sci (Paris) 154: 66–68.
Makino H, Shikata K, Hironaka K, Kushiro M, Yamasaki Y, Sugimoto H, Ota Z, Araki N, and Horiuchi S (1995). Ultrastructure of nonenzymatically glycated mesangial matrix in diabetic nephropathy. Kidney Int 48: 517–526.
Makita Z, Vlassara H, Cerami A, and Bucala R (1992a). Immunochemical detection of advanced glycosylation end products in vivo. J Biol Chem 267: 5133–5138.
Makita Z, Vlassara H, Rayfield E, Cartwright K, Friedman E, Rodby R, Cerami A, and Bucala R (1992b). Hemoglobin-AGE: A circulating marker of advanced glycosylation. Science 258: 651–653.
Matsuse T, Ohga E, Teramoto S, Fukayama M, Nagai R, Horiuchi S, and Ouchi Y (1998). Immunohistochemical localization of advanced glycation end products in pulmonary fibrosis. J Clin Pathol 51: 515–519.
Meng J, Sakata N, Takebayashi S, Asano T, Futata T, Araki N, and Horiuchi S (1996). Advanced glycation end products of the Maillard reaction in aortic pepsin-insoluble and pepsin-soluble collagen from diabetic rats. Diabetes 45: 1037–1043.
Meng J, Sakata N, Takebayashi S, Asano T, Futata T, Nagai R, Ikeda K, and Horiuchi S, Myint T, and Taniguchi N (1998). Glycoxidation in aortic collagen from STZ-induced diabetic rats and its relevance to vascular damage. Atherosclerosis 136: 355–365.
Millar DJ, Holmes C, Faict D, and Dawnay A (1998). Comparison of in vitro AGE formation between standard PD fluid and a novel bicarbonate/lactate formulation. Adv Perit Dial 14: 191–194.
Mitsuhashi T, Nakayama H, Itoh T, Kuwajima S, Aoki S, Atsumi T, and Koike T (1993). Immunochemical detection of advanced glycation end products in renal cortex from STZ-induced diabetic rat. Diabetes 42: 826–832.
Miyata T, Horie K, Ueda Y, Fujita Y, Izuhara Y, Hirano H, Uchida K, Saito A, van Ypersele de Strihou C, and Kurokawa K (2000). Advanced glycation and lipidoxidation of the peritoneal membrane: Respective roles of serum and peritoneal fluid reactive carbonyl compounds. Kidney Int 58: 425–435.
Miyata T, Oda O, Inagi R, Iida Y, Araki N, Yamada N, Horiuchi S, Taniguchi N, Maeda K, and Kinoshita T (1993). Beta 2-mcroglobulin modified with advanced glycation end products is a major component of hemodialysis-associated amyloidosis. J Clin Invest 92: 1243–1252.
Miyata T, Taneda S, Kawai R, Ueda Y, Horiuchi S, Hara M, Maeda K, and Monnier VM (1996). Identification of pentosidine as a native structure for advanced glycation end products in b2-microglobulin-containing amyloid fibrils in patients with dialysis-related amyloidosis. Proc Natl Acad Sci USA 93: 2353–2358.
Mizutari K, Ono T, Ikeda K, Kayashima K, and Horiuchi S (1997). Photo-enhanced modification of human skin elastin in actinic elastosis by N(epsilon)-(carboxymethyl)lysine, one of the glycoxidation products of the Maillard reaction. J Invest Dermatol 108: 797–802.
Morita H, Shinzato T, Cai Z, Horiuchi S, and Maeda K (1996). Immunohistochemical localization of beta 2-microglobulin and advanced glycation end products in amyloid-enriched carpal tunnel ligament. Nephron 73: 117–118.
Nagai R, Ikeda K, Higashi T, Sano H, Jinnouchi Y, Araki T, and Horiuchi S (1997). Hydroxyl radical mediates N epsilon-(carboxymethyl)lysine formation from Amadori product. Biochem Biophys Res Commun 234: 167–172.
Nagai R, Ikeda K, Kawasaki Y, Sano H, Yoshida M, Araki T, Ueda S, and Horiuchi S (1998). Conversion of Amadori product of Maillard reaction to Nepsilon-(carboxy-methyl)lysine in alkaline condition. FEBS Lett 425: 355–360.
Nagai R, Matsumoto K, Ling X, Suzuki H, Araki T, and Horiuchi S (2000). Glycolaldehyde, a reactive intermediate for advanced glycation end products, plays an important role in the generation of an active ligand for the macrophage scavenger receptor. Diabetes 49: 1714–1723.
Nakamura K, Hasegawa T, Fukunaga Y, and Ienaga K (1992). Crosslines A and B as candidates for the fluorophores in age- and diabetes-related cross-linked proteins, and their diacetates produced by Maillard reaction of a-N-acetyl-L-lysine with D-glucose. J Chem Soc Chem Commun 14: 992–994.
Nakamura K, Nakazawa Y, and Ienaga K (1997). Acid-stable fluorescent advanced glycation end products: Vesperlysines A, B, and C are formed as crosslinked products in the Maillard reaction between lysine or proteins with glucose. Biochem Biophys Res Commun 232: 227–230.
Nakamura Y, Horii Y, Nishino T, Shiiki H, Sakaguchi Y, Kagoshima T, Dohi K, Makita Z, Vlassara H, and Bucala R (1993). Immunohistochemical localization of advanced glycosylation endproducts in coronary atheroma and cardiac tissue in diabetes mellitus. Am J Pathol 143: 1649–1656.
Nakayama H, Mitsuhashi T, Kuwajima S, Aoki S, Kuroda Y, Itoh T, and Nakagawa S (1993). Immunochemical detection of advanced glycation end products in lens crystallins from streptozocin-induced diabetic rat. Diabetes 42: 345–350.
Nakayama M, Kawaguchi Y, Yamada K, Hasegawa T, Takazoe K, Katoh N, Hayakawa H, Osaka N, Yamamoto H, Ogawa A, Kubo H, Shigematsu T, Sakai O, and Horiuchi S (1997). Immunohistochemical detection of advanced glycosylation end-products in the peritoneum and its possible pathophysiological role in CAPD. Kidney Int 51: 182–186.
Niwa H, Takeda A, Wakai M, Miyata T, Yasuda Y, Mitsuma T, Kurokawa K, and Sobue G (1998). Accelerated formation of N epsilon-(carboxymethyl) lysine, an advanced glycation end product, by glyoxal and 3-deoxyglucosone in cultured rat sensory neurons. Biochem Biophys Res Commun 248: 93–97.
Njoroge FG, Fernandes AA, and Monnier VM (1988). Mechanism of formation of the putative advanced glycosylation end product and protein cross-link 2-(2-furoyl)-4(5)-(2-furanyl)-1H-imidazole. J Biol Chem 263: 10646–10652.
Oya T, Hattori N, Mizuno Y, Miyata S, Maeda S, Osawa T, and Uchida K (1999). Methylglyoxal modification of protein. J Biol Chem 274: 18492–18502.
Pongor S, Ulrich PC, Bencsath FA, and Cerami A (1984). Aging of proteins: Isolation and identification of a fluorescent chromophore from the reaction of polypeptides with glucose. Proc Natl Acad Sci USA 81: 2684–2688.
Reddy S, Bichler J, Wells-Knecht KJ, Thorpe SR, and Baynes JW (1995). N epsilon-(carboxymethyl)lysine is a dominant advanced glycation end product (AGE) antigen in tissue proteins. Biochemistry 34: 10872–10878.
Sakata N, Imanaga Y, Meng J, Tachikawa Y, Takebayashi S, Nagai R, Horiuchi S, Itabe H, and Takano T (1998). Immunohistochemical localization of different epitopes of advanced glycation end products in human atherosclerotic lesions. Atherosclerosis 141: 61–75.
Sasaki N, Fukatsu R, Tsuzuki K, Hayashi Y, Yoshida T, Fujii N, Koike T, Wakayama I, Yanagihara R, Garruto R, Amano N, and Makita Z (1998). Advanced glycation end products in Alzheimer’s disease and other neurodegenerative diseases. Am J Pathol 153: 1149–1155.
Sell DR and Monnier VM (1989). Structure elucidation of a senescence cross-link from human extracellular matrix. J Biol Chem 264: 21597–21602.
Shi SR, Cote RJ, and Taylor CR (1997). Antigen retrieval immunohistochemistry: Past, present, and future. J Histochem Cytochem 45: 327–343.
Shi SR, Key ME, and Kalra KL (1991). Antigen retrieval in formalin-fixed, paraffin-embedded tissues: an enhancement method for immunohistochemical staining based on microwave oven heating of tissue sections. J Histochem Cytochem 39: 741–748.
Shimokawa I, Higami Y, Horiuchi S, Iwasaki M, and Ikeda T (1998). Advanced glycosylation end products in adrenal lipofuscin. J Gerontol 53: B49–51.
Smith MA, Kutty RK, Richey PL, Yan SD, Stern D, Chader GJ, Wiggert B, Petersen RB, and Perry G (1994a). Heme oxygenase-1 is associated with the neurofibrillary pathology of Alzheimer’s disease. Am J Pathol 145: 42–47.
Smith MA, Taneda S, Richey PL, Miyata S, Yan S-D, Stern D, Sayre LM, Monnier VM, and Perry G (1994b). Advance Maillard reaction end products are associated with Alzheimer disease pathology. Proc Natl Acad Sci USA 91: 5710–5714.
Smith PK, Krohn RI, Hermanson GT, Mallia AK, Gartner FH, Provenzano MD, Fujimoto EK, Goeke NM, Olson BJ, and Klenk DC (1985). Measurement of protein using bicinchoninic acid. Anal Biochem 150: 76–85.
Sugimoto K, Nishizawa Y, Horiuchi S, and Yagihashi S (1997). Localization in human diabetic peripheral nerve of N(epsilon)-carboxymethyllysine-protein adducts, an advanced glycation endproduct. Diabetologia 40: 1380–1387.
Suzuki D, Yagame M, Naka R, Jinde K, Endoh M, Nomoto Y, Sakai H, Araki N, and Horiuchi S (1995). Immunohistochemical staining of renal biopsy samples in patients with diabetic nephropathy in non-insulin dependent diabetes mellitus using monoclonal antibody to advanced glycation end products. Nephrology 1: 199–205.
Takeda A, Wakai M, Niwa H, Dei R, Yamamoto M, Li M, Goto Y, Yasuda T, Nakagomi Y, Watanabe M, Inagaki T, Yasuda Y, Miyata T, and Sobue G (2001). Neuronal and glial advanced glycation end product [Nepsilon-(carboxymethyl)lysine]] in Alzheimer’s disease brains. Acta Neuropathol (Berl) 101: 27–35.
Taylor CR, Shi SR, Chen C, Young L, Yang C, and Cote RJ (1996). Comparative study of antigen retrieval heating methods: Microwave, microwave and pressure cooker, autoclave, and steamer. Biotech Histochem 71: 263–270.
Thornalley PJ (1996). Pharmacology of methylglyoxal: Formation, modification of proteins and nucleic acids, and enzymatic detoxification—A role in pathogenesis and antiproliferative chemotherapy. Gen Pharmacol 27: 565–573.
Thornalley PJ, Langborg A, and Minhas HS (1999). Formation of glyoxal, methylglyoxal and 3-deoxyglucosone in the glycation of proteins by glucose. Biochem J 344: 109–116.
Thornalley PJ, Yurek-George A, and Argirov OK (2000). Kinetics and mechanism of the reaction of aminoguanidine with the alpha-oxoaldehydes glyoxal, methylglyoxal, and 3-deoxyglucosone under physiological conditions. Biochem Pharmacol 60: 55–65.
Ueda Y, Miyata T, Goffin E, Yoshino A, Inagi R, Ishibashi Y, Izuhara Y, Saito A, Kurokawa K, and Van Ypersele De Strihou C (2000). Effect of dwell time on carbonyl stress using icodextrin and amino acid peritoneal dialysis fluids. Kidney Int 58: 2518–2524.
Vitek MP, Bhattacharya K, Glendening JM, Stopa E, Vlassara H, Bucala R, Manogue K, and Cerami A (1994). Advanced glycation end products contribute to amyloidosis in Alzheimer disease. Proc Natl Acad Sci USA 91: 4766–4770.
Wells-Knecht KJ, Zyzak DV, Litchfield JE, Thorpe SR, and Baynes JW (1995a). Mechanism of autoxidative glycosylation: Identification of glyoxal and arabinose as intermediates in the autoxidative modification of proteins by glucose. Biochemistry 34: 3702–3709.
Wells-Knecht MC, Thorpe SR, and Baynes JW (1995b). Pathways of formation of glycoxidation products during glycation of collagen. Biochemistry 34: 15134–15141.
Whistler RL and Wolfrom ML (1963). In: Method in carbohydrate chemistry, vol 2. Academic Press, New York: 421–423.
Wiechelman KJ, Braun RD, and Fitzpatrick JD (1988). Investigation of the bicinchoninic acid protein assay: identification of the groups responsible for color formation. Anal Biochem 175: 231–237.
Yamada H, Miyata S, Igaki N, Yatabe H, Miyauchi Y, Ohara T, Sakai M, Shoda H, Oimomi M, and Kasuga M (1994a). Increase in 3-deoxyglucosone levels in diabetic rat plasma. Specific in vivo determination of intermediate in advanced Maillard reaction. J Biol Chem 269: 20275–20280.
Yamada K, Miyahara Y, Hamaguchi K, Nakayama M, Nakano H, Nozaki O, Miura Y, Suzuki S, Tuchida H, Mimura N, Araki N, and Horiuchi S (1994b). Immunohistochemical study of human advanced glycosylation end-products (AGE) in chronic renal failure. Clin Nephrol 42: 354–361.
Yan SD, Chen X, Schmidt AM, Brett J, Godman G, Zou YS, Scott CW, Caputo C, Frappier T, Smith MA, Perry G, Yen S, and Stern D (1994). Glycated tau protein in Alzheimer disease: A mechanism for induction of oxidant stress. Proc Natl Acad Sci USA 91: 7787–7791.
Yeboah FK, Alli I, and Yaylayan VA (1999). Reactivities of D-glucose and D-fructose during glycation of bovine serum albumin. J Agric Food Chem 47: 3164–3172.
Yoshida S, Yamada K, Hamaguchi K, Nishimura M, Hatakeyama E, Tsuchida H, Sakamoto K, Kashiwabara H, Yokoyama T, Ikeda K, and Horiuchi S (1998). Immunohistochemical study of human advanced glycation end-products (AGE) and growth factors in cardiac tissues of patients on maintenance dialysis and with kidney transplantation. Clin Nephrol 49: 273–380.
Zyzak DV, Richardson JM, Thorpe SR, and Baynes JW (1995). Formation of reactive intermediates from Amadori compounds under physiological conditions. Arch Biochem Biophys 316: 547–554.
Acknowledgements
This work was supported in part by Grants-in-Aid for Scientific Research (09877200, 09770789, and 09470225 to Seikoh Horiuchi and 12770638 to Ryoji Nagai) from the Ministry of Education, Science, Sports, and Cultures of Japan.
We are grateful to Professor Paul Thornalley and Dr. Naila Ahmed (Department of Biological Sciences, University of Essex, United Kingdom) for their helpful discussion on HPLC analysis of AGE structures. We are also grateful to Dr. Masayoshi Johno, Ms. Chiemi Shiotsu (Department of Dermatology, Kumamoto University), Dr. Ling Xia, Dr. Tadashi Jono, Dr. Hideki Hakamata, Ms. Naoko Nakano, Ms. Kaori Fukuhara, Dr. Akira Miyazaki (Department of Biochemistry, Kumamoto University), and Mr. Yoshito Hamahira for their collaborative endeavors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miki Hayashi, C., Nagai, R., Miyazaki, K. et al. Conversion of Amadori Products of the Maillard Reaction to Nε-(carboxymethyl)lysine by Short-Term Heating: Possible Detection of Artifacts by Immunohistochemistry. Lab Invest 82, 795–808 (2002). https://doi.org/10.1097/01.LAB.0000018826.59648.07
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1097/01.LAB.0000018826.59648.07
This article is cited by
-
The effect of atorvastatin on the concentrations of methylglyoxal, glyoxalase 1, and aldo–keto reductase family 1 member B10 in patients with type 2 diabetes mellitus and prediabetes
International Journal of Diabetes in Developing Countries (2023)
-
The glycation of fibronectin by glycolaldehyde and methylglyoxal as a model for aging in Bruch’s membrane
Amino Acids (2016)
-
Antibody-based detection of advanced glycation end-products: promises vs. limitations
Glycoconjugate Journal (2016)
-
Inhibition of AGEs formation by natural products
Amino Acids (2014)
-
Unexpected Crosslinking and Diglycation as Advanced Glycation End-Products from Glyoxal
Journal of the American Society for Mass Spectrometry (2014)