Abstract
Reperfusion injury is a troublesome and unresolved problem in acute myocardial infarction and is believed to be associated with inflammatory reactions in which various types of cells and cytokines participate, in particular, macrophages and monocyte chemoattractant protein-1 (MCP-1). We designed this study to clarify the role and relationship of macrophages and MCP-1 in ischemic and reperfused heart. The number and distribution of macrophages and MCP-1 messenger RNA (mRNA) in the ischemic and reperfused rat heart were examined with in situ hybridization and immunohistochemistry. Myocardial samples were obtained at several times. In situ hybridization was performed with digoxigenin-labeled antisense RNA probe for rat MCP-1 mRNA, and immunohistochemistry was performed with antimacrophage antibody. Double staining with in situ hybridization and immunohistochemistry was also performed. The number of MCP-1 mRNA-positive cells increased after reperfusion and peaked at 3 hours after reperfusion. Early infiltration of ischemic tissues by macrophages was also observed at the time of the absence of an increase of MCP-1 mRNA-positive cells, and this infiltration was not significantly accelerated by reperfusion, but by ischemia itself. The numbers of both MCP-1 mRNA-positive cells and macrophages increased in the ischemic marginal region over time. From the result of double staining, and based on the cellular morphology and the distribution, the majority of MCP-1 mRNA-positive cells appeared to be activated macrophages. This suggests that macrophages may not be attracted to cardiac tissue only by MCP-1 and that MCP-1 may have some roles other than attracting macrophages into ischemic heart. It also suggests that macrophages and MCP-1 may play an important role in reperfusion injury and that MCP-1 may be one of the key molecules of reperfusion injury. These observations may contribute to the development of a new therapeutic approach to the prevention of reperfusion injury.
Similar content being viewed by others
Introduction
Myocardial damage caused by reperfusion in acute myocardial infarction (AMI) has been a troublesome problem, particularly in the past two decades. In 1977, Gruentzig introduced the clinical use of percutaneous transluminal coronary angioplasty, and now, early myocardial reperfusion by various interventions limits the death rate of patients who sustain a myocardial infarction, particularly when performed during its acute phase. However, this life-saving therapeutic approach remains burdened by the phenomenon of reperfusion injury.
Myocardial ischemia and reperfusion injury are believed to be associated with inflammatory reactions involving various types of cells and cytokines (Entman and Smith, 1994; Fishbein et al, 1978). These cells and cytokines probably have an effect on their own numbers, distributions, and activities during the evolution of AMI. Therefore, it has been difficult to clarify the interactions among them and their respective roles. As a result, no effective measure has thus far been developed to prevent reperfusion injury. On the other hand, it has recently been reported that the administration of estrogen lowered myocardial necrosis and myeloperoxidase activity by inhibiting the production of tumor necrosis factor α by macrophages in a rat model of myocardial ischemia and reperfusion (Squadrito et al, 1997).
The importance of macrophages in myocardial ischemic injury has been demonstrated, and the relationships among macrophages and various molecules, such as nitric oxide and osteopontin, have been recently reported (Murry et al, 1994; Suzuki et al, 1996). The recruitment of macrophages is believed to be accelerated by monocyte chemotactic and activating factor (MCAF)/monocyte chemoattractant protein-1 (MCP-1), and plasma concentrations of MCAF/MCP-1 are known to be increased in patients with AMI (Matsumori et al, 1997).
However, it has recently been reported that macrophages are not attracted simply by MCAF/MCP-1, but they are also attracted by various immunological agents, for example, complements (Birdsall et al, 1997). Also, we think that the roles and relationship of macrophages and MCAF/MCP-1 are not clear enough in cardiac ischemia and reperfusion and that it is necessary for new therapeutic approach to clarify them. For these reasons we designed this study in the ischemic and reperfused rat myocardium.
Results
In Situ Hybridization
MCP-1 mRNA-positive cells were rare (5.7 ± 2.4 cells/mm2; n = 3) in the rat hearts at 1 hour after myocardial ischemia without reperfusion (Fig. 1A and Fig. 2), and they did not increase significantly (16.6 ± 7.1 cells/mm2; n = 3) in the hearts at 2 hours after ischemia without reperfusion (Fig. 1B and Fig. 2). In contrast, the number of positive cells in the hearts at 1 hour after reperfusion (73.6 ± 16.7 cells/mm2; n = 5) (Fig. 1C) was significantly greater than in the hearts at 2 hours after ischemia without reperfusion (p = 0.0472) (Fig. 2). Furthermore, the number of positive cells in the hearts at 3 hours after reperfusion (136.4 ± 10.9 cells/mm2; n = 5) (Fig. 1D) was significantly greater than in the hearts at 1 hour after reperfusion (p = 0.0137) (Fig. 3).
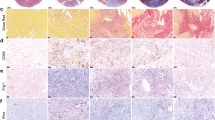
In situ hybridization with digoxigenin (DIG)-labeled antisense RNA probe of rat monocyte chemoattractant protein 1 (MCP-1) mRNA. Positive cells (arrows) are rare in the hearts at 1 hour (A) and 2 hours (B) after ischemia without reperfusion. Positive cells (arrows) are increased in the hearts at 1 hour (C), 3 hours (D), and 6 hours (E) after reperfusion. Ischemic regions and nonischemic regions are the left and the right sides, respectively, on photomicrographs D and E. Positive cells tend to be gradually redistributed in the marginal ischemic region. Most of positive cells (arrow) are suggested to be macrophages morphologically (F). (A, B, C, D, and E; Bar = 20μm) (F; Bar = 5μm)
Mean numbers of MCP-1 mRNA positive cells in the hearts at 1 hour after ischemia without reperfusion (IWR), 2 hours after IWR, and 1 hour after reperfusion (R). The increase in number of positive cells is significantly accelerated after R. *p < 0.05 vs 1 hour after IWR. #p < 0.05 vs 2 hours after IWR.
The number of positive cells in the hearts at 6 hours after reperfusion (130.9 ± 16.3 cells/mm2; n = 5) (Fig. 1E) was not significantly different from their number in the hearts at 3 hours after reperfusion (Fig. 3). Over time, the number of positive cells decreased in the central ischemic region and increased in the border zone (Fig. 4). Based on the cellular morphology and distribution, the majority of MCP-1 mRNA-positive cells appeared to be macrophages (Fig. 1, A–F).
Immunohistochemistry
Few macrophages (1.0 ± 0.5 cells/mm2; n = 2) were detected in sham-operated rat hearts, either with anti-activated-macrophage antibody Ki-M2R or with antimonocyte/dendritic cell/macrophage antibody ED1 (Fig. 5). Activated macrophages were detected in the hearts as early as at 1 hour after ischemia without reperfusion (Fig. 6A), and the number of macrophages at 1 hour after ischemia (103.3 ± 29.3 cells/mm2; n = 5) was significantly greater than the number in sham-operated hearts (p < 0.01) (Fig. 5). The mean numbers of activated macrophages in the hearts at 1 hour after ischemia without reperfusion, at 2 hours after ischemia without reperfusion, at 1 hour after reperfusion, at 3 hours after reperfusion, and at 6 hours after reperfusion were 103.3 ± 29.3, 135.3 ± 31.9, 156.8 ± 35.4, 131.2 ± 12.6, and 134.8 ± 13.1 cells/mm2, respectively (n = 5 each). These differences were not statistically significant (Fig. 5; Fig. 6, A–E; and Fig. 7), and, accordingly, the peak of the infiltration of macrophages was suggested to be earlier than at 1 hour after ischemia.
Mean numbers of activated macrophages in the hearts at 1 hour after ischemia without reperfusion (IWR), 2 hours after IWR, and 1 hour after reperfusion (R), and in sham-operated hearts (Sham). Activated macrophages are already significantly increased at 1 hour after IWR, and the number of activated macrophages have not significantly increased after R. The number of detected cells in Sham was almost the same, either with Ki-M2R, anti-activated macrophages antibody or with ED1, antimonocyte/macrophage/dendritic cell antibody. *p < 0.01 vs Sham.
Immunohistochemistry with Ki-M2R as anti-activated macrophage antibody and with MCA149A as antigranulocyte antibody. Abundant macrophages (arrow) are already visible in the ischemic hearts at 1 hour after ischemia without reperfusion (A). Macrophages (arrows) have not significantly increased in the hearts, either at 2 hours after ischemia without reperfusion (B), 1 hour after reperfusion (C), 3 hours after reperfusion (D), or 6 hours after reperfusion (E). A similar tendency of MCP-1 mRNA-positive cells toward gradual redistribution to the marginal ischemic region is apparent about activated macrophages. Abundant granulocytes (arrow) are also present at 1 hour after ischemia without reperfusion (F). (A, B, C, D, E, and F; Bar = 20μm)
These activated macrophages were widely distributed between the central and marginal regions of ischemia, and over time, the number of macrophages tended to be lower in the central region than in the marginal region, although the difference was not statistically significant (Fig. 8).
In addition, many granulocytes were detected in the hearts as early as at 1 hour after reperfusion (Fig. 6F). However, neither T helper nor T cytotoxic/suppressor cells were found in the hearts at 1 or 3 hours after reperfusion (not shown).
Double Staining
We counted the number of activated macrophages detected with Ki-M2R, the anti-activated-macrophage antibody, among each 100 MCP-1 mRNA-positive cells selected at random in the double-stained cardiac tissues at 3 hours after reperfusion (n = 3). The resulting data showed that the majority (68.7%) of MCP-1 mRNA-positive cells were activated macrophages in the hearts at 3 hours after reperfusion (Fig. 9, A and B; Table 1).
Double staining with in situ hybridization with DIG-labeled antisense RNA probe of rat MCP-1 mRNA and immunohistochemistry with Ki-M2R as anti-activated macrophage antibody in the hearts at 3 hours after reperfusion. Staining with in situ hybridization is recognized inside the cell (violet; arrow) and staining with immunohistochemistry is recognized on the surface of the cell (brown; arrowhead) (A and B). It is clear that activated macrophages produce MCP-1 mRNA. (A; Bar = 5μm)(B; Bar = 2μm)
Discussion
Reperfusion injury is an important clinical problem that remains unresolved, despite the success of various early reperfusion methods in decreasing direct ischemic injury and in improving the survival rate of patients with AMI.
Histopathologically, it has been shown that neutrophils first penetrate the infarcted myocardium, followed by macrophages, and it has been reported that neutrophils are associated with reperfusion injury, in concert with the induction of intracellular adhesion molecule-1 (ICAM-1), interleukin (IL)-6, or IL-8 (Hawkins et al, 1996; Kukielka et al, 1993, 1995a, 1995b; Neumann et al, 1995; Youker et al, 1994). It has also been reported that reperfusion is associated with an increase in the number of macrophages compared with the nonreperfused myocardium (Morita et al, 1993). In the present study, however, macrophages, like neutrophils, were already present in the early stages of ischemia, and their number was not significantly increased by reperfusion. The majority of these macrophages were suggested to be not resident, but newly recruited, because few macrophages were detected in sham-operated hearts, either with anti-activated-macrophage antibody Ki-M2R or with antimonocyte/dendritic cell/macrophage antibody ED1. Surely, it has recently been reported that macrophages are resident in normal heart, but the number of resident macrophages is less than 10 per square millimeter (Frangogiannis et al, 1999; Keller et al, 1988), and this is not so different from sham-operated rat heart in the present study.
MCP-1, one of the C-C chemokines of the superfamily of chemokines, is associated with the recruitment of macrophages. It is produced in nearly all types of cells, including macrophages, and is induced by such inflammatory cytokines as IL-1, tumor necrosis factor-α, and others (Liebler et al, 1994; Takahashi et al, 1995; Weyrich et al, 1995). Furthermore, MCP-1 does not only recruit macrophages, but also stimulates them to induce the release of lysozomal enzymes and the production of active oxygen (Furie and Randolph, 1995), and it is a major attractant of human T lymphocytes (Loetscher et al, 1994). Its association with macrophages in myocardial ischemia and reperfusion, however, remains unclear.
(Kumar et al 1997) have reported that no significant MCP-1 induction was observed in the absence of reperfusion in a dog model of ischemia and reperfusion. (Birdsall et al 1997) have reported that complement C5a, transforming growth factor-β, and MCP-1, in sequence, recruit monocytes into ischemic myocardium within 1 to 5 hours after reperfusion in a dog model. In the present study, a significant acceleration of the production of MCP-1 mRNA by reperfusion was also observed. These observations suggest that MCP-1 controls the influence of macrophages and other cells on cardiac tissue after reperfusion and that it may represent one of the key molecules in reperfusion injury. Furthermore, in the present study, the early infiltration of ischemic tissue by macrophages at the time of the absence of an increase of MCP-1 mRNA-positive cells strongly suggests that MCP-1 participates in reperfusion injury, not by recruiting macrophages, but by activating macrophages themselves or by affecting other cells, including T lymphocytes.
(Kumar et al 1997) have also described the production of MCP-1 by the endothelium of the small veins in a dog model of ischemia and reperfusion. However, in the present rat model of ischemia and reperfusion, we found that the majority, more than two-thirds, of MCP-1 mRNA positive cells were newly recruited and activated macrophages. This suggests that macrophages may affect themselves, each other, or other cells by the production of MCP-1 at least, within a few hours of reperfusion in rat heart. Moreover, the fact that the number of activated macrophages was increased either with reperfusion or without reperfusion and that the production of MCP-1 mRNA was accelerated only by reperfusion suggests that MCP-1 may be more closely concerned with reperfusion injury than macrophages themselves. Accordingly, the ability to control the activity of macrophages or other cells by modulating the production or inhibiting the action of MCP-1 may lead to the design of new therapies to prevent reperfusion injury.
Moreover, we believe that such therapy would be clinically applicable, since the production of MCP-1, later than the production of MCP-1 mRNA, was low within the first few hours of ischemia without reperfusion and was significantly increased by reperfusion. This would allow the delivery, in a timely fashion, of therapy to prevent reperfusion injury, including reperfusion achieved by various methods in the hospital. Our earlier observations, in a rat model of ischemia and reperfusion, of a decrease in infarct size and increase in survival rate by the administration of anti-MCP-1 antibodies just before reperfusion (Ono et al, 1999) are in support of this hypothesis.
In addition, (Okada et al 1998) have reported that MCP-1 is up-regulated by cyclic stretch in human endothelial cells, and (Furukawa et al 1999) have reported that anti-MCP-1 treatment reduces neointimal hyperplasia in early neointimal lesion formation at balloon injury of rat carotid artery. Accordingly, modulating the production or inhibiting the action of MCP-1 may also lead to the prevention of balloon injury and restenosis, and this may truly be a case of killing two birds with one stone in intervention by catheter for AMI.
Materials and Methods
Ischemia-Reperfusion Model
The experiments were performed in 10-week-old male Wistar rats. The animals were anesthetized with sodium pentobarbital (50 mg/kg, ip) and ventilated by respirator with pure oxygen after tracheotomy. A midline thoracotomy was performed to gain access to the heart and mediastinum, and the left anterior descending artery was occluded with a 5–0 silk ligature. Ischemia was directly confirmed by visible discoloration and maintained for 1 hour. Reperfusion was achieved by releasing the ligature. Five rats each were killed at 1 hour, 3 hours, and 6 hours, respectively, after reperfusion. For comparison, three rats each were killed after 1 hour and 2 hours, respectively, of coronary occlusion not followed by reperfusion, and, as sham operation, two rats were killed without occlusion of the left anterior descending artery.
Histologic Study
The rat hearts were removed and divided into two sections in a plane perpendicular to the left ventricular long axis. The hearts were covered with OCT compound, frozen with acetone and dry ice, and stored at −80° C. Slices of cardiac tissue (6 μm thick) were made with cryostat for histopathological examination.
In Situ Hybridization
The cDNAs of rat MCAF/MCP-1 mRNA were ligated to plasmid vectors (pCR-Script; Stratagene, La Jolla, California), and the vectors were transformed and subcloned to competent cells (JM109; Toyobo Engineering, Osaka, Japan). Subcloned vectors were collected with QIAGEN′s (Valencia, California) plasmid midi protocol and linearized with restriction enzyme (Hind III or Eco RI). The linearized plasmid vectors containing cDNA of rat MCAF/MCP-1 were used as templates of in vitro transcription with RNA polymerase (T3 or T7) and digoxigenin (DIG)-labeled uridine-triphosphate, and antisense or sense RNA probes labeled with DIG were synthesized. A DIG RNA Labeling Kit (Boehringer, Mannheim, Germany) was primarily used in this process.
Samples of cardiac tissue on slides were fixed in 4% paraformaldehyde and predigested with proteinase K at 37° C for 30 minutes. The samples were fixed again in 4% paraformaldehyde and dehydrated with ethanol. Next, they were incubated at 50° C for 16 hours with DIG-labeled RNA probes (antisense or sense) for in situ hybridization with MCAF/MCP-1 messenger RNA (mRNA). After the remainder of the probes were washed and removed in 2 × sodium chloride-sodium citrate (SSC) mixed with formamide, the samples were incubated at 4° C for 12 hours with the anti-DIG antibodies conjugate with alkaline phosphatase. After washing and removing the remainder of the antibodies in 100 mm Tris-Hcl, pH 7.5, and 150 mm NaCl, the samples were reacted for approximately 3 hours with nitroblue tetrazolium salt and 5-bromo-4-chloro-3-indolyl phosphate (NBT-BCIP), as a substrate of alkaline phosphatase, for color reaction and detection. The samples were then enclosed with water-soluble sealing compound for microscopic examination. A DIG Nucleic Acid Detection Kit (Boehringer) was primarily used in this process.
Immunohistochemistry
Cardiac tissues were fixed in 4% paraformaldehyde, blocked with normal serum of rabbit, and incubated at room temperature for 30 minutes with Ki-M2R antibodies (BMA, Augst, Switzerland) made of mouse IgG, which are monoclonal and specific against rat-activated macrophages and negative for monocytes or dendritic cells (Wacker et al, 1985). After the remainder of the antibodies were washed and removed in PBS, the samples were incubated at 4° C for 12 hours with biotinylated antibodies specific against mouse IgG from rabbit (DAKO, Glostrup, Denmark). After having removed and washed the remainder of the biotinylated antibodies in PBS, the samples were incubated with avidin-biotin-horseradish peroxidase complex (Vector Laboratories, Burlingame, California), at room temperature for 30 minutes. After the remainder of the avidin-biotin-horseradish peroxidase complex had been removed and washed in PBS, the samples were reacted with 3,3′-diaminobenzidine for coloring reaction and detection. Next, the samples were counter-stained with methylgreen, dehydrated with ethanol, and penetrated with xylene. The samples were then enclosed in an oil-soluble sealing compound for microscopic examination.
Antirat granulocyte antibody MCA149A (Serotec, Oxford, England), antirat T helper cell antibody CL003A (Cedarlane, Ontario, Canada), and antirat T cytotoxic/suppressor cell antibody CL004A (Cedarlane, Ontario, Canada) were used as above for immunohistochemical study. Likewise, antimonocyte/dendritic cell/macrophage antibody ED1 (BMA, Augst, Switzerland) was used in sham-operated rat hearts as above for immunohistochemical study.
Double Staining
After staining the samples of cardiac tissue with in situ hybridization as above, they were stained with Ki-M2R anti-activated-macrophage antibody, used in immunohistochemistry, in a similar fashion.
Statistical Analysis
Values are expressed as mean ± sem, and significance was established by one-way analysis of variance (ANOVA), with multiple comparisons by Fisher’s protected least significance difference. In all analyses, statistical significance was declared at a 95% confidence level.
References
Birdsall HH, Green DM, Trial J, Youker KA, Burns AR, MacKay CR, LaRosa GJ, Hawkins HK, Smith CW, Michael LH, Entman ML, and Rossen RD (1997). Complement C5a, TGF-β1, and MCP-1, in sequence, induce migration of monocytes into ischemic canine myocardium within the first one to five hours after reperfusion. Circulation 95:684–692.
Entman ML and Smith CW (1994). Postreperfusion inflammation: A model for reaction to injury in cardiovascular disease. Cardiovasc Res 28:1301–1311.
Fishbein MC, Maclean D, and Maroko PR (1978). The histopathologic evolution of myocardial infarction. Chest 73:843–849.
Frangogiannis NG, Burns AR, Michael LH, and Entman ML (1999). Histochemical and morphological characteristics of canine cardiac mast cells. Histochem J 31:221–229.
Furie MB and Randolph GJ (1995). Chemokines and tissue injury. Am J Pathol 146:1287–1301.
Furukawa Y, Matsumori A, Ohashi N, Shioi T, Ono K, Harada A, Matsushima K, and Sasayama S (1999). Anti-monocyte chemoattractant protein-1/monocyte chemotactic and activating factor antibody inhibits neointimal hyperplasia in injured rat carotid arteries. Circ Res 84:306–314.
Hawkins HK, Entman ML, Zhu JY, Youker KA, Berens K, Dore M, and Smith CW (1996). Acute inflammatory reaction after myocardial ischemic injury and reperfusion: Development and use of a neutrophil-specific antibody. Am J Pathol 148:1957–1969.
Keller AM, Clancy RM, Barr ML, Marboe CC, and Cannon PJ (1988). Acute reoxygenation injury in the isolated rat heart: Role of resident cardiac mast cells. Circ Res 63:1044–1052.
Kukielka GL, Hawkins HK, Michael L, Manning AM, Youker K, Lane C, Entman ML, Smith CW, and Anderson DC (1993). Regulation of intercellular adhesion molecule-1 (ICAM-1) in ischemic and reperfused canine myocardium. J Clin Invest 92:1504–1516.
Kukielka GL, Smith CW, LaRosa GJ, Manning AM, Mendoza LH, Daly TJ, Hughes BJ, Youker KA, Hawkins HK, Michael LH, Rot A, and Entman ML (1995a). Interleukin-8 gene induction in the myocardium after ischemia and reperfusion in vivo. J Clin Invest 95:89–103.
Kukielka GL, Smith CW, Manning AM, Youker KA, Michael LH, and Entman ML (1995b). Induction of interleukin-6 synthesis in the myocardium: Potential role in postreperfusion inflammatory injury. Circulation 92:1866–1875.
Kumar AG, Ballantyne CM, Michael LH, Kukielka GL, Youker KA, Lindsey ML, Hawkins HK, Birdsall HH, MacKay CR, LaRosa GJ, Rossen RD, Smith CW, and Entman ML (1997). Induction of monocyte chemoattractant protein-1 in the small veins of the ischemic and reperfused canine myocardium. Circulation 95:693–700.
Liebler JM, Kunkel SL, Burdick MD, Standiford TJ, Rolfe MW, and Strieter RM (1994). Production of IL-8 and monocyte chemotactic peptide-1 by peripheral blood monocytes: Disparate responses to phytohemagglutinin and lipopolysaccharide. J Immunol 152:241–249.
Loetscher P, Seitz M, Clark-Lewis I, Baggiolini M, and Moser B (1994). Monocyte chemotactic proteins MCP-1, MCP-2, and MCP-3 are major attractants for human CD4+ and CD8+ T lymphocytes. Faseb J 8:1055–1060.
Matsumori A, Furukawa Y, Hashimoto T, Yoshida A, Ono K, Shioi T, Okada M, Iwasaki A, Nishio R, Matsushima K, and Sasayama S (1997). Plasma levels of the monocyte chemotactic and activating factor/monocyte chemoattractant protein-1 are elevated in patients with acute myocardial infarction. J Mol Cell Cardiol 29:419–423.
Morita M, Kawashima S, Ueno M, Kubota A, and Iwasaki T (1993). Effects of late reperfusion on infarct expansion and infarct healing in conscious rats. Am J Pathol 143:419–430.
Murry CE, Giachelli CM, Schwartz SM, and Vracko R (1994). Macrophages express osteopontin during repair of myocardial necrosis. Am J Pathol 145:1450–1462.
Neumann FJ, Ott I, Gawaz M, Richardt G, Holzapfel H, Jochum M, and Schoemig A (1995). Cardiac release of cytokines and inflammatory responses in acute myocardial infarction. Circulation 92:748–755.
Okada M, Matsumori A, Ono K, Furukawa Y, Shioi T, Iwasaki A, Matsushima K, and Sasayama S (1998). Cyclic stretch upregulates production of interleukin-8 and monocyte chemotactic and activating factor/monocyte chemoattractant protein-1 in human endothelial cells. Arterioscler Thromb Vasc Biol 18:894–901.
Ono K, Matsumori A, Furukawa Y, Igata H, Shioi T, Matsushima K, and Sasayama S (1999). Prevention of myocardial reperfusion injury in rats by an antibody against monocyte chemotactic and activating factor/monocyte chemoattractant protein-1. Lab Invest 79:195–203.
Squadrito F, Altavilla D, Squadrito G, Campo GM, Arlotta M, Arcoraci V, Minutoli L, Serrano M, Saitta A, and Caputi AP (1997). 17β-oestradiol reduces cardiac leukocyte accumulation in myocardial ischaemia reperfusion injury in rat. Eur J Pharmacol 335:185–192.
Suzuki H, Wildhirt SM, Dudek RR, Narayan KS, Bailey AH, and Bing RJ (1996). Induction of apoptosis in myocardial infarction and its possible relationship to nitric oxide synthase in macrophages. Tissue Cell 28:89–97.
Takahashi M, Masuyama J, Ikeda U, Kasahara T, Kitagawa S, Takahashi Y, Shimada K, and Kano S (1995). Induction of monocyte chemoattractant protein-1 synthesis in human monocytes during transendothelial migration in vitro. Circ Res 76:750–757.
Wacker HH, Radzum HJ, and Parwaresch MR (1985). Ki-M2R, a new specific monoclonal antibody, discriminates tissue macrophages from reticulum cells and monocytes in vivo and in vitro. J Leukoc Biol 38:509–520.
Weyrich AS, Mclntyre TM, McEver RP, Prescott SM, and Zimmerman GA (1995). Monocyte tethering by P-selectin regulates monocyte chemotactic protein-1 and tumor necrosis factor-α secretion: Signal integration and NF-kappaB translocation. J Clin Invest 95:2297–2303.
Youker KA, Hawkins HK, Kukielka GL, Perrard JL, Michael LH, Ballantyne CM, Smith CW, and Entman ML (1994). Molecular evidence for induction of intracellular adhesion molecule-1 in the viable border zone associated with ischemia-reperfusion injury of the dog heart. Circulation 89:2736–2746.
Acknowledgements
We would like to thank Dr. Shintaro Nomura (Department of Pathology, University of Osaka, Osaka, Japan) who taught us the technique of nonisotopic in situ hybridization.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported in part by a research grant from the Ministry of Health and Welfare of Japan and a grant-in-aid for general scientific research from the Ministry of Education, Science, and Culture of Japan.
Rights and permissions
About this article
Cite this article
Kakio, T., Matsumori, A., Ono, K. et al. Roles and Relationship of Macrophages and Monocyte Chemotactic and Activating Factor/Monocyte Chemoattractant Protein-1 in the Ischemic and Reperfused Rat Heart. Lab Invest 80, 1127–1136 (2000). https://doi.org/10.1038/labinvest.3780119
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.3780119
This article is cited by
-
The Dynamic Role of Cardiac Macrophages in Aging and Disease
Current Cardiology Reports (2022)
-
Visualization of elastin using cardiac magnetic resonance imaging after myocardial infarction as inflammatory response
Scientific Reports (2021)
-
Chemokines in Myocardial Infarction
Journal of Cardiovascular Translational Research (2021)
-
Significant association between admission serum monocyte chemoattractant protein-1 and early changes in myocardial function in patients with first ST-segment elevation myocardial infarction after primary percutaneous coronary intervention
BMC Cardiovascular Disorders (2019)
-
The Effects of Periostin in a Rat Model of Isoproterenol: Mediated Cardiotoxicity
Cardiovascular Toxicology (2018)