Abstract
Histamine regulates many functions by binding to four histamine G-coupled receptor proteins (H1R, H2R, H3R and H4R). As H3R exerts their effects by coupling to Gαi/o proteins reducing adenosine 3′, 5′-monophosphate (cAMP) levels (a key player in the modulation of cholangiocyte hyperplasia/damage), we evaluated the role of H3R in the regulation of biliary growth. We posed the following questions: (1) Do cholangiocytes express H3R? (2) Does in vivo administration of (R)-(α)-(−)-methylhistamine dihydrobromide (RAMH) (H3R agonist), thioperamide maleate (H3R antagonist) or histamine, in the absence/presence of thioperamide maleate, to bile duct ligated (BDL) rats regulate cholangiocyte proliferation? and (3) Does RAMH inhibit cholangiocyte proliferation by downregulation of cAMP-dependent phosphorylation of protein kinase A (PKA)/extracellular signal-regulated kinase 1/2 (ERK1/2)/ets-like gene-1 (Elk-1)? The expression of H3R was evaluated in liver sections by immunohistochemistry and immunofluorescence, and by real-time PCR in cholangiocyte RNA from normal and BDL rats. BDL rats (immediately after BDL) were treated daily with RAMH, thioperamide maleate or histamine in the absence/presence of thioperamide maleate for 1 week. Following in vivo treatment of BDL rats with RAMH for 1 week, and in vitro stimulation of BDL cholangiocytes with RAMH, we evaluated cholangiocyte proliferation, cAMP levels and PKA, ERK1/2 and Elk-1 phosphorylation. Cholangiocytes from normal and BDL rats express H3R. The expression of H3R mRNA increased in BDL compared to normal cholangiocytes. Histamine decreased cholangiocyte growth of BDL rats to a lower extent than that observed in BDL RAMH-treated rats; histamine-induced inhibition of cholangiocyte growth was partly blocked by thioperamide maleate. In BDL rats treated with thioperamide maleate, cholangiocyte hyperplasia was slightly higher than that of BDL rats. In vitro, RAMH inhibited the proliferation of BDL cholangiocytes. RAMH inhibition of cholangiocyte growth was associated with decreased cAMP levels and PKA/ERK1/2/Elk-1 phosphorylation. Downregulation of cAMP-dependent PKA/ERK1/2/Elk-1 phosphorylation (by activation of H3R) is important in the inhibition of cholangiocyte growth in liver diseases.
Similar content being viewed by others
Main
Cholangiocytes, which are normally mitotically dormant, proliferate in a number of experimental models of cholestasis including bile duct ligation (BDL).1, 2, 3, 4 Cholangiocyte proliferation is regulated by a number of factors including cyclic adenosine 3′,5′-monophosphate (cAMP),1, 2, 3, 5 gastrointestinal hormones (eg, gastrin and somatostatin),1, 2, 6, 7 bile salts,2, 8 cholinergic, adrenergic and serotoninergic neurotransmitters,1, 2, 9 and vascular growth factors.1, 2, 10 Among these regulators of cholangiocyte proliferation, basal and agonist-induced changes in cAMP levels play a key role in the regulation of cholangiocyte growth/loss.2, 3, 5 Although increased cAMP levels sustain cholangiocyte proliferation, decreased cAMP formation results in a reduction of cholangiocyte hyperplasia.2, 3, 5
The aminergic peptide histamine is responsible for many functions in the body such as neurogenic functions, inflammatory responses, allergic responses and gastric secretion.11, 12, 13 Four G-protein coupled histamine receptors (HRs) (H1R, H2R, H3R and H4R) exist.14, 15 Although H1R act via Gαq mobilizing [Ca2+]i,16 the activation of H2R is modulated by Gαs proteins, coupled to adenylyl cyclase.17 H3R were first noted as presynaptic autoreceptors on brain histamine neurons, although they were also found in other cells.18, 19 Cloning and functional characterization of the human and rat H3R cDNA show that this receptor belongs to the family of G-protein-coupled receptors.20, 21 These early studies demonstrated that H3R agonists decrease forskolin-dependent cAMP accumulation.21 Recently, H4R were cloned.22 This receptor is over 35% homologous to the H3R and appears to have similar functions, such as its ability to inhibit forskolin-stimulated cAMP levels (although not as potently as the H3R) in bone marrow cells.22
The rationale for studying the role of H3R in the regulation of cholangiocyte growth in BDL rats is first based on the fact that H3R exerts their effects by coupling to Gαi/o proteins with inhibition of adenylyl cyclase,21, 22 a key factor in the regulation of cholangiocyte growth.1, 2, 3, 5 The aims of our study were to: (i) evaluate the presence of H3R protein in bile ducts from normal and BDL rat liver sections; (ii) study the expression of H3R mRNA in purified cholangiocytes from normal and BDL rats; (iii) determine the in vivo effect of (a) the H3R agonist, (R)-(α)-(−)-methylhistamine dihydrobromide (RAMH),23, 24 (b) the H3 HR antagonist, thioperamide maleate25, 26 and (c) histamine, in the absence or presence of thioperamide maleate, on cholangiocyte proliferation in BDL rats; and (iv) to elucidate, in purified BDL cholangiocytes, the transduction mechanisms by which RAMH regulates the proliferation of these cells.
Materials and methods
Materials
All reagents were purchased from Sigma Chemical Co. (St Louis, MO, USA) unless stated otherwise. Antibodies were obtained from Santa Cruz Biotechnology (Santa Cruz, CA, USA). The substrate for γ-glutamyltranspeptidase (γ-GT), N(γ-L-glutamyl)-4-methoxy-2-naphthylamide was purchased from Polysciences (Warrington, PA, USA). Primers for the determination of H3R mRNA in purified cholangiocytes by real-time PCR were obtained from SuperArray (Frederick, MD, USA). RIA kits for the determination of intracellular cAMP and D-myo-inositol 1,4,5,trisphosphate (IP3) levels were purchased from Amersham (Arlington Heights, IL, USA). The histamine EIA kits (used for measuring histamine levels in normal and BDL serum) were obtained from Cayman Chemical (Ann Arbor, MI, USA).
Animal Model
Male Fisher 344 rats (150–175 g) were purchased from Charles River (Wilmington, MA, USA). Animals were kept in a temperature-controlled environment (22°C) with a 12-h light–dark cycle. The studies were conducted in: (i) normal rats treated with NaCl (vehicle) or RAMH (10 mg/kg body weight/day)23, 24 for 1 week; and (ii) BDL rats that, immediately after BDL,27 were treated for 1 week with daily I.P. injections of NaCl, RAMH (10 mg/kg body weight/day),28 thioperamide maleate (5 mg/kg body weight)25, 26 or histamine (0.5 mg/kg body weight)15, 29 in the absence or presence of thioperamide maleate for 1 week. The doses of RAMH, thioperamide maleate and histamine used in the present studies were similar to those used in other studies in rodents.15, 25, 26, 28, 29 Liver blocks, serum and cholangiocytes were obtained at the end of the selected treatments. We evaluated body and liver weight from the selected groups of animals. Before each procedure, animals were anesthetized with sodium pentobarbital (50 mg/kg body weight IP). In vitro studies were performed in purified cholangiocytes from 1-week BDL rats stimulated with 0.2% BSA (basal) or RAMH (10 μM). All animals received humane care according to the criteria outlined in the ‘Guide for the Care and Use of Laboratory Animals’ prepared by the National Academy of Sciences and published by the National Institutes of Health and under local IACUC approval.
Purification of Cholangiocytes
Cholangiocytes were purified by immunoaffinity separation30 utilizing a monoclonal antibody (IgM, kindly provided by Dr R Faris, Brown University, Providence, RI, USA) against an unidentified antigen expressed by all intrahepatic cholangiocytes.30 Cell viability (approximately 97%) was determined by Trypan blue exclusion. Purity (98–99%) of cholangiocytes was assessed by γ-GT histochemistry.31
Expression of H3 Histamine Receptors
Immunohistochemistry for H3R was performed in frozen sections (6 μm thick; n=3 per each group of animals) pretreated with cold acetone for 10 min, followed by endogenous peroxidase quenching for 5 min with methanol-peroxide solution (0.3% hydrogen peroxide solution, Santoku Chemical Industries, Tokyo, Japan) in 80% methanol (WAKO, Osaka, Japan). After washing with cold 1 × phosphate-buffered saline (PBS), sections were incubated with a specific H3R antibody (C20, goat polyclonal, dilution, 1:100) or non-immune serum (negative control) at 4°C overnight. After rinsing with 1 × PBS, Histofine Simple Stain MAX PO (Nichirei, Tokyo, Japan) was added as secondary antibody for 1 h at room temperature. Nuclear counterstaining was performed by hematoxylin for light micrographs after detecting reactions with VECTOR NovaRED (Vector Laboratories, Inc., Burlingame, CA, USA).
Immunofluorescence for H3R in liver sections (20 μm thick; n=3 per each group of animals) from normal and BDL rats was performed as follows. Samples were fixed in 4% paraformaldehyde (in 1 × PBS) for 10 min, followed by tissue permeabilization in PBST (1 × PBS containing 0.2% Triton X-100). Nonspecific protein binding was blocked by 5% normal goat serum. Following incubation with a primary antibody against H3R (raised in goat, 1:5; Santa Cruz Biotechnology, Santa Cruz, CA, USA) or non-immune goat serum (negative control), together with an anticytokeratin-19 (CK-19) antibody (raised in mouse, 1:50; Vision Biosystems Inc., Norwell, MA, USA), samples were rinsed with 1 × PBS and subsequently incubated with Cy2-conjugated anti-mouse and Cy3-conjugated anti-goat antibodies (both diluted at 1:50, Jackson Immunochemicals, West Grove, PA, USA) Following immunohistochemistry or immunofluorescence, samples were observed either with the light microscope ECLIPSE E600 (Nikon, Kawasaki, Japan) or an Olympus IX71 inverted confocal microscope.
For immunofluorescence for H3R in cholangiocyte smears from normal and BDL rats, samples were pretreated with cold acetone for 10 min, followed by blocking of nonspecific protein binding using normal goat serum. Following incubation with the H3R antibody or nonimmune serum (negative control), samples were rinsed with 1 × PBS and subsequently incubated with Alexa 488-conjugated anti-goat antibody (dilution, 1:100, Molecular Probes, Eugene, OR, USA) as secondary antibody for 1 h at room temperature. Following immunohistochemistry or immunofluorescence, samples were observed either with the light microscope ECLIPSE E600 (Nikon, Kawasaki, Japan) or fluorescence microscope DMRXA/HC (LEICA, Tokyo, Japan).
To evaluate the expression of H3R mRNA in total cholangiocyte RNA (0.75 μg) from normal and BDL rats, we employed the RT2 real-time assay from SuperArray (Frederick, MD, USA). RNA was extracted utilizing the RNeasy Mini Kit (Qiagen Inc., Valencia, CA, USA) according to the instructions provided by the vendor. RNA was extracted from normal and BDL cholangiocytes (1 × 105) and reverse transcribed using the Reaction Ready™ First Strand cDNA synthesis kit (SuperArray, Frederick, MD, USA). These reactions were then used as templates for the PCR assays. SYBR Green PCR master mix was utilized in the experimental assay. One microliter of previously prepared template was added to 12.5 μl of master mix, 10.5 μl of DI water and 1 μl of RT2 PCR rat primers (SuperArray, Frederick, MD, USA) designed specifically for the messages for H3R and glyceraldehyde-3-phosphate dehydrogenase (GAPDH), the housekeeping gene.32 The plate was then placed in the real-time thermal cycler (ABI Prism 7900HT sequence detection system) and run on a two-step PCR cycling program for 95°C for 10 min followed by 40 cycles of 95°C for 15 s and 60°C for 1 min. A ΔΔCT analysis was performed using the normal pooled cholangiocytes as the control sample. Data were expressed as relative mRNA levels±s.e.m. of H3R to GAPDH ratio (n=3).
In Vivo Studies
Evaluation of liver, body weight and liver to body weight ratio, necrosis, lobular damage, and histamine, transaminase and bilirubin serum levels and cholangiocyte apoptosis
In the selected groups of animals, we evaluated the changes in necrosis, lobular morphology (disarrangement of hepatocytes), histamine, transaminases and bilirubin serum levels, and cholangiocyte apoptosis.
Ten randomly selected portal areas, as well as surrounding lobular areas, were evaluated using light microscopy of hematoxylin and eosin stained sections (5 μm thick, 3 sections evaluated per each group of animal). For quantification of damage, the following categories were applied: 0, null; 1, limited to portal area; 2, intermediate; and 3, pan lobular. Liver sections were examined in a coded fashion by light microscopy with an Olympus BX-40 (Tokyo, Japan) microscope equipped with a camera. Histamine serum levels of normal and BDL rats were evaluated by commercially available EIA kits (Cayman Chemical). To evaluate liver damage, serum samples from BDL rats, treated with NaCl or RAMH for 1 week, were analyzed for transaminases (aspartate transaminase (AST) and alanine transaminase (ALT)) and direct bilirubin. Transaminases and direct bilirubin levels were measured using a Dimension® RxL Max* Integrated Chemistry System (Dade Behring Inc., Deerfield, IL, USA).
We evaluated cholangiocyte apoptosis by terminal deoxynucleotidyl transferase biotin-dUTP nick end labeling (TUNEL) analysis33 in paraffin-embedded liver sections (5 μm, three slides evaluated for each group) from the selected group of animals. Following counterstaining with hematoxylin solution, liver sections were examined by light microscopy with an Olympus BX-40 microscope (Tokyo, Japan) equipped with a camera. Approximately 100 cells per slide were counted in a coded fashion in 10 non-overlapping fields.
Evaluation of cholangiocyte proliferation and cAMP levels
To evaluate the effects of RAMH, thioperamide maleate or histamine (in the absence or presence of thioperamide maleate) on cholangiocyte proliferation, we measured the number of proliferating cellular nuclear antigen (PCNA)- and CK-19-positive cholangiocytes (by immunohistochemistry in paraffin-embedded sections, 5 μm thick, three slides analyzed per animal, n=2 animals)34 and γ-GT-positive ducts (by histochemistry in frozen sections, 5 μm thick, three slides analyzed per animal, n=2 animals)31 in sections from the selected group of animals. Following staining, slides were counterstained with hematoxylin and examined in a coded fashion with an ECLIPSE E6000 microscope (Nikon, Japan). Data were expressed as number of PCNA- or CK-19-positive cholangiocytes per 100 cholangiocytes. For γ-GT staining, data were expressed as % bile duct volume per each portal tract examined (10 randomly selected portal areas were evaluated).
We measured PCNA (an index of cell replication)33 protein expression by immunoblots in protein (10 μg) whole-cell lysate from brain (positive control) or purified cholangiocytes from BDL rats treated with NaCl or RAMH for 1 week. Proteins were visualized using chemiluminescence (ECL Plus kit, Amersham Life Science). Blots were normalized against the housekeeping protein, β-actin.35 The intensity of the bands was determined by scanning video densitometry using the phospho-imager, Storm 860, Amersham Biosciences (Piscataway, NJ, USA) using the ImageQuant TLV 2003.02.
We measured intracellular basal cAMP levels (a key regulatory determinant of cellular proliferation including ductal hyperplasia)5, 36, 37 in purified cholangiocytes from normal or BDL rats, which immediately after BDL, were treated with NaCl- or RAMH for 1 week. After purification, cholangiocytes were incubated for 1 h at 37°C to restore surface proteins damaged by treatment with proteolytic enzymes.38 In each experiment, 0.5 mM 3-isobutylmethylxanthine, a phosphodiesterase inhibitor, was added. Following ethanol extraction, basal cAMP levels were measured by radioimmunoassay using commercial kits (Amersham) according to the instructions supplied by the vendor.
Evaluation of the phosphorylation of the PKA → ERK1/2 → Elk-1 signaling pathway
As RAMH did not alter the growth of normal cholangiocytes, we evaluated the effect of RAMH for changes in the phosphorylation of the PKA → extracellular signal-regulated kinase 1/2 (ERK1/2) → ets-like gene-1 (Elk-1) signaling pathway only in BDL cholangiocytes. The expression levels of phosphorylated PKA → ERK1/2 → Elk-1 in cholangiocytes from NaCl and RAMH-treated BDL rats were evaluated by immunoblots. Membranes were stripped for determining protein expression of total PKA → ERK1/2 → Elk-1. Proteins were visualized using chemiluminescence (ECL Plus kit, Amersham Life Science). The intensity of the bands was determined by scanning video densitometry using the phospho-imager, Storm 860, Amersham Biosciences using the ImageQuant TLV 2003.02.
In Vitro Studies
To determine if the effects of RAMH on cholangiocyte proliferation, cAMP levels and the phosphorylation of cAMP-dependent PKA → ERK1/2 → Elk-1 are due to a direct interaction of RAMH with H3R on cholangiocytes (rather than an indirect action), purified cholangiocytes from 1 week BDL rats were treated in vitro with 0.2% BSA (basal) or RAMH (10 μM). Cholangiocyte proliferation was evaluated by PCNA protein expression by immunoblotting in cholangiocytes stimulated at 37°C for 3 h with 0.2% BSA (basal) or RAMH (10 μM). The amount of protein loaded was normalized against β-actin.35 Proteins (10 μg) were visualized using chemiluminescence (ECL Plus kit, Amersham Life Science). The intensity of the bands was determined by scanning video densitometry using the phospho-imager, Storm 860, Amersham Biosciences using the ImageQuant TLV 2003.02.
Following incubation at 37°C for 1 h, intracellular cAMP levels (a key player in the regulation of cholangiocyte hyperplasia)1, 2, 3, 5 were determined in cells treated at room temperature for 5 min38, 39 with (i) 0.2% BSA or (ii) RAMH (10 μM) in the absence or presence of pertussis toxin (PTX) (1 μM).40 To determine that RAMH has no effect on the Gαo activated signaling pathway (phospholipase C/IP3/Ca2+/PKCα-dependent pathway),41, 42 we measured intracellular IP3 levels in cholangiocytes stimulated at room temperature for 10 min43 with (i) 0.2% BSA or (ii) RAMH (10 μM). Intracellular cAMP and IP3 levels were determined by RIA (Amersham) according to directions supplied by the vendor.
We evaluated, by immunoblots, the effects of RAMH on the phosphorylation of PKA → ERK1/2 → Elk-1 in protein (10 μg) from whole-cell lysate from cholangiocytes stimulated with (i) 0.2% BSA or (ii) RAMH (10 μM) for 90 min at 37°C. After stripping, immunoblots were normalized with total amounts from each protein. Proteins (10 μg) were visualized using chemiluminescence (ECL Plus kit, Amersham Life Science). The intensity of the bands was determined by scanning video densitometry using the phospho-imager, Storm 860, Amersham Biosciences using the ImageQuant TLV 2003.02.
Statistical Analysis
All data are expressed as mean±s.e.m. The differences between groups were analyzed by Student's t-test when two groups were analyzed, or analysis of variance (ANOVA) if more than two groups were analyzed. A P-value <0.05 was used to indicate statistically significant differences.
Results
Cholangiocytes Express H3 Histamine Receptors
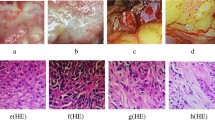
We performed immunohistochemistry (Figure 1) and immunofluorescence (Figure 2) for H3R in liver sections from normal and BDL rats and present cytoplasmic and membranous staining in cholangiocytes. By immunofluorescence, H3R immunoreactivity was colocalized with the expression of CK-19 (as a marker of cholangiocytes)39 (Figure 2). H3R were also expressed by hepatocytes from normal and BDL rats (Figures 1 and 2). No immunohistochemical or immunofluorescent reaction was observed when liver sections were incubated with non-immune serum (Figures 1 and 2). By immunofluorescence, we have shown that smears of isolated cholangiocytes from both normal and BDL rats express H3R (Figure 3a). By real-time PCR, we found that: (i) normal cholangiocytes express H3R mRNA (Figure 3b) and (ii) the expression of H3R mRNA significantly increased in cholangiocytes from BDL rats (Figure 3b).
Immunohistochemistry for H3R in paraffin-embedded liver sections from normal and 1-week BDL rats. By immunohistochemistry (scale bar=50 μm), there was cytoplasmic and membranous staining for H3R in cholangiocytes from normal and BDL rats. H3R were also expressed by hepatocytes from normal and BDL rats. No immunohistochemical reaction was observed when normal or BDL liver sections were incubated with non-immune serum.
Immunofluorescence for H3R in frozen liver sections from normal and 1 week BDL rats. By immunofluorescence in liver sections, there was cytoplasmic and membranous staining (arrows) for H3R in cholangiocytes from normal and BDL rats. By immunofluorescence, H3R immunoreactivity (red) was colocalized with CK-19 immunoreactivity (green; indicated by arrows) demonstrating cholangiocyte expression (scale bar=20 μm); sections were counterstained with DAPI. H3R were also expressed by hepatocytes from normal and BDL rats. No immunofluorescent reaction was observed when normal or BDL liver sections were incubated with non-immune serum.
Immunofluorescence (a, top panel) for H3R in cytospin smears of isolated cholangiocytes, and real-time PCR (b, bottom panel) for H3R mRNA in cholangiocyte RNA (0.75 μg) from normal and 1 week BDL rats. By immunofluorescence (a, top panel), purified cholangiocytes from both normal and BDL rats express H3R. Original magnification, × 40. By real-time PCR (b, bottom panel), we found that (i) normal cholangiocytes express H3R mRNA (expressed as ratio to GAPDH mRNA); and (ii) the relative expression of H3R mRNA (expressed as ratio to GAPDH mRNA) significantly increased in cholangiocytes from BDL rats. Data are mean±s.e.m. of three experiments. *P<0.05 vs relative expression of H3R mRNA of normal cholangiocytes.
In Vivo Studies
Evaluation of liver, body weight and liver to body weight ratio, and histamine, transaminase and bilirubin serum levels, necrosis, lobular damage and cholangiocyte apoptosis
There were no significant changes in the body weight of BDL rats treated with NaCl or RAMH for 1 week (Table 1). Consistent with the concept that RAMH decreases cholangiocyte proliferation, liver and liver to body weight ratio (an index of liver growth including cholangiocytes)27 decreased in BDL rats treated with RAMH compared to BDL rats treated with NaCl (Table 1). In BDL rats treated with RAMH, there was a decrease in the serum levels of bilirubin and AST (but not ALT) compared to BDL rats treated with NaCl (Table 1). Histamine serum levels of normal rats (36.2±4.2 ng/ml; n=7) were similar to those shown in previous studies44 and increased following BDL (50.7±3.6; n=7; P<0.05 vs histamine serum levels of normal rats). There were no significant changes in necrosis and apoptosis in liver sections from the selected groups of animals (Table 2). Both RAMH and histamine decrease the degree of lobular damage compared to BDL rats treated with NaCl (Table 2); no differences in lobular damage were observed between BDL rats treated with histamine plus thioperamide maleate or thioperamide maleate alone (Table 2).
Chronic in vivo administration of RAMH decreases cholangiocyte proliferation
In BDL rats, chronic RAMH administration decreased the number of PCNA-positive cholangiocytes in liver sections compared to liver sections from rats receiving NaCl (Figure 4). Similarly, there was a significant decrease in the number of CK-19-positive cholangiocytes (Figure 5) and γ-GT-positive ducts (Figure 6) in liver sections compared to liver sections from NaCl-treated BDL rats. Similar to RAMH, the administration of histamine to BDL rats significantly decreased the number of PCNA- and CK-19-positive cholangiocytes (Figures 4 and 5) and γ-GT-positive ducts (Figure 6) in liver sections compared to liver sections from BDL rats treated with NaCl; however, the decrease in cholangiocyte growth (by histamine administration alone) was smaller than that observed in BDL rats treated with RAMH (Figures 4, 5 and 6). Consistent with the concept that H3R regulate cholangiocyte growth of BDL rats, histamine inhibition of cholangiocyte growth was partly blocked by thioperamide maleate (Figures 4, 5 and 6); however, in the BDL rats treated with histamine+thioperamide maleate, cholangiocyte growth was still significantly lower than that of BDL rats (Figures 4, 5 and 6). In BDL rats treated with thioperamide maleate, cholangiocyte proliferation and ductal hyperplasia was slightly higher (although not significant) than that of BDL rats (Figures 4, 5 and 6). PCNA protein expression was also decreased in cholangiocytes purified from BDL rats treated with RAMH compared to cholangiocytes from NaCl-treated BDL rats (Figure 7a). Chronic administration of RAMH to normal rats had no effect on the number of PCNA- or CK-19-positive cholangiocytes or γ-GT-positive ducts compared to normal rats receiving NaCl (not shown).
Measurement of the number of PCNA-positive cholangiocytes in liver sections from rats that (immediately after BDL) were treated with NaCl, RAMH, thioperamide maleate (H3R antagonist) or histamine in the absence or presence of thioperamide maleate for 1 week. In BDL rats, chronic RAMH administration induced a decrease in the number of PCNA-positive (see arrows) cholangiocytes compared to NaCl-treated rats. Administration of histamine to BDL rats significantly decreased the number of PCNA-positive cholangiocytes compared to BDL rats treated with NaCl; however, the decrease in the number of PCNA-positive cholangiocytes (by histamine administration alone) was less than that observed in BDL rats treated with RAMH (arrows). Histamine inhibition of the number of PCNA-positive cholangiocytes was partly blocked by thioperamide maleate; however, in the BDL rats treated with histamine+thioperamide maleate, the number of PCNA-positive cholangiocytes was still significantly lower than that of BDL rats treated with NaCl. In BDL rats treated with thioperamide maleate, the number of PCNA-positive cholangiocytes was slightly higher (although not significant) than that of BDL rats. Data are mean±s.e.m. of five cumulative values from 10 randomly selected portal areas. *P<0.05 vs corresponding value from BDL rats treated with NaCl. #P<0.05 vs corresponding value from BDL rats treated with RAMH. Original magnification, × 20.
Measurement of the number of CK-19-positive cholangiocytes in liver sections from rats (that immediately after BDL) were treated with NaCl, RAMH, thioperamide maleate (H3R antagonist) or histamine in the absence or presence of thioperamide maleate for 1 week. In BDL rats, chronic RAMH administration induced a decrease in the number of CK-19-positive (see arrows) cholangiocytes compared to NaCl-treated rats. Administration of histamine to BDL rats significantly decreased the number of CK-19-positive cholangiocytes compared to BDL rats treated with NaCl; however, the decrease in the number of CK-19-positive cholangiocytes (by histamine administration alone) was less than that observed in BDL rats treated with RAMH (arrows). Histamine inhibition of the number of CK-19-positive cholangiocytes was partly blocked by thioperamide maleate; however, in the BDL rats treated with histamine+thioperamide maleate, the number of CK-19-positive cholangiocytes was still significantly lower than that of BDL rats treated with NaCl. In BDL rats treated with thioperamide maleate, the number of CK-19-positive cholangiocytes was slightly higher (although not significant) than that of BDL rats. Data are mean±s.e.m. of five cumulative values from 10 randomly selected portal areas. *P<0.05 vs corresponding value from BDL rats treated with NaCl. #P<0.05 vs corresponding value from BDL rats treated with RAMH. Original magnification, × 20.
Measurement of the number of γ-GT-positive ducts in liver sections from rats that (immediately after BDL) were treated with NaCl, RAMH, thioperamide maleate (H3R antagonist) or histamine in the absence or presence of thioperamide maleate for 1 week. In BDL rats, chronic RAMH administration induced a decrease in the number of γ-GT-positive ducts compared to NaCl-treated rats. Administration of histamine to BDL rats significantly decreased the number of γ-GT-positive ducts compared to BDL rats treated with NaCl; however, the decrease in the number of γ-GT-positive ducts (by histamine administration alone) was less than that observed in BDL rats treated with RAMH (arrows). Histamine inhibition of the number of γ-GT-positive ducts was partly blocked by thioperamide maleate; however, in the BDL rats treated with histamine+thioperamide maleate, the number of γ-GT-positive ducts was still significantly lower than that of BDL rats treated with NaCl. In BDL rats treated with thioperamide maleate, the number of γ-GT-positive ducts was slightly higher (although not significant) than that of BDL rats. Data are mean±s.e.m. of 16 cumulative values from 10 randomly selected portal areas. *P<0.05 vs corresponding value from BDL rats treated with NaCl. #P<0.05 vs corresponding value from BDL rats treated with RAMH.
(a, left panel) Measurement of PCNA protein expression in purified cholangiocytes from rats that (immediately after BDL) were treated with NaCl or RAMH for 1 week. PCNA protein expression was decreased in cholangiocytes from BDL rats treated with RAMH compared to cholangiocytes from NaCl-treated rats. Data are mean±s.e.m. of five experiments. *P<0.05 vs corresponding value from BDL rats treated with NaCl. (b, right panel) Measurement of the phosphorylation of PKA in cholangiocytes from rats that (immediately after BDL) were treated with NaCl or RAMH for 1 week. Chronic in vivo administration of RAMH to BDL rats induced a decrease in the phosphorylation of PKA (expressed as ratio to total PKA protein expression) in purified cholangiocytes compared to cholangiocytes from BDL rats treated with NaCl. Data are mean±s.e.m. of three experiments. *P<0.05 vs corresponding value from BDL rats treated with NaCl.
Consistent with the concept that decreased cholangiocyte proliferation is associated with reduced cAMP levels (a key regulator of cholangiocyte proliferation),1, 2, 3, 5 in vivo treatment of BDL rats with RAMH significantly (P<0.05) decreased intracellular cAMP levels (82.97±5.50 fmol/1 × 105 cells, n=7) of purified cholangiocytes compared to cholangiocyte cAMP levels from NaCl-treated BDL rats (111.10±8.57 fmol/1 × 105 cells, n=7). Administration of RAMH to normal rats did not alter cAMP levels of cholangiocytes compared to cholangiocytes from normal rats treated with NaCl (not shown).
Effect of chronic in vivo administration of RAMH on the phosphorylation of the cAMP-dependent PKA → ERK1/2 → Elk-1 signaling pathway
Administration of RAMH to BDL rats induced a decrease in the phosphorylation of PKA (expressed as ratio to total PKA protein expression) in purified cholangiocytes compared to cholangiocytes from BDL rats treated with NaCl (Figure 7b). ERK1/2 phosphorylation (expressed as ratio to total ERK1/2 protein expression) was significantly decreased in cholangiocytes from BDL+RAMH-treated animals compared to cholangiocytes from BDL rats treated with NaCl (Figure 8). Chronic administration of RAMH to BDL decreased the phosphorylation of Elk-1 (expressed as ratio to total Elk-1 protein expression) in cholangiocytes compared to cholangiocytes from NaCl-treated rats (Figure 9a).
ERK1/2 phosphorylation (expressed as ratio to total ERK1/2 protein expression) was significantly decreased in cholangiocytes from BDL+RAMH-treated animals compared to cholangiocytes from BDL rats treated with NaCl. Data are mean±s.e.m. of three experiments. *P<0.05 vs corresponding value from BDL rats treated with NaCl.
(a) Chronic administration of RAMH to BDL rats decreased the phosphorylation of Elk-1 (expressed as ratio to total Elk-1 protein expression) in cholangiocytes compared to cholangiocytes from NaCl treated rats. Data are mean±s.e.m. of three experiments. *P<0.05 vs corresponding value from BDL rats treated with NaCl. (b) Measurement of PCNA protein expression in purified BDL cholangiocytes treated in vitro with 0.2% BSA (basal) or RAMH (10 μM) with 0.2% BSA for 3 h at 37°C. In vitro stimulation of purified BDL cholangiocytes with RAMH induced a significant decrease in PCNA protein expression compared to cholangiocytes treated with 0.2% BSA. Data are mean±s.e.m. of eight experiments. *P<0.05 vs corresponding basal value.
In Vitro Studies
Effects of RAMH on cholangiocyte proliferation and cAMP and IP3 levels
Parallel to the in vivo studies, in vitro stimulation of purified BDL cholangiocytes with RAMH (10 μM) induced a significant decrease in PCNA protein expression compared to cholangiocytes treated with 0.2% BSA (Figure 9b).
Intracellular cAMP levels were decreased in BDL cholangiocytes treated in vitro with RAMH compared to cAMP levels of cholangiocytes treated in vitro with 0.2% BSA (Figure 10). RAMH-induced inhibition of cAMP levels was blocked by in vitro pretreatment of BDL cholangiocytes with the G-protein inhibitor, PTX.40 PTX alone did not alter cAMP levels of BDL cholangiocytes (Figure 10). In vitro stimulation with RAMH did not change intracellular IP3 levels of BDL cholangiocytes compared to cholangiocytes treated with BSA (data not shown), thus demonstrating that IP3 is not involved in H3R inhibition of cholangiocyte growth.
Measurement of cAMP levels in purified BDL cholangiocytes stimulated at room temperature for 5 min with 0.2% BSA (basal) or RAMH (10 μM) in the absence or presence of PTX (1 μM). RAMH-induced inhibition of cAMP levels was blocked, in vitro, by pretreatment of BDL cholangiocytes with PTX. PTX alone did not change cAMP levels of BDL cholangiocytes. Data are mean±s.e.m. of six experiments. *P<0.05 vs corresponding basal value.
In vitro effect of RAMH on the phosphorylation of the cAMP-dependent PKA → ERK1/2 → Elk-1 signaling pathway
In vitro RAMH induced a decrease in PKA phosphorylation in purified BDL cholangiocytes compared to BDL cholangiocytes treated with BSA (Figure 11a). ERK1/2 (Figure 11b) and Elk-1 (Figure 11c) phosphorylation was significantly decreased in cholangiocytes treated with RAMH compared to purified BDL cholangiocytes treated with BSA.
Measurement of the phosphorylation of (a) PKA, (b) ERK1/2 and (c) Elk-1 in purified BDL cholangiocytes treated in vitro with 0.2% BSA (basal) or PAMH (10 μM). (a) In vitro, RAMH induced a decrease in PKA phosphorylation in purified BDL cholangiocytes compared to BDL cholangiocytes treated with BSA. Data are mean±s.e.m. of three experiments. *P<0.05 vs corresponding basal value. (b) RAMH decreased the phosphorylation of ERK1/2 (b) and Elk-1 (c) compared to cholangiocytes treated with BSA. Data are mean±s.e.m. of three experiments. *P<0.05 vs corresponding basal value.
Discussion
The findings of our study demonstrate that the activation of the specific H3R on cholangiocytes inhibits biliary proliferation induced by BDL.27 Similar to RAMH, the administration of histamine to BDL rats significantly decreased cholangiocyte proliferation compared to BDL rats treated with NaCl; however, the decrease in cholangiocyte growth (by administration of histamine alone) was smaller than that observed in BDL rats treated with RAMH. Histamine inhibition of cholangiocyte growth was partly blocked by thioperamide maleate. In BDL rats treated with thioperamide maleate, ductal hyperplasia was slightly higher (although not significant) than that observed in BDL rats treated with NaCl. In vitro, RAMH inhibited the proliferation of BDL cholangiocytes. The in vivo and in vitro RAMH-induced inhibition of cholangiocyte growth was mediated by a cAMP-dependent decrease of the phosphorylation of PKA → ERK1/2 → Elk-1.
The mechanism by which cholangiopathies develop and progress towards ductopenia is unclear.45 A major event to be considered is the impairment of the proliferative response of cholangiocytes, which involves apoptotic cell death.1, 45, 46 Apoptosis of cholangiocytes in the course of primary biliary cirrhosis (PBC) and primary sclerosing cholangitis (the two most common of the cholangiopathies)1, 45 has been associated with the local release of mediators by cells of the immune system.47, 48, 49 Indeed, some of those mediators like nitric oxide and cytokines have been shown to affect cholangiocyte biology.50 Furthermore, in chronic liver diseases including PBC there is increased number of mast cells,51 which causes a local increase of histamine.51 Moreover, histamine serum levels are increased in patients with chronic cholestatic liver diseases.52 Our findings are relevant to these cholangiopathies, as we have demonstrated that histamine, increased histamine serum levels and activation of H3R modulate the proliferative response of cholangiocytes to cholestasis.
BDL-induced cholangiocyte proliferation is characterized by increased intrahepatic ductal mass27 compared to normal rats. In our study, chronic in vivo administration of RAMH to BDL rats decreased the number of bile ducts compared to NaCl-treated BDL rats. In support of our findings, studies have shown that HR agonists regulate mitosis in other cell types.53, 54, 55 For example, RAMH stimulates cell proliferation and migration in rat oxyntic mucosa.55 Conversely, our present studies demonstrated that RAMH inhibits, both in vivo and in vitro, hyperplastic cholangiocyte proliferation of BDL rats. This difference between the inhibitory effects of RAMH observed in cholangiocytes and the stimulatory effect of this H3R agonist on rat oxyntic mucosa55 is likely due to the different cell target. In support of this concept, studies have shown that gastrin induces the growth of normal56 and neoplastic tissues,57 but inhibits the hyperplastic growth of BDL cholangiocytes2 and the neoplastic growth of biliary58 and pancreatic59 cancers.
Histamine is known to interact with four receptor subtypes.14, 15 Thus, we performed a series of experiments to pinpoint the role of the H3R in histamine modulation of cholangiocyte proliferative response to cholestasis. We observed that the in vivo administration of RAMH to BDL rats decreased cholangiocyte growth to a higher extent compared to histamine. These results suggest that endogenous histamine also interacts with other HRs, exerting an opposite, pro-proliferative effect. In this regard, we have shown that the activation of H1R and H2R enhances normal cholangiocyte growth.60 The findings of our current study show that when BDL rats are administered with the H3R selective antagonist, thioperamide maleate, the increase of bile duct mass in reaction to cholestasis is higher (although not significant) than BDL rats. As H3R are also expressed by hepatocytes, there may indeed be some interactions between cholangiocytes and hepatocytes to modulate the in vivo effects of H3R on cholangiocyte proliferation. However, because we have shown that the inhibition of RAMH on cholangiocyte proliferation occurs in vitro, using a cholangiocyte isolation procedure that excludes hepatocytes, we demonstrated that the in vivo inhibition of RAMH on cholangiocyte growth is a direct effect rather than an effect mediated by hepatocytes.
We evaluated the effect of chronic administration of RAMH on lobular damage, cholangiocyte apoptosis and bilirubin and transaminase serum levels and showed that RAMH ameliorates lobular damage and decreases the serum levels of bilirubin and AST compared to BDL rats treated with NaCl. Supporting our present study, earlier studies have shown that the pro-drug of RAMH reduced the necrotic changes induced by CCl4 treatment and inhibited the increase of plasma AST and ALT activities.61 Similarly, pretreatment with histamine ameliorated the D-galactosamine/lipopolysaccharide-induced necrotic and apoptotic changes in the hepatocytes and inhibited the elevation of serum AST levels.62
We next: (i) performed in vitro studies to demonstrate that RAMH inhibits cholangiocyte proliferation by directly interacting with H3R; and (ii) evaluated the intracellular mechanisms by demonstrating that RAMH-inhibition of cholangiocyte growth is associated with changes in the cAMP-dependent PKA/ERK1/2/Elk-1 pathway, which regulates the mitosis of a number of cells including cholangiocytes.5, 10, 63 cAMP accumulation is linked to Gαs stimulation inducing increased cell proliferation.64 In contrast, when the Gαi protein is activated there is a negative regulation of cAMP that leads to decreased proliferation via downregulation of PKA and the mitogen-activated protein kinase (MAPK) pathway.64 Previous studies have shown that increased cholangiocyte growth is closely coupled with enhanced cAMP levels,5, 39, 65 whereas reduced cholangiocyte proliferation is associated with decreased cAMP levels.66 Maintenance of cAMP levels by the administration of forskolin or β1- and β2-adrenergic receptor agonists prevents the stimulatory effects of cholinergic or adrenergic denervation, respectively, on cholangiocyte apoptosis.34, 65 Furthermore, upregulation of the cAMP system (by chronic forskolin administration) alone is sufficient to induce cholangiocyte hyperplasia in normal rats, similar to the BDL rat model.5 Our study shows that chronic administration of the H3R agonist, RAMH to BDL rats induced a decrease in cholangiocyte cAMP levels compared to cAMP levels of cholangiocytes from BDL rats treated with NaCl. Similarly, in vitro, RAMH induced a decrease in intracellular cAMP levels that was abolished by pretreatment with the general Gi-protein inhibitor, PTX,67 demonstrating a Gαi, PKA-dependent inhibition of adenylyl cyclase and cAMP levels. In support of this concept, recent studies have shown that: (i) H3 receptor agonists decrease forskolin-stimulated cAMP levels;21 and (ii) stimulation of [35S]GTPγ[S] binding through H3 receptor agonists in cerebral cortical membranes is prevented by PTX.68
cAMP-dependent PKA regulation of cell growth involves signaling by the specific MAP kinase, ERK1/2.69 This effect, however, is determined by the type of cells involved and can entail either positive or negative regulation. Histamine has been shown to increase ERK1/2 MAPkinase activity in vascular smooth muscle70 and, specifically, the H1R also induces an increase in phosphorylation of ERK1/2 in bovine adrenal chromaffin cells.71 In our study, involvement of cAMP/PKA in the anti-proliferative effects of histamine (via the H3R agonist) is further supported by our findings that RAMH decreases active site phosphorylation for ERK1/2. To further elucidate the mechanisms regulating the inhibition of proliferation by RAMH, we evaluated the role of Elk-1, a member of the ETS-domain family of transcription factors.72 Studies in human glioblastoma cells show: (i) protein kinase B inhibits Elk-1 expression by downregulation of the MEK → ERK pathway;73 and (ii) activation and nuclear translocation of ERK1/2 induces activation of Elk-1.74 Parallel with these findings,73, 74 we demonstrated that the reduction of ERK1/2 phosphorylation by RAMH results in decreased Elk-1 phosphorylation.
In summary, we propose that in cholestatic liver diseases (eg, after BDL) cholangiocyte proliferation is regulated by a fine balance between the stimulatory (by activation of H1R and H2R) and inhibitory (by activation of H3R and H4R) effects of endogenous histamine. This study indicates that the excessive proliferation of cholangiocytes in the course of cholestatic liver diseases could be counterbalanced by the selective activation of H3R, which mediate inhibition of intrahepatic ductal mass.
References
Alvaro D, Mancino MG, Glaser S, et al. Proliferating cholangiocytes: a neuroendocrine compartment in the diseased liver. Gastroenterology 2006;132:415–431.
LeSage G, Glaser S, Alpini G . Regulation of cholangiocyte proliferation. Liver 2001;21:73–80.
Alpini G, Prall RT, LaRusso NF . The pathobiology of biliary epithelia. In: Arias IM, Boyer JL, Chisari FV, Fausto N, Jakoby W, Schachter D, Shafritz DA (eds). The Liver, Biology and Pathobiology, 4th edn. Lippincott Williams & Wilkins: Philadelphia, PA, 2001, pp 421–435.
Polimeno L, Azzarone A, Zeng QH, et al. Cell proliferation and oncogene expression after bile duct ligation in the rat: evidence of a specific growth effect on bile duct cells. Hepatology 1995;21:1070–1078.
Francis H, Glaser S, Ueno Y, et al. cAMP stimulates the secretory and proliferative capacity of the rat intrahepatic biliary epithelium through changes in the PKA/Src/MEK/ERK1/2 pathway. J Hepatol 2004;41:528–537.
Tracy Jr TF, Tector AJ, Goerke ME, et al. Somatostatin analogue (octreotide) inhibits bile duct epithelial cell proliferation and fibrosis after extrahepatic biliary obstruction. Am J Pathol 1993;143:1574–1578.
Tan CK, Podila PV, Taylor JE, et al. Human cholangiocarcinomas express somatostatin receptors and respond to somatostatin with growth inhibition. Gastroenterology 1995;108:1908–1916.
Hulzebos CV, Voshol PJ, Wolters H, et al. Bile duct proliferation associated with bile salt-induced hypercholeresis in Mdr2 P-glycoprotein-deficient mice. Liver Int 2005;25:604–612.
Barbaro B, Glaser S, Francis H, et al. Nerve regulation of cholangiocyte functions. In: Alpini G, Alvaro D, LeSage G, Marzioni M, LaRusso NF (eds). Pathophysiology of the Bile Duct System. Landes Biosciences: Georgetown, TX, 2004, pp 199–209.
Gaudio E, Barbaro B, Alvaro D, et al. Vascular endothelial growth factor stimulates rat cholangiocyte proliferation via an autocrine mechanism. Gastroenterology 2006;130:1270–1282.
Parsons ME, Ganellin CR . Histamine and its receptors. Br J Pharmacol 2006;147(Suppl 1):S127–S135.
Hou YF, Zhou YC, Zheng XX, et al. Modulation of expression and function of Toll-like receptor 3 in A549 and H292 cells by histamine. Mol Immunol 2006;43:1982–1992.
Jancso G, Santha P, Horvath V, et al. Inhibitory neurogenic modulation of histamine-induced cutaneous plasma extravasation in the pigeon. Regul Pept 2000;95:75–80.
Nguyen T, Shapiro DA, George SR, et al. Discovery of a novel member of the histamine receptor family. Mol Pharmacol 2001;59:427–433.
Repka-Ramirez MS . New concepts of histamine receptors and actions. Curr Allergy Asthma Rep 2003;3:227–231.
Dickenson JM . Stimulation of protein kinase B and p70 S6 Kinase by the histamine H1 receptor in DDT1MF-2 smooth muscle cells. Br J Pharmacol 2002;135:1967–1976.
Mitsuhashi M, Mitsuhashi T, Payan D . Multiple signaling pathways of histamine H2 receptors (identification of an H2 receptor- dependent Ca2+ mobilization pathway in human HL-60 promyelocytic leukemia cells). J Biol Chem 1989;264:18356–18362.
Schwartz JC, Arrang JM, Garbarg M, et al. Histaminergic transmission in the mammalian brain. Physiol Rev 1991;71:1–51.
Jin C, Lintunen M, Panula P . Histamine H(1) and H(3) receptors in the rat thalamus and their modulation after systemic kainic acid administration. Exp Neurol 2005;194:43–56.
Lovenberg TW, Pyati J, Chang H, et al. Cloning of rat histamine H(3) receptor reveals distinct species pharmacological profiles. J Pharmacol Exp Ther 2000;293:771–778.
Lovenberg TW, Roland BL, Wilson SJ, et al. Cloning and functional expression of the human histamine H3 receptor. Mol Pharmacol 1999;55:1101–1107.
Liu C, Ma X, Jiang X, et al. Cloning and pharmacological characterization of a fourth histamine receptor (H(4)) expressed in bone marrow. Mol Pharmacol 2001;59:420–426.
Lee JJ, Parsons ME . Signaling mechanisms coupled to presynaptic A(1)- and H(3)-receptors in the inhibition of cholinergic contractile responses of the guinea pig ileum. J Pharmacol Exp Ther 2000;295:607–613.
Gantner F, Sakai K, Tusche MW, et al. Histamine h(4) and h(2) receptors control histamine-induced interleukin-16 release from human CD8(+) T cells. J Pharmacol Exp Ther 2002;303:300–307.
Adachi N, Liu K, Motoki A, et al. Suppression of ischemia/reperfusion liver injury by histamine H4 receptor stimulation in rats. Eur J Pharmacol 2006;544:181–187.
Nowak P, Dabrowska J, Bortel A, et al. Histamine H(3) receptor agonist- and antagonist-evoked vacuous chewing movements in 6-OHDA-lesioned rats occurs in an absence of change in microdialysate dopamine levels. Eur J Pharmacol 2006;552:46–54.
Alpini G, Lenzi R, Sarkozi L, et al. Biliary physiology in rats with bile ductular cell hyperplasia. Evidence for a secretory function of proliferated bile ductules. J Clin Invest 1988;81:569–578.
Oishi R, Itoh Y, Nishibori M, et al. Effects of the histamine H3-agonist (R)-alpha-methylhistamine and the antagonist thioperamide on histamine metabolism in the mouse and rat brain. J Neurochem 1989;52:1388–1392.
Karavodin L, Jensen R, Sarno M, et al. Toxicology and toxicokinetics of acute and subchronic administration of histamine dihydrochloride in rats. Drug Chem Toxicol 2003;26:35–49.
Ishii M, Vroman B, LaRusso NF . Isolation and morphological characterization of bile duct epithelial cells from normal rat liver. Gastroenterology 1989;97:1236–1247.
Rutenburg AM, Kim H, Fischbein JW, et al. Histochemical and ultrastructural demonstration of γ-glutamyl transpeptidase activity. J Histochem Cytochem 1969;17:517–526.
Alpini G, Glaser S, Ueno Y, et al. Heterogeneity of the proliferative capacity of rat cholangiocytes after bile duct ligation. Am J Physiol Gastrointest Liver Physiol 1998;274:G767–G775.
LeSage G, Glaser S, Ueno Y, et al. Regression of cholangiocyte proliferation after cessation of ANIT feeding is coupled with increased apoptosis. Am J Physiol Gastrointest Liver Physiol 2001;281:G182–G190.
Glaser S, Alvaro D, Francis H, et al. Adrenergic receptor agonists prevent bile duct injury induced by adrenergic denervation by increased cAMP levels and activation of Akt. Am J Physiol Gastrointest Liver Physiol 2006;290:G813–G826.
Alpini G, Ueno Y, Glaser S, et al. Bile acid feeding increased proliferative activity and apical bile acid transporter expression in both small and large rat cholangiocytes. Hepatology 2001;34:868–876.
Sand TE, Thoresen GH, Refsnes M, et al. Growth-regulatory effects of glucagon, insulin, and epidermal growth factor in cultured hepatocytes. Temporal aspects and evidence for bidirectional control by cyclic AMP. Dig Dis Sci 1992;37:84–92.
Tsujii H, Okamoto Y, Kikuchi E, et al. Prostaglandin E2 and rat liver regeneration. Gastroenterology 1993;105:495–499.
Kato A, Gores GJ, LaRusso NF . Secretin stimulates exocytosis in isolated bile duct epithelial cells by a cyclic AMP-mediated mechanism. J Biol Chem 1992;267:15523–15529.
LeSage G, Glaser S, Gubba S, et al. Regrowth of the rat biliary tree after 70% partial hepatectomy is coupled to increased secretin-induced ductal bile secretion. Gastroenterology 1996;111:1633–1644.
Walcher D, Aleksic M, Jerg V, et al. C-peptide induces chemotaxis of human CD4-positive cells: involvement of pertussis toxin-sensitive G-proteins and phosphoinositide 3-kinase. Diabetes 2004;53:1664–1670.
Gomez-Ramirez J, Ortiz J, Blanco I . Presynaptic H3 autoreceptors modulate histamine synthesis through cAMP pathway. Mol Pharmacol 2002;61:239–245.
Endou M, Poli E, Levi R . Histamine H3-receptor signaling in the heart: possible involvement of Gi/Go proteins and N-type Ca++ channels. J Pharmacol Exp Ther 1994;269:221–229.
LeSage G, Alvaro D, Glaser S, et al. Alpha-1 adrenergic receptor agonists modulate ductal secretion of BDL rats via Ca(2+)- and PKC-dependent stimulation of cAMP. Hepatology 2004;40:1116–1127.
Rodgers K, Xiong S . Effect of acute administration of malathion by oral and dermal routes on serum histamine levels. Int J Immunopharmacol 1997;19:437–441.
Lazaridis KN, Strazzabosco M, LaRusso NF . The cholangiopathies: disorders of biliary epithelia. Gastroenterology 2004;127:1565–1577.
Alvaro D, Invernizzi P, Onori P, et al. Estrogen receptors in cholangiocytes and the progression of primary biliary cirrhosis. J Hepatol 2004;41:905–912.
Haruta I, Hashimoto E, Kato Y, et al. Intrahepatic biliary epithelial cell damage and inflammation in portal tract in association with chronic colitis-harboring TCRalpha(−/−) mice. Hepatol Res 2006;34:3–8.
Sasaki M, Ansari AA, Nakanuma Y, et al. The immunopathology of primary biliary cirrhosis: thoughts for the millennium. Arch Immunol Ther Exp (Warsz) 2000;48:1–10.
Tinmouth J, Lee M, Wanless IR, et al. Apoptosis of biliary epithelial cells in primary biliary cirrhosis and primary sclerosing cholangitis. Liver 2002;22:228–234.
Spirli C, Nathanson MH, Fiorotto R, et al. Proinflammatory cytokines inhibit secretion in rat bile duct epithelium. Gastroenterology 2001;121:156–169.
Farrell DJ, Hines JE, Walls AF, et al. Intrahepatic mast cells in chronic liver diseases. Hepatology 1995;22:1175–1181.
Gittlen SD, Schulman ES, Maddrey WC . Raised histamine concentrations in chronic cholestatic liver disease. Gut 1990;31:96–99.
Wang LD, Hoeltzel M, Butler K, et al. Activation of the human histamine H2 receptor is linked to cell proliferation and c-fos gene transcription. Am J Physiol Cell Physiol 1997;273:C2037–C2045.
Rizell M, Hellstrand K, Lindner P, et al. Monotherapy with histamine dihydrochloride suppresses in vivo growth of a rat sarcoma in liver and subcutis. Anticancer Res 2002;22:1943–1948.
Morini G, Grandi D, Schunack W . Ligands for histamine H(3) receptors modulate cell proliferation and migration in rat oxyntic mucosa. Br J Pharmacol 2002;137:237–244.
Quintero E, Ohning GV, Del Rivero M, et al. Gastrin mediates the increase in gastric cell growth in uremic rats. Am J Physiol Gastrointest Liver Physiol 1995;268:G586–G591.
Song DH, Rana B, Wolfe JR, et al. Gastrin-induced gastric adenocarcinoma growth is mediated through cyclin D1. Am J Physiol Gastrointest Liver Physiol 2003;285:G217–G222.
Kanno N, Glaser S, Chowdhury U, et al. Gastrin inhibits cholangiocarcinoma growth through increased apoptosis by activation of Ca2+-dependent protein kinase C-alpha. J Hepatol 2001;34:284–291.
Detjen K, Fenrich MC, Logsdon CD . Transfected cholecystokinin receptors mediate growth inhibitory effects on human pancreatic cancer cell lines. Gastroenterology 1997;112:952–959.
Francis H, Taffetani S, Glaser S, et al. Histamine stimulates cholangiocyte proliferation through transduction pathways involving the H1 and H2 histamine receptor subtypes. Gastroenterology 2004;126:AT925.
Valcheva-Kuzmanova SV, Popova PB, Krasnaliev IJ, et al. Protective effect of BP 2–94, a histamine H3-receptor agonist prodrug, in a model of carbon tetrachloride-induced hepatotoxicity in rats. Folia Med (Plovdiv) 2004;46:36–41.
Masaki T, Chiba S, Tatsukawa H, et al. The role of histamine H1 receptor and H2 receptor in LPS-induced liver injury. FASEB J 2005;19:1245–1252.
Davis S, Vanhoutte P, Pages C, et al. The MAPK/ERK cascade targets both Elk-1 and cAMP response element-binding protein to control long-term potentiation-dependent gene expression in the dentate gyrus in vivo. J Neurosci 2000;20:4563–4572.
Levistre R, Berguerand M, Bereziat G, et al. The cross-regulation of Gi-protein by cholera toxin involves a phosphorylation by protein kinase A. Biochem J 1995;306:765–769.
LeSage G, Alvaro D, Benedetti A, et al. Cholinergic system modulates growth, apoptosis, and secretion of cholangiocytes from bile duct-ligated rats. Gastroenterology 1999;117:191–199.
Glaser S, Benedetti A, Marucci L, et al. Gastrin inhibits cholangiocyte growth in bile duct-ligated rats by interaction with cholecystokinin-B/Gastrin receptors via D-myo-inositol 1,4,5-triphosphate-, Ca(2+)-, and protein kinase C alpha-dependent mechanisms. Hepatology 2000;32:17–25.
Mittra S, Bourreau JP . Gs and Gi coupling of adrenomedullin in adult rat ventricular myocytes. Am J Physiol Heart Circ Physiol 2006;290:H1842–H1847.
Clark EA, Hill SJ . Sensitivity of histamine H3 receptor agonist-stimulated [35S]GTP gamma[S] binding to pertussis toxin. Eur J Pharmacol 1996;296:223–225.
Stork PJ, Schmitt JM . Crosstalk between cAMP and MAP kinase signaling in the regulation of cell proliferation. Trends Cell Biol 2002;12:258–266.
Gorenne I, Su X, Moreland RS . Caldesmon phosphorylation is catalyzed by two kinases in permeabilized and intact vascular smooth muscle. J Cell Physiol 2004;198:461–469.
Cammarota M, Bevilaqua LR, Rostas JA, et al. Histamine activates tyrosine hydroxylase in bovine adrenal chromaffin cells through a pathway that involves ERK1/2 but not p38 or JNK. J Neurochem 2003;84:453–458.
Wiren KM, Toombs AR, Zhang XW . Androgen inhibition of MAP kinase pathway and Elk-1 activation in proliferating osteoblasts. J Mol Endocrinol 2004;32:209–226.
Galetic I, Maira SM, Andjelkovic M, et al. Negative regulation of ERK and Elk by protein kinase B modulates c-Fos transcription. J Biol Chem 2003;278:4416–4423.
Xu L, Fukumura D, Jain RK . Acidic extracellular pH induces vascular endothelial growth factor (VEGF) in human glioblastoma cells via ERK1/2 MAPK signaling pathway: mechanism of low pH-induced VEGF. J Biol Chem 2002;277:11368–11374.
Acknowledgements
We thank Glen Cryer, Division of Communication, Scott & White, for his assistance in editing the manuscript. The study was supported by a grant award from Scott & White Hospital to Heather Francis, the Dr Nicholas C Hightower Centennial Chair of Gastroenterology from Scott & White, the VA Research Scholar Award, a VA Merit Award and the NIH grant DK062975 to Dr Alpini and a grant award from Health and Labour Sciences Research Grants for the Research on Measures for Intractable Diseases (from the Ministry of Health, Labour and Welfare of Japan), from Grant-in-Aid for Scientific Research C (16590573) from JSPS to Dr Ueno and the MIUR Grant PRIN no. 2005067975_002 to Dr Alvaro.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Francis, H., Franchitto, A., Ueno, Y. et al. H3 histamine receptor agonist inhibits biliary growth of BDL rats by downregulation of the cAMP-dependent PKA/ERK1/2/ELK-1 pathway. Lab Invest 87, 473–487 (2007). https://doi.org/10.1038/labinvest.3700533
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.3700533
Keywords
This article is cited by
-
Microbiota transplantation reveals beneficial impact of berberine on hepatotoxicity by improving gut homeostasis
Science China Life Sciences (2018)
-
Isolation and characterization of hepatic mast cells from cholestatic rats
Laboratory Investigation (2016)
-
Histamine receptor expression in human renal tubules: a comparative pharmacological evaluation
Inflammation Research (2015)
-
H3 receptor renal expression in normal and diabetic rats
Inflammation Research (2015)
-
Inhibition of mast cell-derived histamine secretion by cromolyn sodium treatment decreases biliary hyperplasia in cholestatic rodents
Laboratory Investigation (2014)